Abstract
Massive hemorrhage remains the primary cause of potentially preventable death in traumatic injuries. Monitoring hemorrhage and resuscitation accurately can improve outcomes but continues to be challenging since traditional vital signs are highly compensated by the body. Previous work has developed physiologically interpretable algorithms to assess volume status in simulated models of hemorrhage and resuscitation. In this paper, we further develop these algorithms to assess volume status in a nonhuman primate model of controlled blood loss and subsequent whole-blood resuscitation. We acquired arterial blood pressure (ABP) waveform data on 12 adult male baboons during a step-and-hold protocol for hemorrhage and a constant resuscitation rate. A gradient-boosted regression tree model trained on only the ejected-wave pulse area (EWPA) feature yielded a 19% root-mean-square-error (RMSE), 0.71 R2, and an area under the receiver operating characteristic curve of ≥ 0.9 for key operating points of volume status. The performance of this model with a single feature compares well to results reported previously from single-feature machine-learning (ML) models as well as more complex machine learning models that are difficult to interpret and computationally intensive. This study is the first investigation of these physiologically interpretable models on invasively measured ABP waveforms.
Similar content being viewed by others
Introduction
Massive hemorrhage remains the leading cause of potentially preventable death in traumatic injuries in both civilian and military contexts1,2,3,4,5. It is the main cause of lost years of life and lost productivity in the U.S., with 214,000 deaths and 2,800,000 hospitalizations in 2015 alone5. Monitoring hemorrhagic blood loss and subsequent fluid resuscitation is key to improving survivability at point of injury6. Standard assessment of hemorrhagic shock and blood reducing volume status in pre-hospital environments remains imprecise, relying on qualitative assessments related to subjective assessments of altered mental status and manual palpating of radial pulse7. Vital signs such as heart rate (HR) and systolic blood pressure (SBP) and their derivatives such as shock index (SI) are used to monitor for shock when available7,8,9,10,11. However, these measures have low sensitivity to monitor shock due to the body’s compensatory response11,12. In addition, it becomes difficult to provide goal-directed resuscitation since hemodynamic status cannot be accurately monitored. Poorly defined resuscitation endpoints can degrade coagulation, and increase toxicity and reperfusion injuries, resulting in increased morbidity and mortality3,12. Furthermore, over-resuscitation can potentially cause even more damaging outcomes than those from under-resuscitation13. Thus, monitoring blood volume and differentiating between states of near-shock and normovolemia is key to potentially saving more lives with pre-hospital trauma care.
Previous literature documents extensive exploration of noninvasive physiological signals to detect the various phases of compensated shock during hemorrhage and resuscitation. Arterial blood pressure (ABP) waveforms11,12,14,15,16, detection of dynamic light scattering17, and seismography8,12 are a few modalities that have shown promise. The ABP waveform is impacted by changes in cardiac output and compensatory mechanisms during hypovolemia and is thus an informative signal. The compensatory reserve13 is a machine learning (ML) algorithm that takes ABP waveform features as inputs and has shown high performance in monitoring both hemorrhage and resuscitation12,18,19. Compensatory reserve is a measure of the body’s capacity to respond to acute decreases in blood volume and its ability to activate compensatory mechanisms such as tachycardia and vasoconstriction18,20.
Two foundational algorithms have been explored in previous work for estimating compensatory reserve. The first is the Compensatory Reserve Index (CRI). CRI employs traditional machine learning21 and measures compensatory reserve on a scale of 1 (normovolemia) to 0 (decompensation). The second is the Compensatory Reserve Metric (CRM). CRM employs a deep learning approach with a convolutional neural network (CNN)22 and is reported on a scale of 100% (normovolemia) to 0% (decompensation).
Monitoring resuscitation has not been as rigorously explored as monitoring hemorrhage in the literature. Convertino et al. observed strong correlations between CRM and both hemorrhage and blood resuscitated in nonhuman primates. They determined a systemic critical oxygen delivery threshold and corresponding resuscitation target of 40% CRM3,19. Li et al. showed the capability of tracking resuscitation in a porcine model of hemorrhagic shock and fluid resuscitation based on an ML model with electrocardiogram (ECG) and photoplethysmogram (PPG) waveform features as inputs13. The resulting algorithm achieved a resuscitation target with receiver operating characteristic (ROC) area under curve (AUC) of 0.95 with an individualized baseline, degrading to 0.89 without baseline. Most recently, Gupta et al. tested a customized machine learning algorithm with physiologically interpretable features on a simulated human model of hemorrhage followed by resuscitation and showed coefficients of determination as high as 0.85, and AUCs > 0.9 for most feature sets tested23. This result showed the ability to accurately track hemorrhage and resuscitation in a simulated model of hemorrhage.
This paper builds upon this previous work by assessing the value of ABP-derived features to monitor blood volume status during both hemorrhage and resuscitation in a non-human primate (NHP) model of controlled bleeding, thereby revealing further insights on the physiological information embodied in ABP waveforms. The resulting models provide physiological insight when estimating CRM in contrast to the CRM method previously reported by Convertino et al.21. The main contributions of this paper are: (1) these physiologically meaningful models provide comparable accuracy for monitoring controlled blood loss and resuscitation compared to more complicated models that are difficult to physiologically interpret, (2) evaluation of a new feature correlating with stroke volume that was found to be highly important, and (3) the first investigation of these physiologically interpretable models on invasively measured ABP waveforms.
Results
Performance of CRM estimation models
We collected data from twelve adult baboons under sedation. A solid-state vascular catheter with pressure transducers (Millar, Pearland TX USA) placed in the axillary artery acquired arterial blood pressure (ABP) waveforms. Additional catheters were placed in the femoral vein and artery to remove and replace blood. ABP, electrocardiogram (ECG), heart rate (HR), and central venous pressure (CVP) were recorded continuously at 500 Hz.
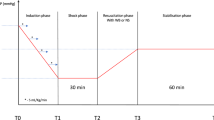
The timing sequence for the hemorrhage and resuscitation protocol is shown in Fig. 1. Baseline values were monitored for 20 min prior to beginning stepwise hemorrhage. The baboons were hemorrhaged to steps of 6.25%, 12.5%, 18.75%, and 25% of total blood volume. Blood was withdrawn via reversed infusion pump at a rate of 50 ml per minute. Each hemorrhage step was held for 7 min. A systolic blood pressure of 70 mmHg was set as an a priori protocol termination minimum threshold. After the last 7 min step at 25% hemorrhage, blood was replaced at a rate of 50 ml per minute. Hemodynamic variables were then allowed to stabilize for 20 min. If a subject did not reach 25% blood-loss due to the early termination protocol, it was classified as low tolerance (LT). Completion of the full experiment resulted in a high tolerance (HT) classification. After recovering from sedation, we returned the baboons to their home cage and monitored return to normal feeding and drinking.
Representative controlled hemorrhage protocol (%) and reference CRM values (%) plotted against time (minutes) during the baseline (green shaded panel), hemorrhage (yellow shaded panel), resuscitation (purple shaded panel), and recovery phases (red shaded panel) of the experiments. The blue line represents the percentage of total blood volume drained for a subject and the red line is the calculated CRM value used as the ground truth for training.
We computed each subject’s reference CRM values based on percentage of blood volume removed, \(B\), at each time point, \(t\), following Eq. (1) as illustrated in Fig. 1, where \({B}_{\max }\) is the maximum blood loss experienced by the subject:
The Reference CRM values plotted in Fig. 1 served as ground truth to train and test our ML models to estimate CRM. Further details on the animal experiments (e.g., baseline vitals) that contributed to the dataset used the present study may be found in the work by Koons et al3. and Hinojosa-Laborde et al.24.
We identified key points on the ABP waveform and derivatives, following Elgendi25. From these key points, features that reflect key physiological parameters were computed from the Table 1 formulas25. These features capture meaningful physiological markers such as cardiac output, autonomic function, and peripheral vascular resistance14,18,24,26,27,28. Standard vital signs such as HR, SBP, and DBP were also included as key features. The half-rise to dicrotic notch feature (HRDN) has shown high accuracy in predicting CRM in previous work23,26 and was included for this analysis. We also included an additional feature called the ejected-wave pulse area (EWPA) in the analysis as this feature has been shown to correlate to stroke volume (SV) as a possible way to capture further information about cardiovascular and hemodynamic changes induced by the hemorrhage experiment29.
Following the approach outlined in our previous work23, we formulated CRM estimation as a supervised regression problem employing ABP-derived features as input variables. The gradient boosted (GB) regression tree30 model was the primary model used. We assessed five separate feature groupings: 1) all features listed in Tables 1, 2) the vital sign features (PPI, HRV, SBP, DBP, and SI), 3) ABP-waveform specific features (PPI, HRDN, PP, EWPA, and IPA), 4) HRDN only, and 5) EWPA only. The dimension of the data was thus 1 – 10 features, with a total of 24,160 feature vectors for the 12 subjects.
We trained models with and without baseline normalization and evaluated generalizability using five-fold cross validation. We split training folds by subject in order to avoid data leakage31 since samples from a single subject are highly correlated. This resulted in 9-subject training sets and 2- or 3-subject test sets in each of the five folds. We used Python’s scikit-learn package for machine learning for all regression experiments28. We trained and tested models on 1) the full procedure: this included baseline, hemorrhage, resuscitation, and recovery sections of the experiment, 2) hemorrhage: this included only hemorrhage data (yellow-shaded section in Figs. 1), and 3) resuscitation: this included only resuscitation data (purple-shaded section in Fig. 1). In all, we trained and tested 30 models and a combination of 5 feature sets, 3 data segments (full, hemorrhage, resuscitation), and 2 classifiers (least squares and GB tree). We followed the framework of performance assessment presented in our previous work23,26 and quantified model accuracy by root-mean-square error (RMSE), coefficient of determination (R2), and ROC AUC. We computed ROCs at the clinically relevant CRM thresholds of 40% and 70%, following Koons et al.19.
Tolerance to hypovolemia also plays an important role in determining a subject’s hemodynamic response to hypovolemia. Low tolerant (LT) individuals undergo decompensation in less time than high tolerant (HT) individuals for the same level of blood loss32. RMSE and R2 were compared between the LT and HT groups to determine if there was a difference in a model’s accuracy on the two kinds of hemodynamic responses to hypovolemia.
Table 2 details accuracies for a gradient-boosted (GB) tree model trained and tested with five sets of features on the full procedure, hemorrhage phase, and resuscitation phase as shown in Fig. 1.
For the isolated hemorrhage and resuscitation segment results, only a subset of the feature sets is shown for comparison since the same trends were observed as in the full protocol. A full table with all feature set results can be found in the supplementary information, Supplementary Table S1. The three highest performing models (lowest RMSE and highest R2) for the full procedure are: 1) the GB tree trained on all features with baseline normalization (RMSE = 18% ± 5%, R2 = 0.72 ± 0.15), 2) the EWPA feature with no baseline normalization (RMSE = 19% ± 3%, R2 = 0.71 ± 0.11), and 3) vital signs with baseline normalization (RMSE = 19% ± 4%, R2 = 0.0.69 ± 0.16). Certain cases show improvement when just trained on the hemorrhage segment. The EWPA only model without any baseline normalization shows the highest performance of any model (RMSE = 13% ± 3%, R2 = 0.79 ± 0.09) when just trained on the hemorrhage data.
Baseline normalization led to performance improvements in models utilizing the full feature set, vital signs, and ABP waveform-derived features. In contrast, feature sets employing single features showed no notable enhancement after baseline normalization. The GB tree models using the EWPA feature exhibited a slight decline in performance following baseline normalization across all evaluated protocol phases.
Table 3 shows the RMSEs and R2 broken down by tolerance groups. There were 6 LT and 6 HT subjects. EWPA performs well for both tolerance groups in all cases regardless of baseline. For this dataset, HRDN does not perform well, particularly in the LT case. On average, HT RMSE is 0.04 lower than LT, and the HT group has an R2 that is 0.19 higher than the LT group, however these differences were not statistically significant due to the small number of subjects available for comparison.
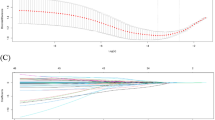
Figure 2 presents a comparison of the relative importance of all evaluated features in the gradient boosting tree models, assessed without baseline normalization, for each phase of the dataset (full data set, hemorrhage-only, resuscitation-only). EWPA was identified as the most important feature in all cases. The Gini importance is insightful but must be interpreted cautiously because it is affected by correlations between features. Still, in this case, it is consistent with the Table 2 results.
Gini importance (unitless value from 0-1) plotted for all ten features tested (Table 1) for the full procedure (blue bars), hemorrhage phase (red bars), and resuscitation phase (yellow bars), comparing relative feature importance. The data for these plots are from the GB tree model trained using all features and without baseline normalization.
Figure 3a shows a Bland-Altman (BA) plot across all subjects. Figure 3b shows an example subject’s reference and estimated CRMs for the GB tree model trained on the full procedure, incorporating all 10 features in Table 1. The limits of agreement (±1.96 standard deviations) were 35-40%. The model bias correlated negatively with CRM, undershooting for higher CRMs and overshooting for lower CRMs, typical for a least-square model. This is observed in Fig. 3b, which shows example CRM estimates during the time course of the experiment (subject 15). Plots of the predicted CRM and true CRM for all subjects for the EWPA only model can be found in the supplementary information, Supplementary Figures S2 and S3. CRM estimates were qualitatively similar for all subjects except for subject 9, for which performance remains to be explained.
a A Bland-Altman plot of the predicted CRM value minus the reference CRM value (%) versus the reference CRM value (%) is presented for the GB tree model trained using all features without baseline normalization for all subjects. The lighter blue dots show the errors calculated along individual time points for the data across all subjects, the solid blue line shows the mean error (0.01%), and the red dashed lines indicate the upper and lower limits of agreement (0.35 and -0.38 respectively). b A sample reference CRM (%) and estimated CRM (%) plotted versus time (minutes) using a GB tree model trained with only the EWPA feature from subject 15 without baseline normalization. The blue line is the true CRM (the ground truth being estimated) and the red line is the model’s predicted CRM value. This particular case had an RMSE of 7.5%, which was lower than the overall average.
ROC analysis
Table 4 tabulates AUCs for full protocol results shown in Table 2. We calculated AUCs at clinically relevant CRM thresholds of CRM ≥ 70%, CRM ≥ 40%, and CRM ≥ 5%23. Each model trained and tested using all the feature configurations listed in Table 4 exhibited high ROC AUCs ( ≥ 0.8) for all binary classification tasks. The full set of results is shown in the supplementary information in Supplementary Table S4.
The ROC performance followed the same trends observed from Table 2 RMSE and R2 values. Models with higher AUCs in Table 4 corresponded to lower RMSE and higher R2 values in Table 2. The GB tree model trained on HRDN without baseline normalization yielded the lowest AUC of 0.80 ± 0.07. The EWPA-only models performed comparably to the models trained on other feature combinations, demonstrating the high sensitivity and specificity of this single ABP-derived feature during both hemorrhage and resuscitation in distinguishing between key CRM thresholds.
Discussion
This work builds on previous analyses of physiologically interpretable features for estimating compensatory reserve23,26,33. This earlier work estimated CRM from noninvasively measured ABP waveforms from a lower body negative pressure (LBNP) stepped hemorrhage model26,33 and LBNP ramped hemorrhage and resuscitation model23. The work reported herein is the first to extend these approaches to ABP waveforms invasively measured from a nonhuman primate model of hemorrhage and resuscitation14, with resuscitation having received relatively little attention for CRM. Highlights of the results include CRM accuracies similar to more complex, black box models for hemorrhage (these black box models have not been designed for resuscitation), and an additional highly important feature related to the integrated compensatory mechanisms that control stroke volume25,29,34.
An important strength of this work is the unique data set of actual blood loss and resuscitation from a nonhuman primate with human-like physiology. This strength comes with a limitation of small sample size, which is understandable for NHP experiments. For test results from the full feature set considered, the small number of subjects can result in overfitting in certain cases. R2 is especially sensitive, with large standard deviations in some cases in Tables 2 and 3. The single-feature EWPA results are much less sensitive to overfitting, as expected for a physiologically consistent feature. This is likely due to stroke-volume being the physiological correlate of pulse-area based features as shown in previous literature25,27,28,29,30,34. In addition, the results for the more operationally relevant performance metric of AUC in Table 4 all have small standard deviations, further confirming the importance of the EWPA feature. As a whole, these results confirm the hypothesis that physiologically based features can be extracted from ABP waveforms to estimate compensation status for both blood loss and resuscitation.
It should be noted that the lower performance of training on the resuscitation segments relative to the hemorrhage segments is due to less data available for the resuscitation segments. More time was spent in the hemorrhage phase with each level of percentage blood loss held for 7 minutes. One can see from Fig. 1 that the subject was in the hemorrhage phase for 30 minutes versus in resuscitation for 15 minutes. This ratio remained true for all subjects, meaning resuscitation data available was half of the amount of hemorrhage data on average. In addition, it is also possible that the lower performance may be the result of including data obtained from LT animals who were no longer undergoing compensation by having reached decompensated shock.
As shown in Fig. 3, the model underestimates higher CRMs ( > 50%) and overestimates for lower CRMs ( < 50%). Despite these proportional biases, the ROC AUC performance reported in Table 4 shows high accuracy binary classification at key thresholds of blood loss (all AUCs > 0.9 for the all features and EWPA models without baseline normalization). The final application of this work requires this level of accuracy at these coarse resolution thresholds of differentiation. Future work would look into corrective measures such as regression-based correction in the model to improve the overall RMSE.
Table 5 and Table 6 compare R2 values and RMSEs (when available) of the algorithms trained and tested in this current work to previous work. The results are presented for GB tree models trained and tested on LBNP-hemorrhage or controlled-bleed segments of data in Table 2 and LBNP-resuscitation or controlled whole blood resuscitation for all the experiments. All cases compared here are without any baseline normalization since that is the expected use-case for any pre-hospital applications. The half-rise to inflection-point (HRIP) feature found to be the most important in the work by Bedolla et al33. is equivalent to the HRDN feature used in the work presented here.
With respect to the operationally important AUC, the AUC found by Convertino et al.22 is 0.93 in predicting the onset of decompensated shock (CRM ~ 5%). All feature sets tested in this work achieve greater than 0.9 except for HRDN, with EWPA achieving an AUC of 0.97 when differentiating above and below the 5% CRM threshold. Thus, the ability of the algorithms presented here to differentiate between key thresholds of blood volume status match the highest performance algorithms presented in literature with much simpler single-feature models that are physiologically interpretable.
In an important difference, our current work finds the most important feature to be related to the area under the ABP primary wave (EWPA), whereas our earlier results from the LBNP model found the most important feature to be related to the time difference between primary and reflected wave (HRDN). We hypothesize that HRDN performed poorly on this dataset because of the different measurement location (axillary artery) than for the other cited studies that used a fingertip ABP measurement. The ABP waveform morphology is well known to vary across the body and that results in changes in the primary wave, reflected wave and dicrotic notch. This body location effect is a consideration for both invasive and non-invasive measurement. In addition, the invasive ABP waveform in this study has a more detailed structure than from a noninvasive measurement (Fig. 4). In the previously published LBNP analysis, EWPA had not been considered as a feature. Based on the excellent results from the current analysis, we evaluated EWPA on the LBNP data and found it to be the second most important feature after HRDN, while still yielding high performance metrics of an RMSE of 17 ± 3% and an R2 of 0.73 ± 0.10. EWPA’s high performance for both datasets is an important new insight. Future work should further explore the efficacy of these features and comparing performance between invasive or non-invasive signal acquisition at key points such as the finger, forehead, upper arm, and chest.
The current study presents a novel analysis of a previously collected NHP dataset for blood loss and resuscitation, seeking to maximize the value of that dataset. Building on previous work, this study highlights the importance of the EWPA feature. The single EWPA feature accurately classifies blood loss thresholds and resuscitation targets in these data, without requiring normalizing to a patient’s pre-injury baseline that would be impractical to measure. This accuracy compares favorably to that from complicated deep learning networks. Additionally, the EWPA feature is physiologically interpretable, since the area under the ejected wave correlates with stroke volume. The work presented here furthers the possibility of blood volume status monitoring in pre-hospital settings. Future work looks to expand data collection and acquire signals simultaneously in multiple locations to better understand the relationship between acquisition location and waveform morphology.
Methods
Hemorrhage Model
As reported in by Koons et al.3, we prepared adult male baboons (n = 12) for the experiment. The non-human primate was selected as the model of study because of its similar genetic composition35 and physiological responses to progressive reductions in central blood volume14,26 in comparison with humans in contrast to quadrupedal species that are genetically and physiologically distant from humans35. Basic demographics for the animals are presented in Table 7. The baboons were individually housed in a shared environment with visual and auditory contact with other animals, beginning two weeks prior to the experiments and continuing until one week following the conclusion of the study. They received food twice daily and had unrestricted access to water. The study protocol received approval from the Texas Biomedical Research Institute (San Antonio, Texas) Institutional Animal Care and Use Committee. All procedures adhered to the Animal Welfare Act, its associated regulations, and the guidelines outlined in the Guide for the Care and Use of Laboratory Animals. On the day of the study, each animal was initially anesthetized with intramuscular ketamine at a dosage of 10 mg/kg. Anesthesia was sustained throughout the procedure using intravenous ketamine (10 mg/kg/hr) in combination with diazepam (0.1 mg/kg/hr). Under sterile conditions, two vascular catheters were placed via small incisions to access and visualize the blood vessels. The animals were intubated to enable spontaneous ventilation during the experiment. A Millar solid-state vascular catheter with attached pressure transducers was inserted into the axillary artery to measure arterial and pulse pressure. Central venous pressure (CVP) was monitored using a fluid-filled catheter positioned near the right atrium and connected to a pressure transducer. Additional catheters were inserted into the femoral artery and vein to facilitate blood withdrawal and reinfusion. Electrocardiogram (ECG) leads were attached following catheter placement to allow continuous heart rate (HR) monitoring. At the conclusion of the hemorrhage study, all catheters were removed, and the incisions were closed with sutures. Throughout the procedure, animals remained intubated and breathed spontaneously. They were supplied with medical-grade air supplemented with 40% oxygen, administered through a side-port on the endotracheal tube, which did not interfere with exhalation.
ABP signal processing
We processed ABP signal data using the pipeline presented by Gupta et al.23,26 with modifications to parameters to account for changes in waveform morphology due to invasive blood pressure measurements and the addition of a new feature.
The ABP signals were processed using a zero-phase finite impulse response (FIR) low-pass filter of order 512, with a cutoff frequency set at 8 Hz. To estimate the first and second derivatives, finite difference methods were applied to the filtered ABP waveforms. Subsequently, both the signals and their derivatives were standardized by computing z-scores within a trailing 2-second window. This step was performed to eliminate baseline drift, detrend the data, and normalize amplitude variations.
As shown in Fig. 5, we extracted features from the ABP signal following Elgendi et al.25. Key points including the waveform trough, peak, and dicrotic notch were extracted and used to calculate amplitude and time-based features with physiological correlates. Additional logic was needed when multiple candidate dicrotic notches are detected, or none are detected. These notches are detected based on the first derivative, as described in25. For cases where multiple candidate notches were identified from first-derivative peaks, the maximally prominent peak within a credible time range (5%–40% of PPI based on a heuristic analysis) was selected. We excluded any ABP pulses with no peaks meeting these criteria from analysis. On average, 15% of the peaks were rejected as not having a valid dicrotic notch. This varied widely across subjects and a table showing the distribution of rejected peaks across the various subjects can be found in the supplementary information, Supplementary Table S5.
To eliminate outliers from each feature, we applied a moving median filter across a centered window spanning 20 heartbeats. Data points exceeding three times the scaled median absolute deviation (MAD) from the local median within this window were discarded. The scaled MAD for each set of local feature values, denoted \({\boldsymbol{A}}\), was computed as \({\boldsymbol{1.48}}* {\boldsymbol{median}}(|{\boldsymbol{A}}-{\boldsymbol{median}}({\boldsymbol{A}})|)\) for each sequence, of local feature values36.
To reduce the influence of short-term variability, a trailing moving average filter with a 20-second window and 90% overlap between successive segments was applied to each feature. For the EWPA feature specifically, we also calculated a moving standard deviation of these averaged values using a symmetric window spanning 21 adjacent segments. Any samples where the EWPA standard deviation surpassed a heuristically selected threshold were excluded as part of an additional outlier removal procedure. Because these processing steps involve non-causal operations—requiring access to 20 seconds of future data—a corresponding 20-second reporting delay ensures that the pipeline can operate causally during real-time deployment.
To assess whether prior knowledge of an individual’s normovolemic physiological baseline is necessary, we also computed a set of features normalized to each subject’s baseline. This was done by dividing each feature time series by its average value during the initial 20-minute baseline period (see Fig. 1).
Training, analysis and performance metrics
Each gradient boosting (GB) ensemble was composed of 100 decision trees, trained to minimize the squared error loss. Bootstrap sampling was not used for generating subsets of data for the individual base learners. The number of estimators was held constant across all experiments, as the limited dataset size precluded the use of a separate validation set for hyperparameter tuning.
To assess the relative influence of each feature in the gradient boosting regression tree models, we evaluated Gini importance28. This metric was computed as the normalized reduction in Friedman’s mean squared error (MSE) criterion30 associated with splits involving the feature under consideration.
A Bland-Altman (BA) analysis37 was also performed to assess the level of agreement between the estimated and reference CRMs. Since the true reference values were available from Eq. (1), the reference CRM was used as the x-axis in the BA plots38.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to U.S. Government ownership but are available from the corresponding author on reasonable request.
Code availability
The underlying code for this study [and training/validation datasets] is not publicly available but may be made available to qualified researchers on reasonable request from the corresponding author pending U.S. Department of Defense approval.
References
Eastridge, B. J. et al. Death on the battlefield (2001–2011). J Trauma Acute Care 73, S431–S437 (2012).
Coppola, S., Froio, S. & Chiumello, D. Fluid resuscitation in trauma patients. Curr. Opin. Crit. Care. 20, 444–450 (2014).
Koons, N. J. et al. Tracking DO2 with Compensatory Reserve During Whole Blood Resuscitation in Baboons. Shock 53, 327–334 (2020).
Huang, G. S. & Dunham, C. M. Mortality outcomes in trauma patients undergoing prehospital red blood cell transfusion: a systematic literature review. Int. J. Burn Trauma 7, 17–26 (2017).
Eastridge, B. J., Holcomb, J. B. & Shackelford, S. Outcomes of traumatic hemorrhagic shock and the epidemiology of preventable death from injury. Transfusion 59, 1423–1428 (2019).
Ravi, P. R. & Puri, B. Fluid resuscitation in haemorrhagic shock in combat casualties. Disaster Mil. Medicine 3, 2 (2017).
The Joint Trauma System. Tactical Combat Casualty Care (TCCC) Guidelines. 25 January 2024. Available at: https://deployedmedicine.allogy.net/learner/collections/11/contents/40. Accessed: 10 June 2025.
Mutschler, M. et al. The Shock Index revisited – a fast guide to transfusion requirement? A retrospective analysis on 21,853 patients derived from the TraumaRegister DGU®. Crit. Care 17, R172–R172 (2013).
Liu, J. et al. Automated Analysis of Vital Signs to Identify Patients With Substantial Bleeding Before Hospital Arrival. Shock 43, 429–436 (2015).
Hanna, K. et al. Multicenter Validation of the Revised Assessment of Bleeding and Transfusion (RABT) Score for Predicting Massive Transfusion. World J. Surg. 44, 1807–1816 (2020).
Stewart, C. L. et al. Detection of low-volume blood loss. J Trauma Acute Care 77, 892–898 (2014).
Convertino, V. A. & Koons, N. J. The compensatory reserve: potential for accurate individualized goal-directed whole blood resuscitation. Transfusion 60, S150–S157 (2020).
Li, X., Pinsky, M. R. & Dubrawski, A. Automated Assessment of Cardiovascular Sufficiency Using Non-Invasive Physiological Data. Sensors 22, 1024 (2022).
Hinojosa-Laborde, C. et al. Comparison of compensatory reserve during lower-body negative pressure and hemorrhage in nonhuman primates. 310, R1154–R1159 (2016).
Reljin, N. et al. Detection of Blood Loss in Trauma Patients Using Time-Frequency Analysis of Photoplethysmographic Signal. 2016 IEEE-EMBS Int. Conf. Biomed. Health Informatics (BHI) 118–121 https://doi.org/10.1109/bhi.2016.7455849 (2016).
Techentin, R. W., et al. 1D Convolutional Neural Networks for Estimation of Compensatory Reserve from Blood Pressure Waveforms. 2019 41st Annu. Int. Conf. IEEE Eng. Medicine Biology Soc. (EMBC), 2169–2173 (2019).
Kerpel, A. et al. Evaluation of Miniature Dynamic Light Scattering Technology for the Assessment of Hemodynamic Status During Graded Hemorrhage and Retransfusion in Pigs. Mil. Med. 182, e2056–e2060 (2017).
Convertino, V. A. et al. The Compensatory Reserve For Early and Accurate Prediction Of Hemodynamic Compromise. Shock 45, 580–590 (2016).
Koons, N. J., et al. Identifying critical DO2 with compensatory reserve during simulated hemorrhage in humans. Transfusion https://doi.org/10.1111/trf.16958 (2022).
Moulton, S. L. et al. Running on empty? The compensatory reserve index. J. Trauma Acute Care 75, 1053–1059 (2013).
Convertino, V. A. et al. S. Estimation of individual-specific progression to impending cardiovascular instability using arterial waveforms. J. Appl. Physiol. 115, 1196–1202 (2013).
Convertino, V. A. et al. AI-Enabled Advanced Development for Assessing Low Circulating Blood Volume for Emergency Medical Care: Comparison of Compensatory Reserve Machine-Learning Algorithms. Sensors 22, 2642 (2022).
Gupta, J. F. et al. Noninvasive Monitoring of Simulated Hemorrhage and Whole Blood Resuscitation. Biosensors 12, 1168 (2022).
Hinojosa-Laborde, C. et al. Validation of lower body negative pressure as an experimental model of hemorrhage. J. Appl. Physiol. 116, 406–415 (2014).
Elgendi, M. On the Analysis of Fingertip Photoplethysmogram Signals. Curr. Cardiol. Rev. 8, 14–25 (2012).
Gupta, J. F., Telfer, B. A. & Convertino, V. A. Feature Importance Analysis for Compensatory Reserve to Predict Hemorrhagic Shock. 2022 44th Annu. Int. Conf. IEEE Eng. Medicine Biology Soc. (EMBC), 1747–1752 (2022).
Shaffer, F. & Ginsberg, J. P. An Overview of Heart Rate Variability Metrics and Norms. Frontiers Public Health 5, 258 (2017).
Pedregosa, F., et al. Scikit-learn: Machine Learning in Python. Arxiv (2012).
Liu, S.-H. et al. Classification of Photoplethysmographic Signal Quality with Deep Convolution Neural Networks for Accurate Measurement of Cardiac Stroke Volume. Appl. Sci. 10, 4612 (2020).
Friedman, J. H. Greedy function approximation: A gradient boosting machine. Ann. Statistics 29, 1189–1232 (2001).
Saeb, S. et al. The need to approximate the use-case in clinical machine learning. Gigascience 6, 1–9 (2017).
Hinojosa-Laborde, C. et al. Heart Rate Variability during Simulated Hemorrhage with Lower Body Negative Pressure in High and Low Tolerant Subjects. Front. Physiol. 2, 85 (2011).
Bedolla, C. N. et al. An Explainable Machine-Learning Model for Compensatory Reserve Measurement: Methods for Feature Selection and the Effects of Subject Variability. Bioengineering 10, 612 (2023).
Murray, W. B. & Foster, P. A. The peripheral pulse wave: Information overlooked. J. Clin. Monit. 12, 365–377 (1996).
Convertino, V. A., Koons, N. J. & Suresh, M. R. Physiology of Human Hemorrhage and Compensation. Compr. Physiol. 11, 1531–1574 (2022).
Pearson, R. K. Outliers in process modeling and identification. IEEE T. Contr. Syst. Tech. 10, 55–63 (2002).
Bland, J. M. & Altman, D. G. Statistical Methods for Assessing Agreement Between Two Methods of Clinical Measurement. Lancet 327, 307–310 (1986).
Krouwer, J. S. Why Bland–Altman plots should use X, not (Y + X)/2 when X is a reference method. Stat. Med. 27, 778–780 (2008).
Acknowledgements
Distribution Statement A. Approved for public release. Distribution is unlimited. This material is based upon work supported by the Department of the Air Force under Air Force Contract No. FA8702-15-D-0001. Any opinions, findings, conclusions or recommendations expressed in this material are those of the author(s) and do not necessarily reflect the views of the Department of the Air Force. Jay F. Gupta created the initial codebase that has been modified for this work and is consulted for continued developments. Ryan McKindles provided final edits from a careful review.
Author information
Authors and Affiliations
Contributions
Conceptualization, B.A.T., S.H.A., and V.A.C.; methodology, B.A.T.,., V.A.C., and S.H.A.; software, and S.H.A.; validation, S.H.A; formal analysis, S.H.A, C.H.-L., and B.A.T.; investigation, S.H.A., B.A.T., E.J.S., C.H.-L., and V.A.C.; resources, V.A.C., E.J.S., and B.A.T.; data curation, S.H.A., B.A.T., E.J.S., C.H.-L., and V.A.C.; writing -- original draft preparation, S.H.A., B.A.T., and V.A.C.; writing—review and editing, S.H.A., E.J.S., B.A.T., C.H.-L., and V.A.C.; visualization, S.H.A.; supervision, B.A.T. and V.A.C.; project administration, B.A.T.; funding acquisition, B.A.T., C.H.-L.; All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests. The funders had no role in the design of the study, in the collection, analyses, or interpretation of data, in the writing of the manuscript, or in the decision to publish the results.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Arshad, S.H., Hinojosa-Laborde, C., Snider, E.J. et al. Monitoring of hemorrhage and whole blood resuscitation in non-human primates. npj Biosensing 2, 31 (2025). https://doi.org/10.1038/s44328-025-00049-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s44328-025-00049-8