Abstract
We aimed to derive a new high-sensitivity cardiac troponin I Access (hs-cTnI-Access) 0/1h-algorithm suitable for Chinese patients. In the multi-centre study, we enrolled 369 patients with suspected non-ST-segment elevation myocardial infarction (NSTEMI). Following an adjustment, AnZhen hs-cTnI-Access 0/1h-algorithm was established with rule-in cut-off values of 0 h ≥ 50 pg/mL or Δ1h ≥ 18.0 pg/mL and rule-out cut-off values of 0 h < 3 pg/mL or 0 h < 4 pg/mL and Δ1h < 3.0 pg/mL. These revised cutoffs presented a negative predictive value (NPV) of 99.46% (95% CI,97.02–99.91%) and a sensitivity of 98.81% (95% CI,93.56–99.79%), and also resulted in a positive predictive value (PPV) of 86.42% (95% CI,77.30–92.24%) and a specificity of 96.14% (95% CI,93.22–97.83%), both of which were superior to those of the ESC 0/1 h algorithm. The new hs-cTnI-Access 0/1 h-algorithm adjusted for Chinese data is promising for improving both safety and efficacy in Chinese patients.
Similar content being viewed by others
Introduction
Acute myocardial infarction (AMI) is characterized by rapid onset, severity, and a high mortality rate, whereas non-ST-segment elevation myocardial infarction (NSTEMI) is easily missed and misdiagnosed. The near- and long-term prognosis of patients with NSTEMI is worse than that of patients with acute ST-segment elevation myocardial infarction (STEMI)1,2. The early diagnosis and screening of NSTEMI are essential. High-sensitivity cardiac troponin (hs-cTn) level is an important addition to clinical information for the rapid triage of patients with NSTEMI in the emergency room3.
Recent diagnostic studies have demonstrated that the safety and efficacy of the hs-cTnI 0/1 h-algorithm are higher than those of the 0/3 h algorithm advocated by the European Society of Cardiology for acute coronary syndromes without persistent ST-segment elevation (European Society of Cardiology NSTE-ACS) guidelines4,5,6. An overseas study, based on a large real-world dataset, revealed that the incorporation of hs-cTnI in patients with suspected ACS can reduce the overall length of stay (LOS) by 1.9 h, delivering significant benefits to emergency departments (ED)7. Consequently, the 2020 ESC NSTE-ACS guidelines recommended the 0/1 h-algorithm as the primary choice and the 0/2 h-algorithm as an alternative option for screening patients with suspected NSTEMI8 in the ED. The 0/1 h-algorithm has been derived and validated in several large foreign cohort studies9,10.
The widely accepted 0/1h-algorithm uses a rule-in cut-off value of 0 h ≥ 50 pg/mL or Δ1h ≥ 15.0 pg/mL, and the rule-out cut-off value of 0 h < 4 pg/mL or 0 h < 5 pg/mL and Δ1h < 4.0 pg/mL. A previous study reported that the NPV of the hs-cTnI 0/1h-algorithm was 99.8–100% while the PPV was 73.8–73.9%9.
While the cutoffs of the ESC hs-cTnI 0/1h-algorithm were originally derived from data obtained from a foreign population and may not apply to the Chinese population, there has been a notable absence of experimentation involving Chinese patients. Consequently, this study adopted the Beckman hs-TnI-Access assay to establish two hs-cTnI-Access 0/1 h-algorithms for Chinese patients suspected of having NSTEMI, employing ESC-recommended and adjusted cut-offs suitable for Chinese patients. Our primary objective was to compare the performance of this novel hs-cTnI-Access 0/1h-algorithm with that of the established ESC 0/1 h-algorithm, with the ultimate goal of identifying potentially more suitable cutoff values for the Chinese population.
Results
Characteristics of patients
A total of 369 patients with suspected NSTEMI were eligible for enrollment in this study, and all underwent coronary angiography (CAG) or CCTA to confirm the diagnoses (Fig. 1). The general characteristics of all patients are presented in Table 1.
Adjudicated final diagnosis
The final diagnosis of NSTEMI was confirmed in 84 (22.8%) patients and 285 patients with non-NSTEMI, including 130 with unstable angina (UA), 28 with cardiac-related diseases excluding acute coronary syndrome (ACS), and 127 with non-cardiac-related diseases (Table 2).
Measurements of Access hs-cTnI at presentation (0 h) in patients with suspected NSTEMI
The concentrations of Access hs-cTnI at presentation in patients diagnosed with adjudicated NSTEMI were significantly elevated compared to those in the non-NSTEMI group (P < 0.001; Table 2, Fig. 2). Specifically, the median Access hs-cTnI concentrations in the NSTEMI group measured 90.3 pg/mL (IQR,34.4–640.4), which were notably higher than that in the UA group (3.4 pg/mL, IQR,2.3–8.3), the cardiac disease group excluding ACS (3.3 pg/mL, IQR, 2.3–5.3), and the non-cardiac related disease group (2.8 pg/mL, IQR,1.9–4.0). Statistically significant differences were observed between the NSTEMI group and each of the other etiology groups (P < 0.001; Table 2).
Boxplots showing concentrations of hs-cTnI Access at presentation according to the final diagnoses. Boxes represent medians and interquartile ranges (IQRs), while whiskers display the smallest and the largest non-outliers. NSTEMI non-ST-segment elevation myocardial infarction, UA unstable angina, Cardiac but not ACS cardiac related diseases excluding acute coronary syndrome, e.g. stable angina, Non-Cardiac non-cardiac related diseases, e.g. intercostal neuralgia, pneumonia and so on.
Details of targeted vessels and treatment decisions
All patients in NSTEMI group underwent CAG to confirm the final diagnoses, while there were 79.2% of patients in UA group conducted CAG and 89.3% in Cardiac but not ACS group. Via CAG and CCTA, we collected vessel information and therapeutic response data from targeted patients, which are presented in Table 3. The details related to the number of stents and processed targeted vessels in each group are shown in Table 3. After discharge, 97.6%, 98.3% and 71.4% of patients in the NSTEMI, UA, and Cardiac but not ACS groups, respectively, received anti-platelet therapy (p < 0.001, Table 3).
Diagnostic accuracy of access hs-cTnI for NSTEMI
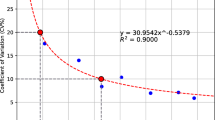
The area under the ROC curve (AUC) values for concentrations obtained at presentation (0 h) using Access hs-cTnI was 0.906, as depicted in Fig. 3 and summarized in Table 4.
The performance of serial concentrations of Access hs-cTnI detected at 0 h, 1 h, Δ1h, and 3 h yielded the following AUCs: 0.906 (95% CI, 0.855, 0.956), 0.966 (95% CI, 0.945, 0.987), 0.957 (95% CI, 0.936, 0.977), and 0.974 (95% CI, 0.955, 0.993), respectively. When we combined the concentrations of 0 h and Δ1h, the AUC was 0.964 (95% CI, 0.946, 0.982). Additionally, when we combined the concentrations of 0 h and Δ3h, the AUC was 0.973 (95% CI, 0.958, 0.988), as indicated in Table 4 and Fig. 4.
Applying ESC recommendation to 0/1h-algorithm for the Chinese population
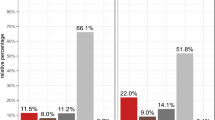
Rule-in cut-off values of 0 h ≥ 50 pg/mL or Δ 1 h ≥ 15.0 pg/mL, rule-out cut-off values of 0 h < 4 pg/mL (chest pain symptoms present for more than 3 h) or 0 h < 5 pg/mL and Δ 1 h < 4.0 pg/mL were selected according to the 0/1 h-algorithm recommended by the ESC guidelines. Finally, 82 patients were ruled in as having NSTEMI, 208 patients were ruled out as having non-NSTEMI, and 79 patients who were not eligible for either of the above criteria were assigned to the observation group and dynamically observed for hs-cTnI changes until 3 h after the visit. An access hs-cTnI test1,2 was performed repeatedly 3 h after presentation at the ED. The ESC 0/1h-algorithm allowed 290 patients to be triaged within 1 h of presentation, with an NPV of 98.08% (95.16–99.25%), Sens of 95.24% (88.39–98.13%), a PPV of 85.37% (76.14–91.43%), and Spec of 95.79% (92.79–97.58%) (see Fig. 5a).
a Performance of the ESC high-sensitivity cardiac troponin I Access 0/1 h algorithm in the Chinese population. ESC European Society of Cardiology, NSTEMI non-ST-segment elevation myocardial infarction, NPV negative predictive value, Sens sensitivity, PPV positive predictive value, Spec specificity. b Performance of the AnZhen 0/1h-01 algorithm in the Chinese population. NSTEMI non-ST-segment elevation myocardial infarction, NPV negative predictive value, Sens sensitivity, PPV positive predictive value, Spec specificity. c Performance of the AnZhen 0/1h-02 algorithm in the Chinese population. NSTEMI non-ST-segment elevation myocardial infarction, NPV negative predictive value, Sens sensitivity, PPV positive predictive value, Spec specificity.
The ESC guidelines recommend that rule-out cut-off values should be chosen to achieve a minimum negative predictive value (NPV) of 99% and sensitivity of 90%. For rule-in cut-off values, a positive predictive value of 70% is typically sought. However, it’s worth noting that the ESC 0/1 h-algorithm, when applied to Chinese patients, achieved an NPV of 98.08% (with a confidence interval of 95.16–99.25%). Consequently, it becomes evident that adjustments are required to tailor the cut-off values to better suit the Chinese population.
Establishing cut-off values appropriate for the Chinese population and direct comparison with the ESC 0/1 h algorithm
We implemented predetermined diagnostic and exclusion thresholds using a categorical regression tree (CART), in accordance with ESC guidelines, aiming to achieve the minimum requirements of NPV > 99.5%, Sens > 99%, and PPV > 70%.
Initially, we adjusted the rule-in cut-off values to 0 h ≥ 28 pg/mL or Δ 1 h ≥ 18.0 pg/mL and the rule-out cut-off values to 0 h < 3 pg/mL (with an onset of chest pain >3 h) or 0 h < 4 pg/mL and Δ 1 h < 3.0 pg/mL to establish the AnZhen 0/1 h-01-algorithm. In this version, 92 patients were adjudicated to the rule-in group, with 76 patients ultimately diagnosed with NSTEMI, resulting in a PPV of 82.61% (73.60–89.0%) and a specificity of 94.39% (91.08–96.52%). Conversely, 186 patients were adjudicated to the rule-out group, and one case was confirmed as NSTEMI (a misdiagnosis rate of 1.19%), yielding an NPV of 99.46% (97.02–99.91%) and a sensitivity of 98.81% (93.56–99.79%). These adjustments significantly improved NPV and PPV compared to the ESC recommended cut-off values (see Fig. 5b).
Subsequently, we recognized that setting the rule-in cut-off value to 0 h ≥ 28 pg/mL might lead to an increased false positive rate and over-screening. Given that 0 h > 50 ng/L is the common clinical criterion, we further adjusted the rule-in cut-off value to 0 h ≥ 50 pg/mL or Δ 1 h ≥ 18.0 pg/mL. A total of 81 patients were categorized in the rule-in group, and the AnZhen 0/1h-02-algorithm was established. 70 patients were finally diagnosed with NSTEMI, with a PPV of 86.42% (77.30–92.24%), Spec of 96.14% (93.22%-97.83%), and NPV consistent with Sens (Fig. 5c). This is the terminal version of the AnZhen 0/1 h algorithm.
Overall, when directly comparing the AnZhen 0/1 h-02 algorithm with the ESC 0/1 h algorithm, the new hs-cTnI-Access 0/1 h algorithm demonstrated superior performance in accurately diagnosing and ruling out patients having NSTEMI, with notably higher NPV and PPV.
Details of clinical information in “Rule-in”, “Rule-out” and “Observe” groups
Table 5 provided the final diagnoses and other clinical information of patients in three groups derived by AnZhen 0/1 h-02-algorithm. 86.4% of patients in Rule-in group were diagnosed as NSTEMI finally, while there were 59.8% in Observe group categorized as NSTE-ACS (NSTEMI and UA).In the Rule-in group, there was only one patient didn’t undergo CAG to confirm final diagnosis.
“Observe” group
Building upon the foundation of the AnZhen 0/1 h-02 algorithm, we aimed to enhance the precise triage of patients in the observation group. To achieve this, we introduced a criterion of Δ 3 h ≥ 17.5 pg/mL into the rule-in cut-off values. As a result, 10 cases were successfully categorized into either the NSTEMI group or the non-NSTEMI group after 3 h of continuous monitoring.
Prognostic performance of the AnZhen hs-cTnI-Access 0/1 h-algorithm
The cumulative event rates during the 30-day follow-up period were 4.94%, 0%, and 0% in the rule-in, observe, and rule-out groups, respectively. After 2 years, the cumulative event rates were 17.28%, 9.80%, and 1.08% in the rule-in, observe, and rule-out groups, respectively. After 3 years, the cumulative event rates were 18.52%, 11.76%, and 1.61% in the three groups respectively (Fig. 6). In total, there were 15 MACCEs occurred in the rule-in group, including cardiovascular death (n = 1), all-cause mortality (n = 1), nonfatal myocardial infarction (n = 2), refractory angina (n = 10), new onset heart failure (n = 1). 12 MACCEs occurred in the observation group, including refractory angina (n = 10), new onset heart failure (n = 1), and stroke (n = 1). 3 MACCEs occurred in the rule-out group, including all-cause mortality (n = 1) and refractory angina (n = 2).
Discussion
In China, acute myocardial infarction ranks as the second leading cause of death11. Recent studies have shown that high-sensitivity troponin exhibits higher positive and negative predictive values compared to other markers of myocardial injury12,13. Although the ESC guidelines recommend a 0/1 h diagnostic algorithm, it is important to note that specific troponin values are based on large foreign cohort studies that require more Chinese data. Therefore, this study examined the high-sensitivity troponin I 0/1 h algorithm in patients with suspected NSTEMI based on data from a Chinese population to explore the appropriate definitive diagnosis and exclusion criteria for the Chinese population.
Based on the platform of the Emergency Chest Pain Center at Beijing AnZhen Hospital, The second hospital of Jilin University and Shanxi Cardiovascular Hospital, we collected national data to examine and optimize the hs-cTnI-Access 0/1 h algorithm for the Chinese population. There were seven findings from this experiment.
First, when we applied the ESC hs-cTnI-Access 0/1h-algorithm to Chinese patients, we triaged 290 cases into rule-in and rule-out groups, constituting 78.59% of the total cohort. However, the algorithm yielded an NPV of 98.08% (with a confidence interval of 95.16–99.25%), falling short of the minimum NPV recommended by ESC guidelines. It’s worth noting that several large multicenter studies conducted abroad have confirmed the excellent diagnostic utility of the hs-cTnI 0/1h-algorithm and the 0/2h-algorithm in patients with suspected NSTEMI4,8,9,10,14,15,16,17,18,19. Yet, the applicability of these algorithms to the Chinese population remains a subject of debate due to the lack of supporting Chinese data.
Secondly, we employed CART to derive new cut-off values tailored specifically for Chinese patients. The terminal iteration of the AnZhen 0/1h-algorithm ultimately assigned 50.41% of patients to the rule-out group, achieving an NPV of 99.46% (95% CI, 97.02–99.91%). However, it is crucial to emphasize that in practical clinical applications, diagnosis should not rely solely on 0 h and 1 h hs-cTnI values. Instead, a comprehensive assessment, encompassing patients’ medical histories, physical examinations, symptomatic features, electrocardiography (ECG), echocardiography, and invasive tests9,14,20, should be conducted to further enhance the NPV, potentially approaching 100%.
Third, within the rule-in group, the positive predictive value (PPV) for NSTEMI in the final AnZhen 0/1h-algorithm stood at 86.42% (95% CI, 77.30–92.24%). Among these patients, 11 cases were diagnosed with other conditions, including unstable angina (UA) and cardiac-related diseases, while acute coronary syndrome (ACS) was excluded. For these individuals, further diagnostic steps such as coronary angiography or CCTA were deemed necessary to confirm the diagnosis. The establishment of this rule-in group was intended to provide a valuable tool for clinicians faced with challenging scenarios, assisting them in deciding whether a more comprehensive examination of the coronary arteries should be pursued.
Fourth, we incorporated the 3-hour hs-cTnI cut-off values into the AnZhen 0/1 h algorithm to enhance the accuracy of diagnosis for patients in the observation group. This extension to the algorithm allowed for a definitive diagnosis within 3 h in 277 out of 369 patients (75.07%), either ruling out or ruling in NSTEMI. This approach aligns with the findings of previous large trials and underscores the importance of monitoring hs-cTnI levels beyond the initial assessment, particularly for patients suspected of having NSTEMI6,21.
Fifth, in some cases, we observed obvious change of hs-cTnI values among patients in the non-NSTEMI groups. Traditionally, individuals with severe coronary artery stenosis exhibited significantly elevated hs-cTnI concentrations. It is essential to consider that non-ischemic physiological conditions can also result in variations in hs-cTnI levels22,23,24,25,26,27. While the 1-h hs-cTnI algorithm may categorize some of them into the rule-in group, it is important to emphasize that the algorithm primarily serves as an alert for clinicians, recognizing potential cardiac events in urgent situations.
Sixth, during our follow-up of patients after discharge, we observed the rates of major adverse cardiovascular and cerebrovascular events (MACCE) over the course of 30 days, which were 4.94% in the rule-in group, 0.0% in the observation group, and 0% in the rule-out group. In the observation group, we identified some cases which demonstrated recurrence of unstable angina (UA) upon reviewing the patients’ medical history, and these recurrences were attributed to the severity of coronary artery disease. Over a 2-year period, MACCE rates were 17.28% in the rule-in group, 9.8% in the observation group, and 1.08% in the rule-out group. After 3 years, the cumulative event rates were 18.52%, 11.76%, and 1.61% in the three groups respectively. Remarkably, only two all-cause non-cardiovascular related deaths were recorded in both the rule-in and rule-out groups. These findings agree with those of previous studies (Fig. 6).
Seventh, currently, most of the previous studies related to the 0/1 h algorithm have focused on the European and American populations; thus, there is a paucity of experimental data in the Chinese and Asian populations. In this article, we established cut-off values appropriate for the Chinese population. When we compared the AnZhen 0/1h-algorithm with the ESC 0/1 h algorithm, the AnZhen 0/1h-algorithm demonstrated superior performance based on the NPV, PPV, sensitivity and specificity. We believe the difference between the two cut-off values depends on ethnic differences. A previous study focused on 99th URL in a Korean population using the Beckman Coulter Access hsTnI, and the results showed that the 99th percentile URLs were 9.5 ng/L (90% CI 7.4–14.9), 7.8 ng/L (90% CI 5.5–19.2 ng/L), and 11.3 ng/L (90% CI 8.0–15.7 ng/L) in healthy participants, women and men, respectively, which were lower than the manufacturer’s claims28. However, in an American population, the Beckman Coulter Access hsTnI assay demonstrated the same 99th percentile URLs as the manufacturer’s claims29. In the previous study focus on Korean population, the researchers proposed the 99th percentile URL for Asian population might be lower than the standard established for Europeans, both of them used he Beckman Coulter Access hsTnI, however, it hadn’t explore the possible reasons behined ethnic furthermore. An other research based on Chinese populations using the VITROS hs-cTnI assay reported a 99th percentile URL lower than both the manufacturer-specified threshold and the threshold commonly used for US populations30. We considered that these observed variations could stem from differences in the physiological characteristics of the reference populations enrolled in these studies. The significant cultural and physiological differences across ethnic groups highlight the need for further systematic investigation. Secondly, many references have observed different 99th percentile URLs based on age and gender, and studies on the 0/1 h algorithm in foreign populations have utilized cohorts with varying mean ages15,31. Due to the conflicts among different populations, we aimed to identify the optimal cut-off values for a Chinese population.
The common use of high-sensitivity troponin has set off much confusion about whether it can cause unnecessary worries, over-testing, or treatments, whereas studies have shown that hs-cTn does not lead to an increased rate of coronary angiography, coronary CT, plate tests, and other tests14. The correct interpretation of high-sensitivity troponin is quite important. The 0/1 h diagnostic algorithm is the preferred rapid screening procedure, and the balance of the negative predictive value, sensitivity, and validity must be considered when determining the cut-off value. Although the exclusion criteria included “ chest pain symptoms present for more than 3 h and 0 h < 3 pg/mL”, the final diagnosis needs to be combined with the clinical data and all other clinical information. Additionally, a repeat test at 3 h after presentation is necessary, especially for the patients who were classified into observed group, to avoid missed diagnoses (for example, due to the delayed release of hs-cTn into the circulation)32.
This study also had some limitations. First, the sample size of this experiment was small, although all samples were collected from three chest pain center platforms. In our subsequent related research, we will further expand the sample size. Second, renal function was independent of the outcome; only patients with terminal renal failure on chronic dialysis were excluded. However, the effects of terminal renal failure on hs-cTnI levels need to be further explored18. Third, the final diagnosis of the study was determined using coronary angiography or CCTA, an unavoidable problem in some of the patients who underwent CCTA was the presence of artifacts in the report of some coronary lesions, so our final diagnostic interpretation of the patients depended on the combined clinical presentation, not just rely on CAG or CCTA, therefore, the interventions for the patients were selected based on comprehensive judgment. Fourth, several large cohort studies have explored the diagnostic efficacy of the 0/1 h process in post-CABG patients33 and found that poor diagnostic power correlated with changes in baseline hs-cTnI levels in post-CABG patients. Further studies should focus on the post-CABG effects. Finally, this study established a 0/1 h process for the Chinese population. The applicability of the 0/1 h diagnostic performance in patients presenting >12 h after the onset of chest pain symptoms was also considered in large multicenter studies abroad34 and it was concluded that the 0/1 h process applies to both early and late presentations, and this is something that we will consider further refining.
In the course of this trial, the AnZhen 0/1h-algorithm demonstrated its effectiveness in accurately diagnosing and ruling out patients suspected of having NSTEMI among the Chinese population. It notably achieved higher levels of NPV and PPV when compared to the ESC 0/1 h algorithm. This straightforward algorithm has the potential to enhance treatment rates while avoiding unnecessary invasive procedures and prolonged observation periods. Simultaneously, it holds the promise of conserving valuable medical resources and reducing patient costs.
However, to further validate the safety and efficacy of this new 0/1 h algorithm tailored to the Chinese population, additional multicenter experiments with larger sample sizes are essential. These endeavors will provide a more comprehensive assessment of its performance across diverse clinical settings and patient demographics.
Methods
Study design
We conducted a prospective, multi-center, longitudinal study from 2017 to 2024 at Beijing Anzhen Hospital, The second hospital of Jilin University and Shanxi Cardiovascular Hospital. During this period, we consecutively recruited patients (aged 18–80 years) who presented to the ED with non-traumatic chest pain. The main inclusion criteria were as follows: i) patients who experienced any acute chest pain or angina pectoris symptoms presenting within 12 h before hospitalization; ii) patients who experienced any acute chest pain or angina pectoris peak within 12 h before hospitalization; and iii) all subjects who provided informed consent from the patient or family. The main exclusion criteria were as follows: i) patients with ST-segment elevation on ECG; ii) pregnant women; iii) patients with comorbid tumors; iv) patients whose clinical information and final clinical diagnoses were incomplete and uncertain; and v) patients with terminal renal failure on chronic dialysis. This study was approved by the Medical Ethics Committee of all three hospitals, and all patients and their families provided written informed consent before study enrollment (ClinicalTrials.gov registry number NCT03331549).
Baseline data collection
After enrollment, the baseline information recorded included age, sex, smoking history, medical history, family history of heart disease, D-dimer levels, high-sensitivity troponin I level, 12-lead ECG, and coronary angiography/coronary computed tomographic angiography (CCTA). All baseline information was gathered through real-time medical history collection. All laboratory and ancillary test results were interpreted in accordance with the appropriate disease diagnosis and treatment guidelines. The ECG and coronary angiography/CCTA results were interpreted independently by two senior cardiologists, with a third specialist in case of disagreement.
Detection of hs-cTnI
Blood samples were drawn from all patients with suspected NSTEMI immediately at the time of presentation (0 h) and 1 h after presentation to measure hs-cTnI-Access levels. The samples were collected in tubes containing anticoagulants and serum retained at –80 degrees.
The high-sensitivity troponin assay was conducted using a DxI800 fully automatic immunoassay analyzer (Beckman Coulter, Access hs-cTnI, Beckman Coulter, Inc. Brea, CA, USA) with a dedicated accessory kit35. Access hs-cTnI exhibited a 99th percentile concentration of 18 pg/mL (females, 12 pg/mL; males, 20 pg/mL), with a corresponding CV of <5%. The limit of the blank and the limit of detection were determined to be 1.7 pg/mL and 2.3 pg/mL, respectively. All samples were tested in a blinded laboratory.
Determination of the final diagnoses
The final diagnoses of all patients with suspected NSTEMI were determined by the Chest Pain Center within the Emergency Department at Beijing AnZhen Hospital. The diagnostic process for acute myocardial infarction and the interpretation of high-sensitivity troponin assay results adhered to the latest Fourth Universal Definition guidelines36. In brief, acute myocardial infarction was diagnosed when there was evidence of myocardial necrosis accompanied by symptoms of myocardial ischemia. Myocardial necrosis was defined as a high-sensitivity troponin level exceeding the 99th percentile of the normal population on at least one occasion, coupled with a significant elevation or reduction (a change of ≥30% from the 99th percentile was deemed significant). It is worth nothing that coronary angiography or CCTA served as the gold standard for myocardial infraction diagnosis37,38,39. Among the patients, a total of 244 underwent coronary angiography, and 125 patients underwent CCTA. Other clinical diagnoses were determined based on established clinical expertise and relevant guidelines. The final diagnoses were defined as “NSTEMI”, “UA (unstable angina)”, “Cardiac but not ACS (cardiac related diseases excluding acute coronary syndrome, e.g. stable angina)” and “Non-Cardiac (non-cardiac related diseases, e.g. intercostal neuralgia, pneumonia and so on)” based on the results of coronary angiography or CCTA and other historical and laboratory test results.
Patients were categorized into three groups, namely the “Exclusion” group, the “Inclusion” group, and the “Observation in Hospital” group, based on the consensus reached by cardiologists through thorough review of all medical records from the patient’s initial visit to the emergency department. In cases where the two independent cardiologists disagreed, a third cardiologist, not involved in the patient’s clinical management, independently adjudicated the diagnosis.
Follow-up
After hospital discharge, patients were contacted by telephone at 1, 3, 12, 24 and 36 months, and the primary prognostic endpoints were major adverse cardiovascular and cerebrovascular events (MACCE), which included cardiovascular death, all-cause mortality, nonfatal myocardial infarction, refractory angina, new onset heart failure and stroke, at 30, 720 and 1080 days.
Statistical methods
Statistical analysis of the test data was performed using IBM SPSS Statistics for Windows (version 27.0, SPSS Inc., Chicago, IL) and R Software (version 4.3.1). All measures were tested for normality by the Sharpiro–Wilk test, and data conforming to a normal distribution were expressed as x ± s, with independent sample t-tests for normally distributed samples and non-parametric tests for non-normally distributed samples. Bonferroni correction was adopted when analyzing comparisons among multiple AUC values. All measures were expressed as frequencies and percentages, and trends in event rates were assessed using the χ2 test.
Receiver operating characteristic (ROC) curves were drawn, and the inclusion and exclusion cutoff point values in the 0 h/1 h rule were calculated. This included calculating both troponin cutoff(s) and troponin delta cutoffs (s). The corresponding sensitivity, specificity, positive prediction rate, negative prediction rate, and other statistical parameters were provided. Differences were considered statistically significant at P < 0.05. Using the classification and regression tree (CART) method, the cutoff values for the excluded diagnoses met the minimum indicators: 99.5% NPV for rule-out, 99% sensitivity, and 70% for rule-in, to establish a suitable 0 h/1 h process cut-off value for the Chinese population40. Derived rule-in thresholds were obtained based on the CART analysis, which targeted a minimum positive predictive value (PPV) of 70%. If the predefined target performance was not achieved in the derivation sample using the CART-derived thresholds, the thresholds were changed stepwise (by) until the predefined performance was achieved. The optimal rule-out thresholds were selected based on integer increases from the hsTnI assay’s LOD, and the optimal rule-in thresholds were selected based on 5-fold integer decreases from the hsTnI assay’s 99th URL.
MACCE occurring during the 30-day, 2-year, and 3-year follow-up period, as classified by the AnZhen 0/1 h algorithm, were plotted using Kaplan–Meier curves, and the log-rank test was used to assess differences in cumulative events between the three groups.
Application of the 0/1 h algorithm for ESC recommended cut-off values
We employed the 0/1 h algorithm cut-off values recommended by the 2020 ESC NSTEMI guidelines to evaluate performance41. These measurements were conducted using Beckman’s latest high-sensitivity troponin assay kit (Access hs-cTnI). The selected rule-in cut-off value was 0 h ≥ 50 pg/mL or Δ1h ≥ 15.0 pg/mL, while the rule-out cut-off value was 0 h < 4 pg/mL or 0 h < 5 pg/mL and Δ1h < 4.0 pg/mL.
Determination of cut-off values suitable for Chinese populations
Utilizing the classification and regression tree (CART) method, we determined the cut-off values for the excluded diagnoses while adhering to specific criteria: achieving a minimum of 99.5% negative predictive value (NPV) for Rule-out, maintaining a sensitivity of 99%, and ensuring a rule-in rate of at least 70%. These criteria were integral in establishing suitable cut-off values for the 0/1 h algorithm tailored to the Chinese population40. The decision values, optimized in the process establishment cohort, were rounded to integer values measured in ng/L. We also cross-referenced these candidate thresholds with data from the ROC analysis. In instances where the cut-off values derived through CART did not initially meet the predefined target performance, we made incremental adjustments to the thresholds until the desired performance criteria were attained. The development of the hs-cTnI-Access 0/1 h algorithm was carried out using a cohort consisting of all patients who had access to hs-cTnI measurements at both ED presentation and 1 h later.
Data availability
The raw data supporting the conclusions of this article will be made available by the authors without undue reservation. For privacy reasons, the data are not publicly available. Data are available from the corresponding author (contact email address: hxndoctor@126.com) upon reasonable request and with permission from the Medical Ethics Committee of Beijing AnZhen Hospital.
References
Puymirat, E. et al. Acute myocardial infarction: changes in patient characteristics, management, and 6-month outcomes over a period of 20 years in the FAST-MI program (french registry of acute ST-elevation or non-ST-elevation myocardial infarction) 1995 to 2015. Circulation 136, 1908–1919 (2017).
Chin, C. T. et al. Characteristics and outcomes of medically managed patients with non-ST-segment elevation acute coronary syndromes: Insights from the multinational EPICOR Asia study. Int. J. Cardiol. 243, 15–20 (2017).
Shah, A. S. V. et al. High-sensitivity troponin in the evaluation of patients with suspected acute coronary syndrome: a stepped-wedge, cluster-randomised controlled trial. Lancet 392, 919–928 (2018).
Chapman, A. R. et al. Comparison of the efficacy and safety of early rule-out pathways for acute myocardial infarction. Circulation 135, 1586–1596 (2017).
Chapman, A. R. et al. Novel high-sensitivity cardiac troponin I assay in patients with suspected acute coronary syndrome. Heart 105, 616–622 (2019).
Wildi, K. et al. Safety and efficacy of the 0 h/3 h protocol for rapid rule out of myocardial infarction. Am. Heart J. 181, 16–25 (2016).
Greenslade, J. H. et al. Widespread introduction of a high-sensitivity troponin assay: assessing the impact on patients and health services. J. Clin. Med. 9, 1883 (2020).
Twerenbold, R. et al. Prospective validation of the 0/1-h algorithm for early diagnosis of myocardial infarction. J. Am. Coll. Cardiol. 72, 620–632 (2018).
Boeddinghaus, J. et al. High-sensitivity cardiac troponin I assay for early diagnosis of acute myocardial infarction. Clin. Chem. 65, 893–904 (2019).
Nestelberger, T. et al. Two-hour algorithm for rapid triage of suspected acute myocardial infarction using a high-sensitivity cardiac troponin I assay. Clin. Chem. 65, 1437–1447 (2019).
The Writing Committee Of The Report On Cardiovascular Health And Diseases In China Report on Cardiovascular Health and Diseases in China 2022: an Updated Summary. Biomed. Environ. Sci 36, 669–701 (2023).
Rubini Giménez, M. et al. Rapid rule out of acute myocardial infarction using undetectable levels of high-sensitivity cardiac troponin. Int. J. Cardiol. 168, 3896–3901 (2013).
Keller, T. et al. Serial changes in highly sensitive troponin I assay and early diagnosis of myocardial infarction. JAMA 306, 2684–2693 (2011).
Twerenbold, R. et al. Impact of high-sensitivity cardiac troponin on use of coronary angiography, cardiac stress testing, and time to discharge in suspected acute myocardial infarction. Eur. Heart J. 37, 3324–3332 (2016).
Mueller, C. et al. Multicenter evaluation of a 0-hour/1-hour algorithm in the diagnosis of myocardial infarction with high-sensitivity cardiac troponin T. Ann. Emerg. Med. 68, 76–87.e4 (2016).
Jaeger, C. et al. One-hour rule-in and rule-out of acute myocardial infarction using high-sensitivity cardiac troponin I. Am. Heart J. 171, 92–102.e1 (2016). 5.
Pretorius, C. J., Tate, J. R., Wilgen, U., Cullen, L. & Ungerer, J. P. J. A critical evaluation of the Beckman Coulter access hsTnI: analytical performance, reference interval and concordance. Clin. Biochem. 55, 49–55 (2018).
Twerenbold, R. et al. 0/1-hour triage algorithm for myocardial infarction in patients with renal dysfunction. Circulation 137, 436–451 (2018).
Koechlin, L. et al. Performance of the ESC 0/2h-algorithm using high-sensitivity cardiac troponin I in the early diagnosis of myocardial infarction. Am. Heart J. 242, 132–137 (2021).
Boeddinghaus, J. et al. Early diagnosis of myocardial infarction with point-of-care high-sensitivity cardiac troponin I. J. Am. Coll. Cardiol. 75, 1111–1124 (2020).
Haller, P. M. et al. Performance of the ESC 0/1-h and 0/3-h algorithm for the rapid identification of myocardial infarction without ST-elevation in patients with diabetes. Diabetes Care 43, 460–467 (2020).
Park, K. C., Gaze, D. C., Collinson, P. O. & Marber, M. S. Cardiac troponins: from myocardial infarction to chronic disease. Cardiovasc. Res. 113, 1708–1718 (2017).
McCarthy, C. P. et al. Myocardial injury in the era of high-sensitivity cardiac troponin assays: a practical approach for clinicians. JAMA Cardiol. 4, 1034–1042 (2019).
Januzzi, J. L. Jr et al. Recommendations for institutions transitioning to high-sensitivity troponin testing: JACC Scientific Expert Panel. J. Am. Coll. Cardiol. 73, 1059–1077 (2019).
Schmid, J. et al. Elevated cardiac troponin T in patients with skeletal myopathies. J. Am. Coll. Cardiol. 71, 1540–1549 (2018).
Mair, J. et al. How is cardiac troponin released from injured myocardium?. Eur. Heart J. Acute Cardiovasc. Care 7, 553–560 (2018).
Shave, R. & Oxborough, D. Exercise-induced cardiac injury: evidence from novel imaging techniques and highly sensitive cardiac troponin assays. Prog. Cardiovasc. Dis. 54, 407–415 (2012).
Kim, S., Yoo, S. J. & Kim, J. Evaluation of the new Beckman Coulter Access hsTnI: 99th percentile upper reference limits according to age and sex in the Korean population. Clin. Biochem. 79, 48–53 (2020).
Christenson, R. H. et al. Analytical and clinical characterization of a novel high-sensitivity cardiac troponin assay in a United States population. Clin. Biochem. 83, 28–36 (2020).
He, B. et al. Determination of age- and sex-specific 99th percentile upper reference limits for high-sensitivity cardiac troponin I in healthy Chinese adults. Cardiology 147, 261–270 (2022).
Reichlin, T. et al. One-hour rule-out and rule-in of acute myocardial infarction using high-sensitivity cardiac troponin T. Arch. Intern. Med. 172, 1211–1218 (2012).
Pickering, J. W. et al. Early kinetic profiles of troponin I and T measured by high-sensitivity assays in patients with myocardial infarction. Clin. Chim. Acta. 505, 15–25 (2020).
Koechlin, L. et al. Lower diagnostic accuracy of hs-cTnI in patients with prior coronary artery bypass grafting. Int. J. Cardiol. 354, 1–6 (2022).
Boeddinghaus, J. et al. Diagnostic performance of the European Society of Cardiology 0/1-h algorithms in late presenters. J. Am. Coll. Cardiol. 77, 1264–1267 (2021).
Badertscher, P. et al. Direct comparison of the 0/1h and 0/3h algorithms for early rule-out of acute myocardial infarction. Circulation 137, 2536–2538 (2018).
Thygesen, K. et al. Fourth universal definition of myocardial infarction (2018). J. Am. Coll. Cardiol. 72, 2231–2264 (2018).
Sandoval, Y. et al. High-sensitivity cardiac troponin and the 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guidelines for the evaluation and diagnosis of acute chest pain. Circulation 146, 569–581 (2022).
Aakre, K. M. et al. Analytical considerations in deriving 99th percentile upper reference limits for high-sensitivity cardiac troponin assays: educational recommendations from the IFCC Committee on Clinical Application of Cardiac Bio-Markers. Clin. Chem. 68, 1022–1030 (2022).
Boeddinghaus, J. et al. Clinical validation of a novel high-sensitivity cardiac troponin I assay for early diagnosis of acute myocardial infarction. Clin. Chem. 64, 1347–1360 (2018).
Roffi, M. et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur. Heart J. 37, 267–315 (2016).
Collet, J.-P. et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur. Heart J. 42, 1289–1367 (2021).
Acknowledgements
Xiaonan He was supported by the foundation of the National Natural Science Foundation of China (No.62272327).
Author information
Authors and Affiliations
Contributions
J.C. and X.H. were responsible for designing the study. H.Y. provided the laboratory testing condition. Q.G. and X.L. conducted statistical analyses and interpretations. J.C. wrote the manuscript. J.C., J.S., K.S., B.W., and S.Z. contributed to data collection and follow-up. All authors have revised the manuscript and approved the final version. X.H. provided the sponsorship for this article and oversaw the integrity and accuracy of the data analysis.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, J., Yuan, H., Geng, Q. et al. A rapid 0/1 h algorithm for suspected non-ST-segment elevation myocardial infarction using high-sensitivity cardiac troponin I. npj Cardiovasc Health 2, 47 (2025). https://doi.org/10.1038/s44325-025-00080-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s44325-025-00080-8