Abstract
Acute Myeloid Leukemia (AML) with rearranged PICALM::MLLT10 is a rare and poorly characterized entity. Here, we describe a patient with this rearrangement, and compare this case to the literature. We observed a trend towards young age, male sex, extramedullary involvement (particularly mediastinal myelosarcoma), trisomy 4, trisomy 19 and aberrant CD7-expression. It was suggested that upregulation of DOT1l or BMI1 is a key effector for subsequent leukemogenesis. However, molecular data are not available for most published cases. Interestingly, two different EZH2-mutations were detected in our case, while generally being rare in AML, which is concordant with recent reports on the occurrence of EZH2mut in this AML subtype. As a synergistic effect of BMI1 and EZH2 has already been demonstrated in other neoplasms, we hypothesize that acquiring an EZH2 mutation might be a crucial proliferation advantage in PICALM::MLLT10 positive cells. This may explain the high percentage of EZH2 mutated cases in this entity, but also supports the hypothesis of BMI1-mediated leukemogenesis.
Similar content being viewed by others
Introduction
The PICALM::MLLT10 (also known as CALM::AF10) fusion transcript has first been discovered in the U-937 histiocytic lymphoma cell line [1, 2]. It is the product of a translocation of chromosomes 10 and 11 (t(10;11)(p12.3;q14.2)). MLLT10-rearranged acute myeloid leukemia (AML) is uncommon. It most frequently occurs as KMT2A::MLLT10-fusion, which one study estimates as the third most prevalent KMT2A-rearrangement, being present in 19% of KMT2A-rearranged AML [3]. In comparison, PICALM::MLLT10 rearranged AML is extremely rare, with the largest published cohort in the adult setting only including 18 cases [4, 5], and the largest pediatric cohort including 39 patients [6]. This is in contrast to MPAL, where the fusion seems more frequent [7], and to gamma-delta-T-cell acute lymphoblastic leukemia (ALL) where the fusion also occurs more frequently [8]. Given its low incidence in AML, the diagnosis can be challenging, as is evident in the case presented here.
It is not entirely clear how PICALM::MLLT10 leads to leukemogenesis. It has been shown that the interaction of the clathrin-binding-domain of PICALM and the OM-LZ region of MLLT10 is the relevant outcome of the fusion [9]. It has also been shown that several genes, including BMI1 posterior HOXA genes, and MEIS1 are overexpressed in PICALM::MLLT10-positive acute leukemias [10, 11]. However, there are two proposed downstream mechanisms. One focuses on the interaction of a nuclear export signal contained within PICALM and the DOT1L [9, 12, 13]. This prevents nuclear export of the fusion transcript, and facilitates PICALM-dependent upregulation of HOXA-family genes (HOXA 5, 9, 10, MEIS1), which in turn blocks differentiation of hematopoietic stem cells (HSCs) [14]. The other hypothesis focuses on BMI1, which encodes a ring finger protein that is part of the Polycomb Repressive Complex 1 (PRC1). Interestingly, it is not upregulated in KMT2A-rearranged AML. The gene is located downstream of AF10. PRC1 stabilizes long-term silencing of regions targeted by Polycomb Repressive Complex 2 (PRC2), which represses multiple tumor suppressor genes (e.g., CDKN2A and CDKN2D). Thus, its upregulation is oncogenic. It has been shown that inhibition of BMI1 is capable of both inhibiting PICALM::MLLT10-driven leukemic transformation and impairing the growth of PICALM::MLLT10 rearranged AML in several models [15].
We conclude that the case report and literature review presented here will aid clinicians in recognizing this rare entity and understanding its disease biology.
Case report
A 30-year-old man presented to the Emergency Department of a local hospital 4 times in 11 days with increasing thoracic pain. Due to unspecific ST-elevations on ECG, pericarditis was diagnosed. He was repeatedly discharged with anti-inflammatory and analgesic drugs, until he returned with nausea, myalgias, fever, chills, and sweating. A computed tomography scan was performed (Fig. 1), which revealed a mediastinal mass of 6.5 × 4 × 7 cm, and putative pyelonephritis. The patient was admitted under the suspicion of sepsis. Laboratory studies were compatible with disseminated intravascular coagulation (DIC;Tc: 9 G/l, D-Dimer: >128.000 µg/l, PT: 21 s, Fibrinogen: 2.1 g/l). immune-thrombopenia (ITP) and paraneoplastic DIC were considered, and the patient was transferred to our academic hospital.
At our center, petechiae on abdomen and legs were noted, and the patient reported bleeding easily when brushing his teeth. Neither lymphadenopathy nor organomegalies were present. There was no palpable scrotal mass. An ultrasound of the urogenital tract did not reveal a germ cell tumor. Laboratory studies were notable for massive elevation of acute-phase markers (Table 1).
A blood smear revealed blasts which were morphologically judged to be of primarily lymphatic aspect with immature nucleus and multiple nucleoli. A left-shift of the myeloid lineage was noted. No fragmentocytes were observed. In contrast to the primary cytomorphologic aspect, immunophenotyping of the peripheral blood revealed a large population of myeloblasts (strongly positive for MPO, positive for CD15, CD33, CD34, CD38, CD71, CD105, and CD123), partially positive for CD117, HLA-DR, negative for CD13). A bone marrow biopsy confirmed the diagnosis of AML (FAB M1). The patient received all-trans retinoic acid and arsenic trioxide until PML::RARα-rearrangement was ruled out. Cytogenetics revealed t(10;11)(p12.3;q14.2). Interphase fluorescence in-situ hybridization (FISH) and myeloid gene panel (Illumina TSO500 panel) sequencing confirmed a PICALM::MLLT10 fusion transcript (variant allele frequency (VAF): 38%) and found two mutations in EZH2 (c.2069 G > A, p.R690H, VAF 36%, ClinVar: likely pathogenic; c.2084 C > T, p.S695L, VAF 36%, ClinVar: pathogenic/likely pathogenic), but no other mutations or rearrangements (65 genes and 688 rearrangements analyzed). Though not definitively deductible from our sequencing data, the presence of two separate EZH2mut could hint at a biallelic loss of function. Both EZH2 mutations we have detected are located in the SET-domain of EZH2. According to the Catalog of Somatic Mutations in Cancer (COSMIC) database, one of these mutations (p.S695L) has previously been described in AML, myelodysplastic neoplasm (MDS), ALL, all well as solid tumors, while the other (p.R690H) has been described in a number of hematologic tumors, including AML, MDS, myelofibrosis, Chronic myeloid leukemia, and ALL. Missense mutations in this region abrogate catalytic activity in vitro [16]. Both mutations in the SET-domain as well as homozygous aberrations of EZH2 show a trend towards worse survival in one large study [17]. Conventional cytogenetics revealed no aberration besides the reciprocal fusion, with t(10;11)(p12.3;q14.2) being detectable in 18/20 metaphases.
The patient then underwent intensive induction chemotherapy with cytarabine and idarubicin (“7 + 3” regimen). Bone marrow biopsy after two cycles showed complete morphological remission, as well as flow-cytometric and molecular measurable residual disease (MRD) negativity, and the remnant of the strongly regressive mediastinal mass was not 18-fluor-desoxy-glucose-avid on positron emission tomography (PET)-CT. We thus considered it most likely that the mass was a myelosarcoma of the present AML and refrained from a biopsy.
The patient then underwent allogeneic stem cell transplant from his matching sister after myeloablative conditioning with cyclophosphamide and busulfan. He received cyclosporine A (CyA) and methotrexate (MTX) as graft versus host disease (GVHD)-prophylaxis. Eleven months after allogeneic stem cell allogeneic transplant, molecular relapse became apparent with an increasing PICALM::MLLT10 fusion transcript. However, under salvage therapy with azacitidine and venetoclax (aza/ven), the fusion transcript disappeared below the limit of detection (VAF of 2%) again. Unfortunately, seven months after initiation of aza/ven an extramedullary relapse in the form of a progression of the previously described mediastinal mass occurred, while the bone marrow remained MRD negative. Video-assisted thoracoscopic surgery was performed to take a biopsy of the mass, which confirmed the presence of a myelosarcoma, the known PICALM::MLLT10 fusion and the EZH2-mutations. However, in addition mutations in BRAF (G469A; VAF 43%), NRAS (G12S; VAF 44%) and TP53 (L145R; VAF 57%) were detected in the mediastinal mass. Activating mutations in BRAF are rare in AML and are clearly associated with adverse outcomes [18, 19]. After subsequent radiation of the mediastinal mass (12 × 2 Gray), further extramedullary manifestations of the AML appeared in the patient’s pancreas, ribs, and skull. He underwent a second allogeneic stem cell transplant from the same donor (conditioning: Fludarabine and total body irradiation (8 Gray); GVHD-prophylaxis: CyA, MTX) five months after discontinuation of aza/ven. Subsequently, a maintenance therapy with the BRAF-Inhibitor darafenib and the MEK-Inhibitor trametinib was initiated. This therapy is the standard of care in malignant melanoma with activating BRAF-mutations [20]. In AML, BRAF-inhibition is not established, but case reports have also shown responses [21]. Unfortunately, the patient did not achieve a long-term remission and died four months after the second transplant.
Literature review
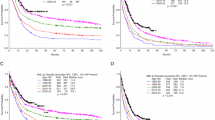
We searched PubMed for possible spellings of the translocation of interest (“PICALM-MLLT10”, “CALM-AF10”, “PICALM::MLLT10”, “CALM::AF10”) alone and in combination with “AML” or “Acute myeloid leukemia”. Papers including clinical characterizations of patients diagnosed as AML by the respective authors were included. Papers for which no English-language full-text was available were excluded. We identified 118 cases of PICALM::MLLT10 rearranged AML published in case reports or case series [4, 6, 22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44]. Relevant clinical, immunophenotypic and genetic characteristics of the reported cases are summarized in Table 2. The reported patients are typically younger than the average AML patient with a median age of 14 years at diagnosis (range 6-66). There is a trend towards male sex (71/118). Extramedullary disease is common, with 35 cases reporting some extramedullary involvement. Of these, at least 25 were myelosarcomas (10 mediastinal, 2 abdominal, 1 mammary, 1 uterine, 11 unknown location). However, the type of extramedullary disease was not always specified. Thus, the young, male patient with extensive extramedullary involvement we present here has quite typical clinical features of PICALM::MLLT10-rearranged AML.
Karyotypes were available for 63 cases. There was a median of 1 cytogenetic abnormality (range: 0–15) besides PICALM::MLLT10. 29 cases had cytogenetic aberrations associated with a poor prognosis, while only one each had an aberration that is associated with favorable/intermediate outcome according to the European Leukemia Net risk stratification from 2022. Eight had trisomy 4 and eight had trisomy 19. In seven patients i17(q10) co-occurred, while no other cytogenetic aberration was co-occurring in more than three cases. Immunophenotypic markers are available for 69 cases. Markers commonly associated with AML were widely reported, while CD7 was the most frequent aberrant marker (27/34 cases). Unfortunately, molecular genetic analyses are not available for the majority of previously reported cases. However, following the introduction of next generation sequencing analysis in increasing numbers of AL patients, newer series make it apparent that PICALM::MLLT10 has a characteristic comutational profile. The most frequent co-mutations occurred in PHF6 (22), TP53 (12), NF1, NRAS, SUZ12 (8 each), WT1 (6) and EZH2 (5). As our patient also had two EZH2 mutations, we investigated these co-occurrences further. In a series of 15 AL (12 T-ALL, 1 MPAL, 2 AML) patients with PICALM::MLLT10 rearrangement 4 (including one AML) cases carried mutations in EZH2, which usually is very rare in AL, with one report finding one mutation amongst 113 AML cases and another finding no EZH2mut in 54 AML patients [16, 29, 45]. Notably, four more patients in the series (including the other reported AML) carried a polymorphism of EZH2. Another analysis of PICALM::MLLT10-rearranged AL found EZH2mut in 6/20 cases (ALAL, T-ALL and AML) [35]. Furthermore, one analysis of MLLT10-fusions in pediatric AML found another three patients with the co-occurrence of PICALM::MLLT10 and EZH2 mutations [24].
Discussion
The literature to date suggests, that PICALM::MLLT10 rearranged AML is associated with unusually young age, male sex, and (mediastinal) myelosarcoma, which our case confirms. Unfortunately, our patient seems to confirm the previously reported trend towards adverse outcome. A recent large retrospective analysis also confirms the negative prognosis in the pediatric population [6]. A large analysis suggests that MLLT10, regardless of the fusion partner, always seems to convey adverse outcomes [5].
A significant percentage of published cases (23/63) had a complex karyotype. However, it is unclear whether the genomic instability required to produce these karyotypes is cause or effect of the PICALM::MLLT10-rearrangement. While the high incidence of trisomies 4 and 19 that was first noted by Borel et al. [4] is confirmed by other published cases, our patient did not have such aberrations.
As described in the literature, the occurrence of this translocation not only in AML, but as well in both ALL and MPAL points towards its occurrence in a pluripotent progenitor cell compartment [32, 46]. The descendants of this progenitor might then develop into different ALs depending on the differentiation they undergo and secondary alterations accumulated. This could also explain the high latency of AL development in a transgenic murine model [47]. Research in this area is ongoing, with the current WHO classification of myeloid disease hinting at a potential re-definition of PICALM:: MLLT10 as a MPAL-defining genetic aberration in the next update of the classification [7].
While better genetic characterization of this entity is needed, a pattern of typical co-mutations seems to emerge from our literature analysis. Our case-report matches the published co-mutations well, as the mutations in EZH2, NRAS and TP53 all seem frequent in this population. However, NRAS and TP53 are also frequently mutated in other AML [48]. EZH2 on the other hand seems more closely associated with PICALM::MLLT10. EZH2 is the catalytic subunit of the Polycomb Repressor Complex 2 (PRC2), which recruits PRC1 via methylation markers. Together, they mediate long term epigenetic silencing of chromatin. Studies in hepatocellular carcinoma, esophageal squamous cell carcinoma and prostate cancer have shown a synergistic effect of BMI1- and EZH2-upregulation, while the interaction in breast cancer seems more complex [49,50,51,52,53,54,55]. Therefore, we hypothesize that, if BMI1-upregulation is the relevant mechanism of leukemogenesis in PICALM::MLLT10 positive AL, acquiring an EZH2 mutation constitutes a crucial survival benefit, leading to selection of EZH2 mutated clones. This hypothesis would explain the strikingly elevated frequency of EZH2 mutations in PICALM::MLLT10 positive AML. Multiple large cohorts of AML patients (Basheer et al.: n = 2434; Papapemmanuil et al.: n = 1540; Rausch et al.: n = 1138; Stasik et al.: n = 1604; Wang et al.: n = 714), have found EZH2mut in 5% (Basheer), 4% (Papaemmanuil, Rausch, Stasik), and 2% of AML cases, respectively, and some smaller studies show barely any cases (1/113, 0/54) [16, 17, 45, 56,57,58,59]. EZH2mut are associated with worse OS, with one large study observing a trend towards even worse outcomes for homozygous mutations and mutations of the SET-domain [17]. In contrast to the low incidence of EZH2mut observed in large unselected cohorts of AML, we and others have shown frequent occurrence of EZH2mut in PICALM::MLLT10 positive AML [24, 29, 35]. However, the potential association between PICALM::MLLT10 rearrangements and EZH2mut is based on small samples and further studies are needed.
In addition, our hypothesis strengthens the case for BMI1-mediated leukemogenesis. Clinically, the possibility of targeting both BMI1 and EZH2 therapeutically makes this finding especially relevant [15]. In follicular lymphoma, the EZH2-Inhibitor tazemetostat is already approved by the FDA, proving the safety of targeting EZH2 in humans [60]. In AML EZH2-inhibitors have already shown promise in PDX-mouse-models [61].
In conclusion, this report not only highlights and confirms the clinical characteristics of PICAL::MLLT10mut AML, but also elucidates key molecular mechanisms as well as potential targets for eventual therapeutic intervention.
Data Availability
As this report contains data of an individual patient, we cannot make the data available to protect our patients privacy.
References
Sundström C, Nilsson K. Establishment and characterization of a human histiocytic lymphoma cell line (U-937). Int J Cancer. 1976;17:565–77.
Dreyling MH, Martinez-Climent JA, Zheng M, Mao J, Rowley JD, Bohlander SK. The t(10;11)(p13;q14) in the U937 cell line results in the fusion of the AF10 gene and CALM, encoding a new member of the AP-3 clathrin assembly protein family. Proc Natl Acad Sci USA. 1996;93:4804–9.
Meyer C, Larghero P, Almeida Lopes B, Burmeister T, Gröger D, Sutton R, et al. The KMT2A recombinome of acute leukemias in 2023. Leukemia 2023;37:988-1005.
Borel C, Dastugue N, Cances-Lauwers V, Mozziconacci MJ, Prebet T, Vey N, et al. PICALM-MLLT10 acute myeloid leukemia: a French cohort of 18 patients. Leuk Res. 2012;36:1365–9.
Forgione MO, McClure BJ, Yeung DT, Eadie LN, White DL. MLLT10 rearranged acute leukemia: Incidence, prognosis, and possible therapeutic strategies. Genes, Chromosomes Cancer. 2020;59:709–21.
Mark C, Meshinchi S, Joyce B, Gibson B, Harrison C, Bergmann AK, et al. Treatment outcomes of childhood PICALM::MLLT10 acute leukaemias. Br J Haematol. 2024;204:576–84.
Khoury JD, Solary E, Abla O, Akkari Y, Alaggio R, Apperley JF, et al. The 5th edition of the World Health Organization Classification of Haematolymphoid Tumours: Myeloid and Histiocytic/Dendritic Neoplasms. Leukemia. 2022;36:1703–19.
Asnafi V, Radford-Weiss I, Dastugue N, Bayle C, Leboeuf D, Charrin C, et al. CALM-AF10 is a common fusion transcript in T-ALL and is specific to the TCRγδ lineage. Blood. 2003;102:1000–6.
Deshpande AJ, Rouhi A, Lin Y, Stadler C, Greif PA, Arseni N, et al. The clathrin-binding domain of CALM and the OM-LZ domain of AF10 are sufficient to induce acute myeloid leukemia in mice. Leukemia. 2011;25:1718–27.
Dik WA, Brahim W, Braun C, Asnafi V, Dastugue N, Bernard OA, et al. CALM-AF10 + T-ALL expression profiles are characterized by overexpression of HOXA and BMI1 oncogenes. Leukemia. 2005;19:1948–57.
Mulaw MA, Krause A, Riedel A, Tizazu B, Reuter H, Bohlander SK. Early target genes of CALM/AF10 as revealed by gene expression profiling. Blood. 2008;112:2260.
Okada Y, Jiang Q, Lemieux M, Jeannotte L, Su L, Zhang Y. Leukaemic transformation by CALM–AF10 involves upregulation of Hoxa5 by hDOT1L. Nat Cell Biol. 2006;8:1017–24.
Conway AE, Scotland PB, Lavau CP, Wechsler DS. A CALM-derived nuclear export signal is essential for CALM-AF10-mediated leukemogenesis. Blood. 2013;121:4758–68.
Abramovich C, Humphries RK. Hox regulation of normal and leukemic hematopoietic stem cells. Curr Opin Hematol. 2005;12:210–6.
Barbosa K, Deshpande A, Chen BR, Ghosh A, Sun Y, Dutta S, et al. Acute myeloid leukemia driven by the CALM-AF10 fusion gene is dependent on BMI1. Exp Hematol. 2019;74:42–51.e43.
Ernst T, Chase AJ, Score J, Hidalgo-Curtis CE, Bryant C, Jones AV, et al. Inactivating mutations of the histone methyltransferase gene EZH2 in myeloid disorders. Nat Genet. 2010;42:722–6.
Stasik S, Middeke JM, Kramer M, Röllig C, Krämer A, Scholl S, et al. EZH2 mutations and impact on clinical outcome: an analysis in 1,604 patients with newly diagnosed acute myeloid leukemia. Haematologica. 2020;105:e228–e231.
Abu-Shihab Y, Nicolet D, Mrózek K, Routbort M, Patel KP, Walker CJ, et al. BRAF-mutated acute myeloid leukemia (AML) represents a distinct, prognostically poor subgroup enriched in myelodysplasia-related (MR-)AML. Blood. 2023;142:1575.
George GV, Evans AG, Jajosky AN. BRAF V600E-mutant acute myeloid leukemia: a case series and literature review of a rare entity. Genes. 2024;15:1383.
Robert C, Grob JJ, Stroyakovskiy D, Karaszewska B, Hauschild A, Levchenko E, et al. Five-Year Outcomes with Dabrafenib plus Trametinib in Metastatic Melanoma. N. Engl J Med. 2019;381:626–36.
Wander SA, Hasserjian RP, Oduro K, Glomski K., Nardi V, Cote GM, et al. Combined targeted therapy for BRAF-mutant, treatment-related acute myeloid leukemia. JCO Precision Oncology 2017:1–7.
Abdelhaleem M, Beimnet K, Kirby-Allen M, Naqvi A, Hitzler J, Shago M. High incidence of CALM-AF10 fusion and the identification of a novel fusion transcript in acute megakaryoblastic leukemia in children without Down’s syndrome. Leukemia. 2007;21:352–3.
Abdou SM, Jadayel DM, Min T, Swansbury GJ, Dainton MG, Jafer O, et al. Incidence of MLL Rearrangement in Acute Myeloid Leukemia, and a CALM - AF10 Fusion in M4 Type Acute Myeloblastic Leukemia. Leuk Lymphoma. 2002;43:89–95.
Abla O, Ries RE, Triche T Jr, Gerbing RB, Hirsch B, Raimondi S, et al. Structural variants involving MLLT10 fusion are associated with adverse outcomes in pediatric acute myeloid leukemia. Blood Adv. 2024;8:2005–17.
Borel C, Huynh A, Chaufour X, Lousteau O, Demur C, Delabesse E, et al. Uterine chloroma, aortic thrombus and CALM/AF10 acute myeloid leukemia. Leuk Res. 2010;34:e88–90.
Dreyling MH, Schrader K, Fonatsch C, Schlegelberger B, Haase D, Schoch C, et al. MLL and CALM are fused to AF10 in morphologically distinct subsets of acute leukemia with translocation t(10;11): both rearrangements are associated with a poor prognosis. Blood. 1998;91:4662–7.
Carlson KM, Vignon C, Bohlander S, Martinez-Climent JA, Beau MML, Rowley JD. Identification and molecular characterization of CALM/AF10 fusion products in T cell acute lymphoblastic leukemia and acute myeloid leukemia. Leukemia. 2000;14:100–4.
Dargenio M, Federico V, Matera R, Seripa D, Fina MP, Vergine C, et al. Extramedullary involvement in a patient with CD7+ and CD56+ Acute Myeloid Leukemia (AML) and PICALM-MLLT10 fusion gene: A challenging diagnosis and treatment. J Clin Med Images Case Rep. 2024;4:1653.
Grossmann V, Bacher U, Kohlmann A, Artusi V, Klein HU, Dugas M, et al. EZH2 mutations and their association with PICALM-MLLT10 positive acute leukaemia. Br J Haematol. 2012;157:387–90.
Huh JY, Chung S, Oh D, Kang MS, Eom HS, Cho EH, et al. Clathrin assembly lymphoid myeloid leukemia-AF10-positive acute leukemias: a report of 2 cases with a review of the literature. Korean J Lab Med. 2010;30:117–21.
Jones LK, Chaplin T, Shankar A, Neat M, Patel N, Samuel DP, et al. Identification and molecular characterisation of a CALM-AF10 fusion in acute megakaryoblastic leukaemia. Leukemia. 2001;15:910–4.
Kobayashi H, Hosoda F, Maseki N, Sakurai M, Imashuku S, Ohki M, et al. Hematologic malignancies with the t(10;11) (p13;q21) have the same molecular event and a variety of morphologic or immunologic phenotypes. Genes Chromosomes Cancer. 1997;20:253–9.
Kumon K, Kobayashi H, Maseki N, Sakashita A, Sakurai M, Tanizawa A, et al. Mixed-lineage leukemia with t(10;11)(p13;q21): an analysis of AF10-CALM and CALM-AF10 fusion mRNAs and clinical features. Genes Chromosomes Cancer. 1999;25:33–39.
Meyer C, Larghero P, Almeida Lopes B, Burmeister T, Gröger D, Sutton R, et al. Dual-color split signal fluorescence in situ hybridization assays for the detection of CALM/AF10 in t(10;11)(p13;q14-q21)-positive acute leukemia. Haematologica 2006;91:1248-51.
Ma J, Liu Y-C, Voss RK, Ma J, Palagani A, Caldwell E, et al. Genomic and global gene expression profiling in pediatric and young adult acute leukemia with PICALM::MLLT10 Fusion. Leukemia. 2024;38:981–90.
Naesens L, Devos H, Nollet F, Michaux L, Selleslag D. Mediastinal myeloid sarcoma with TP53 mutation preceding acute myeloid leukemia with a PICALM-MLLT10 Fusion gene. Acta Haematologica. 2018;140:97–104.
Nakamura F, Maki K, Arai Y, Nakamura Y, Mitani K. Monocytic leukemia with CALM/AF10 rearrangement showing mediastinal emphysema. Am J Hematol. 2003;72:138–42.
Park MS, Kim HY, Lee JJ, Cho D, Jung CW, Kim HJ, et al. The first case of acute myeloid leukemia with t(10;11)(p13;q21);PICALM-MLLT10 rearrangement presenting with extensive skin involvement. Ann Lab Med. 2023;43:310–4.
Savage NM, Kota V, Manaloor EJ, Kulharya AS, Pierini V, Mecucci C, et al. Acute leukemia with PICALM-MLLT10 fusion gene: diagnostic and treatment struggle. Cancer Genet Cytogenet. 2010;202:129–32.
Sindt A, Deau B, Brahim W, Staal A, Visanica S, Villarese P, et al. Acute monocytic leukemia with coexpression of minor BCR-ABL1 and PICALM-MLLT10 fusion genes along with overexpression of HOXA9. Genes Chromosomes Cancer. 2006;45:575–82.
Sun H, Zhu Y, Li J, Zhao L, Yang G, Yan Z, et al. PICALM::MLLT10 may indicate a new subgroup of acute leukemias with miscellaneous immunophenotype and poor initial treatment response but showing sensitivity to venetoclax. eJHaem. 2024;5:565–72.
Wang J, Zhang W, Xu X, Buglioni A, Li P, Chen X, et al. Clinicopathologic features and outcomes of acute leukemia harboring PICALM::MLLT10 fusion. Hum Pathol. 2024;151:105626.
Wang J-n, Bangcheng Y, Fei C, Li Y, Yongxian H, Gaofeng Z, et al. PICALM-MLLT10 fusion gene in hematological neoplasms: clinical features, current practices, and prognoses. Hematology. 2024;29:2423324.
Zhang X, Zhong J, Sun Y, Wu S. PICALM::MLLT10 fusion gene positive acute myeloid leukemia with PHF6 mutation and presented with CD7 positive immunophenotype. Cytom B Clin Cytom. 2025;108:179–82.
Makishima H, Jankowska AM, Tiu RV, Szpurka H, Sugimoto Y, Hu Z, et al. Novel homo- and hemizygous mutations in EZH2 in myeloid malignancies. Leukemia. 2010;24:1799–804.
Bohlander SK, Muschinsky V, Schrader K, Siebert R, Schlegelberger B, Harder L, et al. Molecular analysis of the CALM/AF10 fusion: identical rearrangements in acute myeloid leukemia, acute lymphoblastic leukemia and malignant lymphoma patients. Leukemia. 2000;14:93–9.
Caudell D, Zhang Z, Chung YJ, Aplan PD. Expression of a CALM-AF10 fusion gene leads to Hoxa cluster overexpression and acute leukemia in transgenic mice. Cancer Res. 2007;67:8022–31.
Metzeler KH, Herold T, Rothenberg-Thurley M, Amler S, Sauerland MC, Görlich D, et al. Spectrum and prognostic relevance of driver gene mutations in acute myeloid leukemia. Blood. 2016;128:686–98.
Sasaki M, Ikeda H, Itatsu K, Yamaguchi J, Sawada S, Minato H, et al. The overexpression of polycomb group proteins Bmi1 and EZH2 is associated with the progression and aggressive biological behavior of hepatocellular carcinoma. Lab Invest. 2008;88:873–82.
Xu L, Lin J, Deng W, Luo W, Huang Y, Liu CQ, et al. EZH2 facilitates BMI1-dependent hepatocarcinogenesis through epigenetically silencing microRNA-200c. Oncogenesis. 2020;9:101.
Ha SY, Kim SH. Co-expression of Bmi1 and EZH2 as an independent poor prognostic factor in esophageal squamous cell carcinoma. Pathol Res Pr. 2012;208:462–9.
Yamada A, Fujii S, Daiko H, Nishimura M, Chiba T, Ochiai A. Aberrant expression of EZH2 is associated with a poor outcome and P53 alteration in squamous cell carcinoma of the esophagus. Int J Oncol. 2011;38:345–53.
van Leenders GJ, Dukers D, Hessels D, van den Kieboom SW, Hulsbergen CA, Witjes JA, et al. Polycomb-group oncogenes EZH2, BMI1, and RING1 are overexpressed in prostate cancer with adverse pathologic and clinical features. Eur Urol. 2007;52:455–63.
Lee YC, Chang WW, Chen YY, Tsai YH, Chou YH, Tseng HC, et al. Hsp90α mediates BMI1 expression in breast cancer stem/progenitor cells through facilitating nuclear translocation of c-Myc and EZH2. Int J Mol Sci.2017:18.
Pietersen AM, Horlings HM, Hauptmann M, Langerød A, Ajouaou A, Cornelissen-Steijger P, et al. EZH2 and BMI1 inversely correlate with prognosis and TP53 mutation in breast cancer. Breast Cancer Res. 2008;10:R109.
Basheer F, Giotopoulos G, Meduri E, Yun H, Mazan M, Sasca D, et al. Contrasting requirements during disease evolution identify EZH2 as a therapeutic target in AML. J Exp Med. 2019;216:966–81.
Papaemmanuil E, Gerstung M, Bullinger L, Gaidzik VI, Paschka P, Roberts ND, et al. Genomic classification and prognosis in acute myeloid leukemia. N. Engl J Med. 2016;374:2209–21.
Rausch, C, Rothenberg-Thurley, M, Dufour, A, Schneider, S, Gittinger, H, Sauerland, C et al. Validation and refinement of the 2022 European LeukemiaNet genetic risk stratification of acute myeloid leukemia. Leukemia. 2023;37:1234–44.
Rausch C, Rothenberg-Thurley M, Dufour A, Schneider S, Gittinger H, Sauerland C, et al. EZH2 mutations are related to low blast percentage in bone marrow and -7/del(7q) in de novo acute myeloid leukemia. PLoS One. 2013;8:e61341.
Morschhauser F, Tilly H, Chaidos A, McKay P, Phillips T, Assouline S, et al. Tazemetostat for patients with relapsed or refractory follicular lymphoma: an open-label, single-arm, multicentre, phase 2 trial. Lancet Oncol. 2020;21:1433–42.
Porazzi P, Petruk S, Pagliaroli L, De Dominici M, Deming D II, Puccetti MV, et al. Targeting chemotherapy to decondensed H3K27me3-marked chromatin of AML cells enhances leukemia suppression. Cancer Res. 2022;82:458–71.
Acknowledgements
We thank the patient who consented to this report.
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
CR and TP designed the analysis. UB and JT contributed laboratory and genetic data. MH and KS cared for the patient and contributed clinical data. CR conducted the literature search, analyzed the data and wrote the manuscript. TH and UB contributed to writing the manuscript. All authors edited and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
CR: Travel funding: International Medical Education, Jazz Pharmaceuticals and Servier; Advisory Boards: BeiGene, Servier, Takeda.
Ethics approval and consent to participate statement
All methods were performed in accordance with the relevant guidelines and regulations. The study was approved by a decision of the local ethics committee from Berne, Switzerland (decision number #2024-00879; decision date 17.09.2024). Written informed consent as per institutional guideline was obtained from the patient. No identifiable images of the patient are presented in the study.
Consent for publication
The patient described in this report consented to the publication of their case.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Rausch, C., Bacher, U., Tchinda, J. et al. Observation of PICALM::MLLT10-rearrangement and coincidental EZH2 mutations in a patient with acute myeloid leukemia: A case report and review of the literature. BJC Rep 3, 66 (2025). https://doi.org/10.1038/s44276-025-00175-w
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s44276-025-00175-w