Abstract
The experience sampling method (ESM) has proven valuable for studying everyday experiences across clinical populations but remains underexplored in dementia. This article assesses feasibility and utility of a smartphone-based ESM study co-designed with dementia stakeholders. Over 10 days, 12 participants with dementia (transdiagnostic, mean age = 62, range 52–72) responded to seven daily notifications assessing their thoughts and affect, and an end-of-day questionnaire on daily life satisfaction and meaning. Feasibility was evaluated via participation/compliance rates, drop-out, completion times, and subjective participation experiences. Data utility was assessed through between-person and within-person variance and intraclass correlation coefficients. The study achieved 80% compliance with no dropouts. Participants reported low burden and positive participation experiences. Data had substantial within- and between-person variability. Our study shows high-intensity smartphone-based ESM can be successfully implemented in targeted dementia subgroups, underscoring its potential to capture real-time subjective experiences and encouraging further ESM adaptation for more diverse dementia populations.
Similar content being viewed by others
Introduction
Recent years have seen an upsurge of interest in methods that capture people’s natural experiences and activities as they go about their daily lives. These methods, often referred to as ambulatory assessment, involve repeated assessments in participants’ everyday environments as opposed to, for example, controlled single assessments in the lab1. Ambulatory assessment encompasses a variety of approaches. For instance, passive mobile sensing uses electronic wearables to automatically record variables like heart rate, skin temperature, and movement, while daily diary methods require participants to complete a diary at the end of each day for a set period. The experience sampling method (ESM)—also known as ecological momentary assessment—asks participants to provide subjective reports on specific variables multiple times a day, for example through their smartphone1,2.
ESM approaches have gained significant popularity in psychology and psychiatry research because of their distinct advantages3. By capturing real-world and real-time experiences directly from the individual, ESM reports offer high ecological validity and reduce recall bias—a common issue in retrospective self-reports, where participants may struggle to accurately remember or summarize past experiences. Moreover, ESM enables researchers to track fluctuations in thoughts and emotions over short time spans and to map out intricate within-person relationships among these variables4,5,6. This approach produces rich, multidimensional data, allowing researchers to uncover complex temporal patterns and contextual dynamics. These insights not only provide unique opportunities to understand and predict individual patterns but also support the development of personalized interventions and treatment7,8.
To better understand the daily experiences of specific groups, ESM approaches have been successfully implemented in both non-clinical and clinical populations. These include young children and adolescents9,10, children with autism spectrum disorder11, different psychopathological groups such as those with mood, anxiety, and psychotic disorders12, and patients with acquired brain injury13,14. Notably, the use of ESM in healthy aging has grown significantly over the past two decades15. These studies have provided valuable insights, for example, into daily activities and their associated levels of physical activity and enjoyment16, and the value of repeated real-life assessments of cognition17 and mental health18. These studies illustrate the potential of ESM in capturing the complexity and variability of aging processes and experiences, which can facilitate early detection of symptoms, identification of protective lifestyle factors, and the development of personalized interventions to enhance late-life well-being.
However, most existing research has excluded participants with a dementia diagnosis15,19, likely due to perceived challenges in implementing these approaches in populations with cognitive difficulties. Practical concerns and preconceptions about the capabilities of people with dementia may raise doubts about the feasibility and validity of ESM in this context. For instance, older adults with dementia may be viewed as less familiar with digital technology, and their cognitive impairments are assumed to hinder their ability to introspect and report on their experiences20,21. Moreover, participating in an ESM study requires substantial time and mental effort, which can be taxing for individuals with cognitive difficulties. These challenges likely explain why most existing studies have relied on passive sensing e.g., ref. 22, or caregiver reports e.g., ref. 23, rather than self-reports from people with dementia. As a result, the potential of ESM to shed light on the daily lives and experiences of people with dementia remains largely untapped. This represents a missed opportunity, as ESM—being less reliant on retrospective memory— may offer a valid and effective method for capturing subjective experiences in individuals with dementia20.
Several pioneering studies suggest that ESM may be feasible for people with dementia under certain conditions. For example, Rullier, et al.19 conducted a study involving farmers over the age of 70 in rural France living with mild cognitive impairment or dementia. They adapted their approach to this population by using landline phone calls to collect verbal responses multiple times daily. Niculescu, et al.24 gathered observational data on depressive symptoms from participants with moderate-to-severe dementia in a specialized dementia unit, incorporating self-reported yes/no items about sadness and worry, which provided meaningful complementary data. These studies demonstrate that ESM methods can be tailored to participants’ abilities, such as through verbal or face-to-face approaches.
Self-administered ESM data collection via digital devices like smartphones offers distinct advantages in terms of convenience and efficient use of time and resources. While the use of electronic devices for ESM has been scarcely applied in dementia research, there are indications of its potential feasibility. As the digital divide between younger and older generations is “rapidly shrinking”25, many people living with dementia are becoming more familiar with screens. For instance, one study found that 75% of patients referred to a memory clinic for a neuropsychological evaluation reported owning a smartphone26. Additionally, studies show that people with dementia can use touchscreens independently and intuitively27 and that people with cognitive impairments, including dementia, value smartphones in their daily lives28. New technologies are also increasingly being leveraged in dementia care, as seen in initiatives developing digital programs to support daily living e.g., ref. 29. Furthermore, while smartphone-based ESM has yet to be widely used to capture psychological experiences like thoughts and feelings in dementia, it has been successfully applied in participants with mild cognitive impairment30,31 and to repeatedly assess cognitive functioning in participants with mild cognitive impairment or very mild dementia32,33. These findings highlight the untapped potential of digital ESM methods to capture the lived experiences of people with dementia in real time.
In sum, while evidence suggests that ESM may be feasible for certain subgroups of people with dementia, no studies to date have demonstrated the feasibility and utility of an intensive smartphone-based ESM approach to repeatedly assess subjective experiences in this population. Here, we report on a 10-day smartphone ESM study with high measurement intensity conducted in a targeted transdiagnostic sample of participants with dementia. Using m-Path, a user-friendly and flexible ESM platform and app34, participants provided repeated self-reports on their momentary mood, ongoing thoughts, and their daily life satisfaction and meaning in life. This article describes in detail our methodological approach, which included a co-design element to engage the opinions and expertise of stakeholders with lived experience of dementia, and evaluates both the feasibility of implementing this methodology and the utility of the data collected. This work aligns with recent calls to better understand the daily experiences of people with dementia and to explore the potential of ESM for capturing these insights20.
Results
Participants
The final sample consisted of 12 participants, 9 of whom were women (75%). Participants had a mean age of 62 years old (SD = 6; range 52–72), which means the study mainly included participants with young-onset dementia. They had on average 13 years of education (SD = 3; range 9–18). Six were retired, two were not working, three worked part-time, and one full-time. Ten participants lived with a spouse or partner, while two lived alone. The sample was transdiagnostic, comprising five participants with Alzheimer’s disease, four with behavioral-variant frontotemporal dementia, and three with semantic dementia. For 11 participants, diagnoses were certain or probable, while 1 was classified as possible. The mean score for the ACE-III cognitive screening tool was 84 (SD = 13, range 53–98), while the mean score for the DAD (functional abilities) was 91 (SD = 14, range 55–100), with a mean sub-score of 89 for instrumental activities of daily living (SD = 18, range 43–100), and the mean score for the FRS (behavioral changes and functional dependence) was 3.20 (SD = 2.41, range −0.02–3.20), reflecting mild to moderate dementia stages.
Feasibility: participation rate, drop-out, compliance rate, and completion times
Of the 23 individuals contacted, 14 agreed to participate (61%), two of whom were eventually not included due to an uncertain diagnosis. Reasons mentioned for not participating were concerns that the study would be too stressful or demanding (n = 3), rapid dementia progression with a move to residential care (n = 2), or being too busy (n = 1). One participant did not provide a reason, and two never responded to the study invitation. There were no dropouts during the study. The mean compliance rate was 80% (SD = 13%, range 54%-91%), with a total of 799 out of 1004 possible measurements completed across participants. As described in the Methods section, certain personalized adaptations were implemented to promote participant compliance. For three participants, the data collection period was extended by one or two days, and for one participant, her partner received synchronized notifications allowing him to remind her to respond. On average, the momentary questionnaires (including the voice recording item) took 2 min and 10 s (SD = 1 min 23 s) to complete, while the end-of-day items took 36 s (SD = 25 s). These times align with the estimated completion times outlined in the study registration (2–3 min for momentary questionnaire and less than one minute for end-of-day items). Compliance had a Pearson correlation of 0.41 (95% CI [−0.22, 0.80], p = 0.19) with age, −0.13 (95% CI [−0.65, 0.48], p = 0.69) with cognitive status (ACE-III), 0.57 (95% CI [0.00, 0.86], p = 0.05) with the FRS, and 0.19 (95% CI [−0.38, 0.72], p = 0.55) with the DAD. The lack of significant associations between these variables suggests that participant age, level of cognitive and functional impairment, did not strongly influence study compliance, although correlations should be interpreted with caution given the small sample size.
Feasibility: subjective participation experiences
Table 1 provides an overview of the descriptives for the study evaluation items. Results indicate that participants on average experienced low participation burden and high motivation, and ease of participating. Participants indicated that they had carefully responded to the questions and that they were satisfied with the training and support received from the research team. Participants rated three items more moderately (i.e., <4 or >2 for reverse-phrased items), suggesting a more neutral stance on enjoying tracking their thoughts, remembering to keep their phone with them, and completing the questions without self-reflection. However, these ratings still indicated a relatively positive experience. The item scores were corroborated by the open feedback provided by participants, where several participants expressed their appreciation for the opportunity to be involved in the study and to reflect on their daily thoughts and emotions, although one participant also commented that they found participation “quite boring”. Two participants provided feedback on methodological aspects (e.g., pointing out temporal ambiguities such as that ‘your future’ can refer to ‘your future tomorrow’ or ‘your future in years’ time’), underscoring their engagement with the research questions. The participant with the lowest compliance rate reported having difficulties hearing the notifications, suggesting that the research team may have missed an opportunity to assist with adjusting her phone settings.
Utility
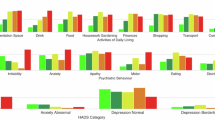
Table 2 provides an overview of the between-person and within-person variance and the ICC for each of the momentary and end-of-day items. The results suggest sufficient variability at the within-person level to support the utility of an intensive ESM design, with nine items even showing an ICC below 0.50, indicating greater within-person than between-person variability. The life satisfaction and meaning in life items measured on a daily level showed relatively higher ICC’s than momentary mood and ongoing thoughts, which is to be expected given the lower measurement frequency; however, these items still showed significant variability at a within-person level. Figure 1 provides a visual representation of the variability within and between participants per item.
Discussion
This study reports on the successful implementation of a high-intensity smartphone-based ESM approach in a targeted transdiagnostic sample of 12 participants with dementia. Through this detailed description of our methodology, we hope to provide a practical framework for future research using ESM in dementia populations. Key strategies include engaging a stakeholder panel or steering committee to co-design study materials and ensure feasibility, adopting a flexible and supportive approach tailored to participants’ specific needs, leveraging user-friendly technology, and closely monitoring progress throughout the study. Providing step-by-step instructions in accessible formats and offering ongoing assistance can also help participants feel supported and engaged. These practices underline the importance of balancing methodological rigor with adaptability and a focus on participant well-being while placing the firsthand experiences of people with dementia at the center of the inquiry. Informal carers also played a positive role in encouraging their spouses or parents, so their involvement can enhance participation and data quality. While support from a partner proved helpful for some participants, it was not essential, as several study members successfully completed the study independently.
Over half of the individuals approached for this study agreed to participate, which is higher than participation rates observed or estimated in the general population (5–30%; e.g., refs. 35,36) and in participants with mild cognitive impairment (36% and 14%)21,31. Zuidersma et al.21 suggested that the low participation rates in their study might have been influenced by participants being invited immediately after receiving a cognitive impairment diagnosis, a potentially suboptimal timing. A strength of our study was that participants already had an established relationship with the research clinic, with many having participated in prior studies. This may have enhanced their sense of engagement and agency, and their willingness to participate in research, thus mitigating against study dropout.
Participants also demonstrated a high compliance rate (80%), which is comparable but on the higher end of compliance rates observed in the average ESM study (78%)37,38 or in studies involving individuals with mild cognitive impairment (78%)30,31, acquired brain injuries (80% and 71%)13,14 and older adults in general (54–99%)15. This is notable given our study’s relatively short response window (20 min in total), which is more restrictive than similar research. We found no strong indication that the compliance rate was lower for older participants or participants with lower cognitive status. Overall, participants were able to complete the questionnaires swiftly, and they reported that the process was easy to do. On average, they also reported low participation burden, high motivation, and high carefulness in responding to the questions.
Our findings not only indicate that the ESM approach can be feasible and acceptable for dementia participants, but it also produces high-frequency data with sufficient within-person variability that can be effectively used for dynamic modeling, similar to for example, affect variabilities observed in other empirical studies39,40. Taken together, our findings highlight both the motivation and capabilities of people with dementia to engage with higher-intensity forms of real-time data collection, as well as the potential of such designs to generate meaningful insights. This study represents an important step in challenging possible misconceptions about the feasibility and value of involving people with dementia in this type of research.
Some limitations of this work should be considered and may guide future work. The most important limitation is the small, convenience-based sample, which limits the generalizability of the findings. Our participants represent a specific subgroup of people living with dementia—those who are younger, own and actively use a smartphone. Women were overrepresented in the sample, the age range was relatively narrow, and participants were largely in mild to moderate stages of dementia severity. However, as the population of people with dementia who use smartphones continues to grow, so does the potential of this approach for future research. Future studies are encouraged to consider adaptations that could enhance inclusivity for individuals who are older, have more advanced cognitive impairment, are less familiar with digital technology, or live in remote communities who may not be able to travel to participate in research41.
To improve accessibility of ESM for such populations, several adaptations could be explored. For participants who do not regularly use smartphones, researchers might provide simplified devices with intuitive user interfaces—such as basic tablets or smartwatches with large response buttons—paired with the necessary training and ongoing technical assistance. Previous ESM work with older populations, for instance, has highlighted the feasibility of using smartwatches with an integrated response system42. Interface design could also be tailored to individual sensory and cognitive needs by adjusting features like signal volume, vibration cues, and font sizes15. For participants with more advanced dementia, lower-tech alternatives—such as daily telephone check-ins or paper-based diaries—may provide rich information, even if they do not match the granularity of high-frequency ESM. A higher level of carer/informant involvement could also be considered, especially for participants facing more severe cognitive or motor challenges. Carers could be trained to prompt or assist with survey completion and to log contextual observations. Such protocols could allow for varying degrees of carer involvement depending on participant needs and designed to align with daily care routines. At the same time, preserving the validity of self-report data should remain a priority, so carer input should be minimally directive where feasible. In addition, future research could explore alternative data collection modalities to enhance accessibility. For instance, voice-interactive smart home devices could be adapted to deliver ESM prompts and record verbal responses, offering a type of automated digital interview. Depending on the research question, more passive data collection methods, such as the Electronically Activated Recorder (EAR)43 can also be explored. These methods show potential in capturing naturalistic insights, for example, into daily social behavior, by recording brief snippets of audio throughout the day. While such methods raise important ethical considerations, they have demonstrated predictive utility for psychological outcomes such as social connectedness and well-being in a US student sample44.
While our sample represents a specific subgroup of people with dementia, we did observe variability in participants’ cognitive and functional abilities, as reflected in their ACE-III, DAD, and FRS scores. Different patterns were evident depending on the specific diagnosis. For instance, participants with semantic dementia had lower ACE-III scores due to language difficulties, yet their functional abilities remained relatively intact. In contrast, participants with behavioral-variant frontotemporal dementia (bvFTD) had better cognitive function according to their ACE-III scores, but faced stronger challenges with behavioral changes and functional dependency, as reflected in their FRS scores. These differences highlight the importance of a flexible and individualized approach when assessing eligibility for ESM studies, not relying on single measures of cognitive status but taking into account each participant’s unique capabilities and challenges45. While the transdiagnostic nature of the sample was regarded as a positive aspect of the study by the SDN-LEEAP panel, future studies with larger samples would enable us to stratify our sample according to dementia subtype. Such studies could provide deeper insights into how ESM approaches should be tailored to different subtypes of dementia allowing for a more targeted understanding of the daily experiences of individuals within these populations.
To enable scaling ESM approaches to larger samples with dementia, several strategies could be considered. In addition to leveraging novel technologies for more automated data collection as described above, studies may increase efficiency by streamlining participant onboarding and support. For instance, collective onboarding sessions could be used to orient participants, supplemented by automated features such as reminders, progress tracking, and data management systems. Participant support could also be structured in a tiered format, beginning with access to comprehensive FAQs and troubleshooting guides for common issues, and offering more personalized, one-on-one support from the research team when needed.
In terms of study design, the current study employed a relatively high signaling intensity. However, the observed feasibility findings are specific to this design and may not generalize to even more intensive protocols, for example, with more items per interaction. Future research should explore the boundaries of different design choices within dementia populations. Additionally, while we emphasize the value of a flexible and pragmatic approach, we also acknowledge that certain methodological adjustments, such as slight modifications to the phrasing of validated items and truncated Likert scales, can have unintended effects46. The impact of such changes should be carefully considered and further investigated in future work. In this context, item quality assessment tools like the ESM-Q47 can serve as a valuable resource to guide the development and evaluation of items in future ESM studies within dementia populations.
In addition to refining methodological approaches, future efforts could explore how ESM might guide interventions and be integrated into clinical practice to enhance quality of life and care for people living with dementia. At a fundamental level, increasing opportunities for people with dementia to participate in ESM studies may be beneficial in itself. The process of self-monitoring can promote greater awareness of adaptive and less adaptive behaviors and contexts. Particularly when paired with personalized feedback on ESM trajectories, such approaches may help identify patterns in mood, well-being, or activity engagement, and factors that contribute to or detract from daily functioning8,31. These individualized insights may also serve as a valuable starting point in care conversations or provide complementary information in therapeutic settings. Beyond monitoring, ESM interfaces can be adapted to deliver interventions directly—for example, brief psychoeducation videos, guided relaxation or mindfulness exercises, or simple cognitive strategies—and may at the same time offer a platform for users to request support when needed48. Recent developments in ESM-based interventions, such as Just-In-Time Adaptive Interventions (JITAIs), further expand this potential. By combining real-time self-report data with, for example, contextual and sensor inputs, JITAIs can help identify moments when tailored support is most needed, enabling timely and responsive interventions that align with individual circumstances49.
As the landscape of dementia research evolves, methods like smartphone-based ESM present new opportunities to better understand the subjective experience of individuals living with dementia. The current study demonstrates the feasibility and appeal of this method for examining a neglected aspect of dementia, namely, their day-to-day psychological functioning and well-being. Future studies should examine different ESM designs and include larger and more diverse samples across different socioeconomic and cultural backgrounds, and spanning a broader range of dementia stages and subtypes. This will require substantial resources to ensure participants receive the support and guidance needed. However, our findings highlight the exciting potential of this approach for tracking fluctuating subjective experiences in dementia, underscoring its promise as a powerful tool to better understand the lived experiences of people with dementia and develop tailored interventions to support their wellbeing and improve dementia care.
Method
This study is a part of the Meaning in Mind Dementia (MinMIND) project, which focuses on how daily cognition and affect processes relate to meaning in life and well-being in dementia (https://osf.io/uh5dc/). As this article focuses on the methodological aspects of the study, we provide a comprehensive description of the methods and we summarize potential strategies and adaptations for conducting smartphone-based ESM studies in dementia populations in Table 3. All materials, including the recruitment flyer, eligibility questions, participant information sheet, informed consent form, measures, and other resources, are openly available on the OSF project page (https://osf.io/wg6kn/).
Stakeholder consultation
Prior to data collection, we consulted the Sydney Dementia Network Lived Experience Expert Advisory Panel (SDN-LEEAP). This panel comprises people with lived experience of dementia, as well as current and former carers, who regularly provide feedback and recommendations to inform dementia research priorities. The study was presented to 15 SDN-LEEAP members, inviting their input on the perceived acceptability and feasibility of the approach and any suggestions for improvement. The panel had two weeks to read through the study materials, following which the first author gave a presentation to the panel describing the rationale, objectives, and methodology of the ESM protocol. All LEEAP panel members responded very positively to the overall study aims, endorsing the value of a smartphone-based ESM approach as a way of collecting real-life data, and commenting on the need for this type of approach to ensure meaningful participation of people with dementia. Several recommendations were proposed by the panel, all of which were integrated into the study design. These included: (i) using Likert-scale buttons instead of sliders, (ii) incorporating a training video on how to install and use m-Path in addition to written instructions, (iii) extending data collection from seven to ten days to capture greater variability in experiences, and (iv) recruiting a broad, transdiagnostic sample to promote inclusivity.
Participant recruitment
Adults with dementia were recruited from the FRONTIER research clinic at the Brain and Mind Centre at the University of Sydney, Australia between March 2023 and November 2024. Participants attend FRONTIER for diagnosis and follow-up and provide informed consent which includes their permission to be approached for new studies and to use their pseudonymized clinical data for future research. Exclusion criteria for this study included severe hearing, vision, or speech impairments, or other major neurological or psychological disorders (e.g., severe brain injury, schizophrenia, bipolar disorder, substance abuse), and inability to independently use their smartphone. Inclusion criteria were: a dementia diagnosis according to current international consensus criteria50,51,52 following multidisciplinary consensus between FRONTIER team members (senior neurologist, clinical neuropsychologist, occupational therapist) based on medical history, comprehensive clinical assessment, cognitive assessments, and structural neuroimaging where available, age 50 or older, living at home, owning and using a smartphone in daily life, having recently (i.e., within the last half year) visited the FRONTIER clinic with full diagnostic information available, and proficiency in English. The availability of recent clinical and diagnostic data enabled fully remote recruitment and participation (via email and video calls), reducing participant burden by removing the need for additional clinic visits. Participants were further required to be physically, psychologically, and cognitively able to participate in the study. This was assessed through a flexible individualized approach, recognizing that single test scores are not always representative of a person’s real-world ability to participate in research. First, potential participants were identified based on indicators of sufficiently preserved functional abilities, including cognitive test scores and evaluations of instrumental activities of daily living (e.g., ACE-III, DAD, FRS; see Measures). This initial screening was supplemented by consultation with research assistants or team members who had interacted with the individuals during their most recent clinic visit and could provide additional insights into their likely ability to engage in the study.
Potential participants and/or their family carers (depending on the preferred contact listed in their file) were initially contacted via email with study information and a flyer. Recipients were invited to reply if interested in learning more about the study. If no response was received, a follow-up email or phone call was made during which participants could indicate if they were interested in learning more about the study. For those who expressed interest, a separate phone or video call was arranged to provide detailed information about the study and to further assess eligibility through a screening conversation focused on the study’s practical requirements. This included questions on smartphone use and proficiency, as well as participants’ waking hours and daily schedules, to tailor the signaling schedule. Calls were conducted with participants alone or with a significant other or care partner (e.g., spouse, adult child), depending on the cognitive capacity, preferences, and needs of the individual.
After the call, participants received detailed written information about the study, an informed consent sheet summarizing key points, and a link to an online consent form on the secure REDCap environment. Participants were encouraged to review these materials at their own pace and were reminded they could contact the research team with any remaining questions before completing the consent form. Once the completed form was received, participants were emailed instructions on how to download and register on m-Path, the app used for ESM data collection34. These instructions were provided in both written form and as a video tutorial, carefully demonstrating each step (e.g., how to download the app, register for the study, enter their participant ID, grant the necessary permissions). The research team remained available to assist with any issues during this registration process.
After participants successfully registered on m-Path, a video call was scheduled for a trial run of the data collection. During this session, participants received a test notification and practiced responding to a trial survey with guidance from the researcher. It was also verified whether their sound settings were appropriate (to signal a momentary notification). Once participants were comfortable using the app and understood the process, a start date for data collection was set.
Data collection procedure
On the first day, participants received a single auditory notification with a baseline questionnaire assessing their general experience of meaning in life, depressive symptoms, and life satisfaction (see Measures for details). A reminder notification was sent two hours later, and participants had the entire day to complete this initial questionnaire. The following day, the 10-day ESM data collection began. Participants received seven notifications daily at semi-random intervals within 90-minute blocks, with a minimum 15-minute gap between consecutive notifications. Each notification included a brief reminder: “You are participating in a study run by the FRONTIER clinic about daily experiences of people with dementia. Please answer the following questions.” Participants were prompted to answer the same set of questions about their momentary thoughts and feelings, with item order randomized within multi-item scales (see Measures). The first question was open-ended, prompting participants to share their ongoing thoughts via voice recording. The voice recording feature enabled participants to respond extemporaneously, without being constrained by typing proficiency or speed. All the other questions were Likert-type items. Figure 2 shows screenshots with example items in the m-Path app. If participants did not respond within five minutes, they received a reminder notification, which expired after an additional 15 min. At a fixed time each evening, tailored to the schedule of each participant, they received an eighth notification with a short end-of-day questionnaire assessing their daily meaning in life and life satisfaction. A reminder was sent if participants did not respond within 30 min, and they had the entire evening to complete it. After this 10-day period, participants received a final notification with an end-point questionnaire with the same items of the baseline questionnaire in addition to a study participation evaluation. Again, a reminder was sent after two hours, and participants had the entire day to complete this final questionnaire. The data collected were complemented by background demographic and clinical information drawn from participants’ most recent clinic visit (see Measures).
Follow-up
After two to four days of data collection, a follow-up videocall was scheduled by a researcher to discuss participants’ experiences. The researcher inquired about any perceived burden or distress and encouraged participants to share questions or concerns. Adjustments were made as needed based on their feedback. For example, the first participant suggested that some of the Likert-scale items would be more intuitive if they repeated the specific content from the item (e.g., “very happy” instead of “very”). This change was implemented for her and all subsequent participants. Three participants needed additional time to familiarize themselves with the data collection process, and they reported feeling not satisfied with their response rate in the initial days. To address this, we extended the data collection period by one or two days in consultation with the participants. In certain cases, personalized adaptations were required. For example, one participant struggled to remember to keep her phone nearby. At her partner’s suggestion, notifications were synchronized with his phone, allowing him to remind her to respond. This measure significantly improved her compliance without creating undue burden for her partner, according to his report. Another participant, who was working part-time, was unable to respond to notifications during work. Therefore, the signaling schedule during four working days was modified to reduce the number of notifications sent during her working hours.
Ethical considerations
Given the novelty of applying an ESM approach in a dementia population, we gave particular attention to ethical considerations in this study. As mentioned above, the study design and ESM procedures were developed in consultation with the SDN-LEEAP panel to ensure they reflected the experiences of the target population and were feasible and inclusive. The input from the panel also proved invaluable in addressing queries from the two ethics committees that evaluated the project. Consequently, the research was approved by the Human Research Ethics Committee of the University of Sydney (2022/882) and the Social and Societal Ethics Committee of KU Leuven (G-2022-4720-R3).
During recruitment, we ensured that participants received comprehensive yet accessible information about all aspects of the study. The information was presented in clear, straightforward language tailored to their abilities and delivered in a stepwise manner to allow participants sufficient time to review at their own pace. Participants were encouraged to ask questions at any stage, and efforts were made to foster engagement and demonstrate respect for their role in the research.
For informed consent, we adopted a process consent approach53, which involves regularly checking and reaffirming participants’ ongoing consent throughout the study and closely monitoring for any signs of distress or concerns. At the end of each day, after completing the end-of-day questionnaire, participants were reminded of the voluntary nature of their participation and were provided with the researcher team’s contact details: “Thank you for completing today’s questionnaires. Remember that your participation in this study is completely voluntary. If you experience any difficulties, have questions or concerns, or wish to stop your participation, you can contact the research team at any time.” None of the participants revoked their participation during the study.
Measures
Figure 3 gives an overview of the measures and number of items collected at different phases of the data collection procedure. The measures used are described in brief below, but more detailed information can be found in the Supplementary Materials on OSF (https://osf.io/wg6kn/).
The baseline questionnaire included questionnaires on meaning in life, life satisfaction, and depressive symptoms. Meaning in life and its three subdimensions (coherence, purpose, significance) were measured with the Three Dimensional Meaning in Life Scale (3DM)54 on a 5-point Likert-type scale ranging from 1 (not at all true) to 5 (very true). Minor adaptations were made to item wordings without changing the meaning to increase comprehensibility for the dementia sample (e.g., “Every day I experience the sense that life is worth living” changed to “Every day I feel that life is worth living”). Reliability as indicated by McDonald’s ω was 0.93 for the total scale, .87 for coherence, 0.96 for purpose, and .75 for significance. Life satisfaction was measured with the 5-item Satisfaction With Life Scale (SWLS)55, rated on a 5-point Likert scale from 1 (strongly disagree) to 5 (strongly agree). McDonald’s ω in the current sample was 0.98. Depressive symptoms were measured with the 10-item short form of the Center for Epidemiologic Studies Depression scale (CES-D)56,57, with a 4-point Likert scale ranging from 0 (rarely or none of the time) to 3 (most or almost all the time). McDonald’s ω in the current sample was 0.90.
The end-point questionnaire included the same questionnaires as the baseline questionnaire in addition to 18 items assessing participants’ experiences about being in the study, selected and adapted from ref. 58 (see Results section Table 1 for the full item list). Participants used a 5-point Likert scale to report their participation burden (e.g., “It was tiring to take part in this study.”), ease of use (e.g., “The app was easy to use.”), enjoyment and motivation (e.g., “I stayed motivated to respond to the beeps during the study.”), their carefulness in responding (e.g., “I paid a lot of attention to what the questions were asking.”), and satisfaction with the training and support received (e.g., “I felt supported by the researchers during the study.”). As the different themes do not represent validated subscales, no scale scores were calculated. Presenting the data from individual items also allows for more granular insights into specific aspects of the experience. In addition to the questionnaire, participants were invited to leave any remaining open-ended comments or feedback. McDonald’s ω was .95 for the total 3DM scale, 0.89 for coherence, 0.94 for purpose, 0.79 for significance, 0.94 for the SWLS, and 0.96 for CES-D.
The momentary ESM questionnaire included items on ongoing thought and affect. Regarding ongoing thought, participants first responded to one open-ended question: “Just before you opened this application, what were you thinking about? Please tell us in a couple of sentences using the record button below. Tap the record button and your voice will be recorded as you describe your thoughts.” Next, they responded to six follow-up statements regarding the thoughts they just described (e.g., “My thoughts were about events from my past”, “My thoughts were about myself”; see Results section Table 2 for the full item list) using a Likert-scale from 1 (not at all) to 5 (completely). These items were selected and adapted from previous studies using Multi-Dimensional Experience Sampling59,60. Momentary affect was measured with 6 items (e.g., “1. How happy do you feel at the moment?”, “How anxious do you feel at the moment?”; see Results section Table 2 for the full item list) selected to cover the four quadrants of the affective circumplex model, which includes the two dimensions of valence (positive vs. negative) and arousal (activated vs. deactivated)61,62,63. The items were rated on a 5-point Likert scale from 1 (not at all) to 5 (very).
The end-of-day questionnaire included three items. A single item (“How satisfied did you feel with your life today?”) rated on a 5-point Likert scale from 1 (very dissatisfied) to 5 (very satisfied) was used to assess daily life satisfaction64. Two items (“How meaningful did you feel your life was today?” and “How much purpose did you feel in your life today?”) rated on a 5-point Likert Scale were used to measure daily meaning63,65.
Background clinical information was extracted from participants’ files, including demographic information (age, sex, education), most recent diagnostic information, overall cognitive functioning as measured with the Addenbrooke’s Cognitive Examination - III (ACE-III)66, functional abilities as measured with the Disability Assessment for Dementia Scale (DAD)67, and behavioral changes and functional dependence as measured with the Frontotemporal Dementia Rating Scale (FRS)68. Scores on the ACE-III and DAD range from 0 to 100, and scores on the FRS range from −6.66 to 5.39 (Rasch score), with lower scores reflecting greater impairment.
Data analysis
Data were analyzed using IBM SPSS Statistics 28 and R69. First, descriptive analyses were performed to characterize the sample in terms of demographics and cognitive performance. Second, feasibility was assessed by calculating the participation rate (i.e., the proportion of contacted individuals who agreed to participate), drop-out rate, compliance, and completion times. For participants with an extended ESM data collection (see section “Follow-up”) to 11 (n = 2) or 12 days (n = 1), data for the entire data collection period was used. In addition, two-tailed Pearson correlations were explored between compliance and both age and the clinical variables (ACE-III, DAD, FRS), and descriptive statistics were calculated for the study participation evaluation items. Third, utility was assessed by calculating the between-person and within-person variability and the intraclass correlation coefficient (ICC) for the momentary and daily measures. These values were computed using unconditional multilevel models for each item with the lme4 package70, with participant ID as the grouping variable. The ICC represents the proportion of between-person variance relative to the total variance (the sum of between-person and within-person variance). A very high ICC (e.g., >0.90) indicates that individuals differ from each other on a given variable but show little variation within themselves over time, indicating that frequent repeated measurements are unnecessary71. Therefore, sufficient within-person variability and a moderately-sized ICC are essential to justify the use of a high-frequency longitudinal ESM design.
Data availability
The data that support the findings of this study are not openly available due to the restricting conditions in our ethics approval. The data can be requested by contacting the corresponding author, and access will be granted after obtaining the necessary approval and data sharing agreements in accordance with ethical procedures governing the reuse of sensitive data. The R code for this study is available on the Open Science Framework and can be accessed via https://osf.io/wg6kn/. Analytic details not included in the R code can be requested by contacting the corresponding author.
References
Myin-Germeys, I. & Kuppens, P. Experience sampling methods, an introduction. In The open handbook of experience sampling methodology: A step-by-step guide to designing, conducting, and analyzing ESM studies (eds Myin-Germeys I. & Kuppens P.) 7–19 (Center for Research on Experience Sampling and Ambulatory Methods Leuven, 2022).
Shiffman, S., Stone, A. A. & Hufford, M. R. Ecological momentary assessment. Annu. Rev. Clin. Psychol. 4, 1–32 (2008).
Myin‐Germeys, I. et al. Experience sampling methodology in mental health research: new insights and technical developments. World Psychiatry 17, 123–132 (2018).
Verhagen, S. J., Hasmi, L., Drukker, M., van Os, J. & Delespaul, P. A. Use of the experience sampling method in the context of clinical trials. BMJ Ment. Health 19, 86–89 (2016).
Scollon, C. N., Kim-Prieto, C. & Diener, E. Experience sampling: promises and pitfalls, strengths and weaknesses. J. Happiness Stud. 4, 5–34 (2003).
Csikszentmihalyi, M. & Larson, R. Validity and reliability of the experience-sampling method. J. Nerv. Ment. Dis. 175, 526–536 (1987).
Wichers, M. et al. Momentary assessment technology as a tool to help patients with depression help themselves. Acta Psychiatr. Scand. 124, 262–272 (2011).
Van Knippenberg, R., De Vugt, M., Ponds, R., Myin-Germeys, I. & Verhey, F. An experience sampling method intervention for dementia caregivers: results of a randomized controlled trial. Am. J. Geriatr. Psychiatry 26, 1231–1243 (2018).
Mölsä, M. E., Lax, M., Korhonen, J., Gumpel, T. P. & Söderberg, P. The experience sampling method in monitoring social interactions among children and adolescents in school: a systematic literature review. Front. Psychol. 13, 844698 (2022).
Vilaysack, B., Cordier, R., Doma, K. & Chen, Y. W. Capturing everyday experiences of typically developing children aged five to seven years: a feasibility study of experience sampling methodology. Aust. Occup. Ther. J. 63, 424–433 (2016).
Chen, Y.-W., Cordier, R. & Brown, N. A preliminary study on the reliability and validity of using experience sampling method in children with autism spectrum disorders. Dev. Neurorehabil. 18, 383–389 (2015).
Myin-Germeys, I. et al. Experience sampling research in psychopathology: opening the black box of daily life. Psychol. Med. 39, 1533–1547 (2009).
Lenaert, B. et al. Exploring the feasibility and usability of the experience sampling method to examine the daily lives of patients with acquired brain injury. Neuropsychol. Rehabil. 29, 754–766 (2019).
Johnson, E. et al. Feasibility and validity of computerized ambulatory monitoring in stroke patients. Neurology 73, 1579–1583 (2009).
Vanhollebeke, J., Appel, J. E., Dezutter, J. & Dewitte, L. Use of the time-based experience sampling methods in older adults: a systematic review of studies between 2007 and 2022 and recommendations for future research Eur. J. Psychol. Assess. 40, 481–497 (2024).
Cabrita, M., Lousberg, R., Tabak, M., Hermens, H. J. & Vollenbroek-Hutten, M. M. An exploratory study on the impact of daily activities on the pleasure and physical activity of older adults. Eur. Rev. Aging Phys. Act. 14, 1–11 (2017).
Allard, M. et al. Mobile technologies in the early detection of cognitive decline. PLoS One 9, e112197 (2014).
Kim, H. et al. Depression prediction by using ecological momentary assessment, actiwatch data, and machine learning: observational study on older adults living alone. JMIR mHealth uHealth 7, e14149 (2019).
Rullier, L. et al. Daily life functioning of community‐dwelling elderly couples: an investigation of the feasibility and validity of Ecological Momentary Assessment. Int. J. Methods Psychiatr. Res. 23, 208–216 (2014).
Miklitz, C., Fliessbach, K. & McCormick, C. Happiness, positive emotions, and subjective well-being in dementia. Front. Neurol. 15, 1422354 (2024).
Zuidersma, M., Müller, F., Snippe, E., Zuidema, S. U. & Oude Voshaar, R. C. Feasibility, usability and clinical value of intensive longitudinal diary assessments in older persons with cognitive impairment and depressive symptoms. Aging Ment. Health 27, 1466–1475 (2023).
Wijbenga, R. A. et al. Individual differences in the temporal relationship between sleep and agitation: a single-subject study in nursing home residents with dementia experiencing sleep disturbance and agitation. Aging Ment. Health 26, 1669–1677 (2022).
Beerens, H. C. et al. The association between aspects of daily life and quality of life of people with dementia living in long-term care facilities: a momentary assessment study. Int. Psychogeriatr. 28, 1323–1331 (2016).
Niculescu, I. et al. Ecological momentary assessment of depression in people with advanced dementia: Longitudinal pilot study. JMIR Aging 4, e29021 (2021).
Ramsey, A. T., Wetherell, J. L., Depp, C., Dixon, D. & Lenze, E. Feasibility and acceptability of smartphone assessment in older adults with cognitive and emotional difficulties. J. Technol. Hum. Serv. 34, 209–223 (2016).
Benge, J. F. et al. The smartphone in the memory clinic: a study of patient and care partner’s utilisation habits. Neuropsychol. Rehabil. 30, 101–115 (2018).
Joddrell, P. & Astell, A. J. Studies involving people with dementia and touchscreen technology: a literature review. JMIR Rehabil. Assistive Technol. 3, e5788 (2016).
Wilson, S. A., Byrne, P., Rodgers, S. E. & Maden, M. A Systematic review of smartphone and tablet use by older adults with and without cognitive impairment. Innov. Aging 6, igac002 (2022).
Orrell, M. et al. Improving the lives of people with dementia through technology: Interdisciplinary network for dementia utilising current technology. (Routledge London, 2022).
Zhaoyang, R., Sliwinski, M. J., Martire, L. M., Katz, M. J. & Scott, S. B. Features of daily social interactions that discriminate between older adults with and without mild cognitive impairment. J. Gerontol., Ser. B Psychol. Sci. Soc. Sci. 79, gbab019 (2024).
Bartels, S. L., van Knippenberg, R. J., Malinowsky, C., Verhey, F. R. & de Vugt, M. E. Smartphone-based experience sampling in people with mild cognitive impairment: feasibility and usability study. JMIR aging 3, e19852 (2020).
Nicosia, J. et al. Unsupervised high-frequency smartphone-based cognitive assessments are reliable, valid, and feasible in older adults at risk for Alzheimer’s disease. J. Int. Neuropsychol. Soc. 29, 459–471 (2023).
Staffaroni, A. M., Tsoy, E., Taylor, J., Boxer, A. L. & Possin, K. L. Digital cognitive assessments for dementia: digital assessments may enhance the efficiency of evaluations in neurology and other clinics. Pract. Neurol. 2020, 24 (2020).
Mestdagh, M. et al. m-Path: an easy-to-use and highly tailorable platform for ecological momentary assessment and intervention in behavioral research and clinical practice. Front. Digit. health 5, 1182175 (2023).
Maes, I. H. et al. Measuring health-related quality of life by experiences: the experience sampling method. Value Health 18, 44–51 (2015).
Stone, A. A. et al. Shedding light on participant selection bias in Ecological Momentary Assessment (EMA) studies: findings from an internet panel study. PLoS One 18, e0282591 (2023).
Vachon, H., Viechtbauer, W., Rintala, A. & Myin-Germeys, I. Compliance and retention with the experience sampling method over the continuum of severe mental disorders: meta-analysis and recommendations. J. Med. Internet Res. 21, e14475 (2019).
Rintala, A., Wampers, M., Myin-Germeys, I. & Viechtbauer, W. Response compliance and predictors thereof in studies using the experience sampling method. Psychol. Assess. 31, 226 (2019).
Cloos, L., Ceulemans, E. & Kuppens, P. Development, validation, and comparison of self-report measures for positive and negative affect in intensive longitudinal research. Psychol. Assess. 35, 189 (2023).
Podsakoff, N. P., Spoelma, T. M., Chawla, N. & Gabriel, A. S. What predicts within-person variance in applied psychology constructs? An empirical examination. J. Appl. Psychol. 104, 727 (2019).
Ahmed, R. M., Piguet, O., Mummery, C., Naismith, S. & Irish, M. The Holy Grail: Highlighting the need for equitable access to dementia treatments and clinical trials. Lancet Reg. Heal. West. Pac. Reg. 55, 101492 (2025).
Rouzaud Laborde, C. et al. Satisfaction, usability, and compliance with the use of smartwatches for ecological momentary assessment of knee osteoarthritis symptoms in older adults: usability study. JMIR aging 4, e24553 (2021).
Mehl, M. R. The electronically activated recorder (EAR) a method for the naturalistic observation of daily social behavior. Curr. Dir. Psychol. Sci. 26, 184–190 (2017).
Sun, J., Harris, K. & Vazire, S. Is well-being associated with the quantity and quality of social interactions? J. Personal. Soc. Psychol. 119, 1478 (2020).
Strikwerda-Brown, C., Grilli, M. D., Andrews-Hanna, J. R. & Irish, M. All is not lost”—Rethinking the nature of memory and the self in dementia. Ageing Res. Rev. 54, 100932 (2019).
Stewart, A. L., Thrasher, A. D., Goldberg, J. & Shea, J. A. A framework for understanding modifications to measures for diverse populations. J. Aging Health 24, 992–1017 (2012).
Eisele, G. et al. ESM-Q: a consensus-based quality assessment tool for experience sampling method items. Behav. Res. Methods 57, 1–20 (2025).
Balaskas, A., Schueller, S. M., Cox, A. L. & Doherty, G. Ecological momentary interventions for mental health: a scoping review. PLoS One 16, e0248152 (2021).
Nahum-Shani, I. et al. Just-in-time adaptive interventions (JITAIs) in mobile health: key components and design principles for ongoing health behavior support. Ann. Behav. Med. 52, 446–462 (2018).
Rascovsky, K. et al. Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. Brain 134, 2456–2477 (2011).
McKhann, G. M. et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer’s. Dement. 7, 263–269 (2011).
Gorno-Tempini, M. L. et al. Classification of primary progressive aphasia and its variants. Neurology 76, 1006–1014 (2011).
Dewing, J. Participatory research: a method for process consent with persons who have dementia. Dementia 6, 11–25 (2007).
Martela, F. & Steger, M. F. The role of significance relative to the other dimensions of meaning in life–an examination utilizing the three dimensional meaning in life scale (3DM). J. Posit. Psychol. 18, 606–626 (2023).
Diener, E., Emmons, R. A., Larsen, R. J. & Griffin, S. The satisfaction with life scale. J. Pers. Assess. 49, 71–75 (1985).
Radloff, L. S. The CES-D scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1, 385–401 (1977).
Andresen, E. M., Malmgren, J. A., Carter, W. B. & Patrick, D. L. Screening for depression in well older adults: evaluation of a short form of the CES-D. Am. J. Prev. Med. 10, 77–84 (1994).
Eisele, G. et al. The effects of sampling frequency and questionnaire length on perceived burden, compliance, and careless responding in experience sampling data in a student population. Assessment 29, 136–151 (2022).
Smallwood, J. et al. Representing representation: Integration between the temporal lobe and the posterior cingulate influences the content and form of spontaneous thought. PLoS One 11, e0152272 (2016).
Turnbull, A. et al. Age-related changes in ongoing thought relate to external context and individual cognition. Conscious. Cogn. 96, 103226 (2021).
Russell, J. A. A circumplex model of affect. J. Personal. Soc. Psychol. 39, 1161 (1980).
Dejonckheere, E. et al. The bipolarity of affect and depressive symptoms. J. Personal. Soc. Psychol. 114, 323 (2018).
Newman, D. B., Nezlek, J. B. & Thrash, T. M. The dynamics of searching for meaning and presence of meaning in daily life. J. Pers. 86, 368–379 (2018).
Newman, D. B., Schwarz, N. & Stone, A. A. Global reports of well-being overestimate aggregated daily states of well-being. J. Positive Psychol. 16, 407–416 (2020).
Kashdan, T. & Steger, M. Curiosity and pathways to well-being and meaning in life: traits, states, and everyday behaviors. Motiv. Emot. 31, 159–173 (2007).
Hsieh, S., Schubert, S., Hoon, C., Mioshi, E. & Hodges, J. R. Validation of the Addenbrooke’s cognitive examination III in frontotemporal dementia and Alzheimer’s disease. Dement. Geriatr. Cogn. Disord. 36, 242–250 (2013).
Gélinas, I., Gauthier, L., McIntyre, M. & Gauthier, S. Development of a functional measure for persons with Alzheimer’s disease: the disability assessment for dementia. Am. J. Occup. Ther. 53, 471–481 (1999).
Mioshi, E., Hsieh, S., Savage, S., Hornberger, M. & Hodges, J. R. Clinical staging and disease progression in frontotemporal dementia. Neurology 74, 1591–1597 (2010).
R Core Team. (R Foundation for Statistical Computing, 2022).
Bates, D., Mächler, M., Bolker, B. & Walker, S. Fitting linear mixed-effects models using lme4. J. Stat. Softw. 67, 1–48 (2015).
Kuppens, P. & Myin-Germeys, I. Research questions that can be answered with ESM research. In The open handbook of experience sampling methodology: A step-by-step guide to designing, conducting, and analyzing ESM studies (eds Myin-Germeys I. & Kuppens P.) 21–31 (Center for Research on Experience Sampling and Ambulatory Methods Leuven, 2022).
Acknowledgements
This work was supported by the Research Foundation Flanders (FWO) [12A7322N to LD]. MI is supported by an Investigator Grant from the National Health and Medical Research Council of Australian (GNT2025228) and a Medical Research Future Fund grant from the Department of Health and Aged Care (MRF2024329).
Author information
Authors and Affiliations
Contributions
L.D., E.D., J.D., M.V., and M.I. designed the study. L.D. collected the questionnaire and ESM data. R.M.A. collected clinical data and characterized the sample. L.D. analyzed the data, E.D. assisted with the data analyses. L.D. wrote the manuscript; E.D., J.D., M.V., and M.I. provided critical feedback on the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
E.D. is co-founder and shareholder of m-Path Software, the commercial experience sampling platform that was used in this study. E.D. declares no non-financial competing interests. All other authors declare no financial or non-financial competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dewitte, L., Dejonckheere, E., Dezutter, J. et al. Experience sampling in dementia: feasibility, utility and methodological insights from a high-intensity smartphone-based study. npj Dement. 1, 21 (2025). https://doi.org/10.1038/s44400-025-00023-1
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s44400-025-00023-1