Abstract
Study design:
Retrospective cohort study.
Objectives:
Our study aimed to describe the outcome of bloodstream infection (BSI) in spinal cord injury (SCI) patients and their associated risk factors for severity and mortality.
Setting:
A French University Hospital.
Methods:
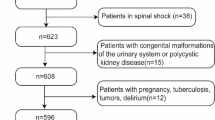
We conducted a retrospective cohort study of all BSIs occurring in hospitalized SCI patients. We analyzed their outcome and risk factors especially the impact of multidrug-resistant organisms (MDROs).
Results:
Overall, 318 BSIs occurring among 256 patients were included in the analysis. Mean age was 50.8 years and gender ratio (M/F) was 2.70, with a mean injury duration of 11.6 years.
Severity and 30-day mortality of BSI episodes were, respectively, 43.4% and 7.9%. BSI severity was significantly more frequent when caused by respiratory tract infections (RTIs) (odds ratio (OR)=1.38; 95% confidence interval (CI): 1.13–1.44) and significantly lower when caused by urinary tract infections (UTIs) (OR=0.47; 95% CI: 0.28–0.76). BSI mortality was significantly higher when caused by RTIs (OR=3.08; 95% CI: 1.05–8.99), catheter-related bloodstream infections (OR=3.54; 95% CI: 1.36–9.18) or Pseudomonas aeruginosa infections (OR=3.79; 95% CI: 1.14–12.55).
MDROs were responsible for 41.2% of all BSI. They have no impact on severity and mortality, whichever be the primary site of infection.
In multivariate analysis, mortality was higher when BSI episodes were due to RTIs (OR=3.26; 95% CI: 1.29–8.22) and Pseudomonas aeruginosa infections (OR=3.53; 95% CI: 1.06–11.70), or when associated with immunosuppressive therapy (OR=2.57; 95% CI: 1.14–5.78) or initial severity signs (OR=1.68; 95% CI: 1.01–2.81).
Conclusion:
BSI occurring in SCI population were often severe but mortality remained low. MDROs were frequent but not associated with severity or mortality of BSI episodes. Risk factors associated with mortality were initial severe presentation, RTI, immunosuppressive therapy and BSI due to Pseudomonas aeruginosa.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
National Spinal Cord Injury Statistical Center Spinal Cord Injury Facts and Figures at a Glance. National Institute of Disability Rehabilitation Research: Washington, DC, USA,. 2015. Available at: https://www.nscisc.uab.edu/Public/Facts2015.pdf (last accessed 20 September 2016).
Lalwani S, Punia P, Mathur P, Trikha V, Satyarthee G, Misra MC . Hospital acquired infections: preventable cause of mortality in spinal cord injury patients. J Lab Physicians 2014; 6: 36–39.
Wall BM, Mangold T, Huch KM, Corbett C, Cooke CR . Bacteremia in the chronic spinal cord injury population: risk factors for mortality. J Spinal Cord Med 2003; 26: 248–253.
Darouiche RO . In: Lin VW, Cardenas DD, Cutter NC, Frost FS, Hammond MC, Lindblom LB et al (eds). Spinal Cord Medicine: Principles and Practice. Demos Medical Publishing LLC: New York, NY, USA. 2003, pp 201.
Evans CT, LaVela SL, Weaver FM, Priebe M, Sandford P, Niemiec P et al. Epidemiology of hospital-acquired infections in veterans with spinal cord injury and disorder. Infect Control Hosp Epidemiol 2008; 29: 234–242.
DeVivo MJ, Stover S . In: Stover SL, DeLisa JA, Whiteneck GG (eds). Spinal Cord Injury: Clinical Outcomes from the Model Systems. Aspen Publications: Gaithersburg, MD, USA. 1995, pp 289–313.
DeVivo MJ, Krause JS, Lammertse DP . Recent trends in mortality and causes of death among persons with spinal cord injury. Arch Phys Med Rehabil 1999; 80: 1411–1419.
Evans CT, Hershow RC, Chin A, Foulis PR, Burns SP, Weaver FM . Bloodstream infections and setting of onset in persons with spinal cord injury and disorder. Spinal Cord 2009; 47: 610–615.
Dinh A, Saliba M, Saadeh D, Bouchand F, Descatha A, Roux AL et al. Blood stream infections due to multidrug-resistant organisms among spinal cord-injured patients, epidemiology over 16 years and associated risks: a comparative study. Spinal Cord 2016; 54: 720–725.
NCCLS.Performance standards for Antimicrobial Susceptibility Testing, 25th Informational Supplement, NCCLS, Wayne, PA, USA, Approved standard M100-S25, 2015. http://shop.clsi.org/site/Sample_pdf/M100S25_sample.pdf?bcsi_scan_628cd39dca2568d2=8kbY8qJQWooHYUPyF0AuEjSjOCsdAAAAU/6Kwg==&bcsi_scan_filename=M100S25_sample.pdf. Accessed on 25 November 2016.
Tenover FC, Raney PM, Williams PP, Rasheed JK, Biddle JW, Oliver A et al. Evaluation of the NCCLS extended-spectrum β-lactamase confirmation methods for Escherichia coli with isolates collected during Project ICARE. J Clin Microbiol 2003; 41: 3142–3146.
Lillie PJ, Allen J, Hall C, Walsh C, Adams K, Thaker H et al. Long-term mortality following bloodstream infection. Clin Microbiol Infect 2013; 19: 955–960.
Laupland KB, Gregson DB, Zygun DA, Doig CJ, Mortis G, Church DL . Severe bloodstream infections: a population-based assessment. Crit Care Med 2004; 32: 992–997.
Wenzel RP, Edmond MB . The impact of hospital-acquired bloodstream infections. Emerg Infect Dis 2001; 7: 174–177.
Waites KB, Canupp KC, Chen Y, DeVivo MJ, Moser SA . Bacteremia after spinal cord injury in initial versus subsequent hospitalizations. J Spinal Cord Med 2001; 24: 96–100.
Bhatt K, Cid E, Maiman D . Bacteremia in the spinal cord injury population. J Am Paraplegia Soc 1987; 10: 11–14.
Montgomerie JZ, Chan E, Gilmore DS, Canawati HN, Sapico FL . Low mortality among patients with spinal cord injury and bacteremia. Rev Infect Dis 1991; 13: 867–871.
Weinstein MP, Murphy JR, Reller LB, Lichtenstein KA . The clinical significance of positive blood cultures: a comprehensive analysis of 500 episodes of bacteremia and fungemia in adults. Clinical observations, with special reference to factors influencing prognosis. Rev Infect Dis 1983; 5: 54–70.
DeVivo MJ, Black KJ, Stover SL . Causes of death during the first 12 years after spinal cord injury. Arch Phys Med Rehabil 1993; 74: 248–254.
Micek ST, Lloyd AE, Ritchie DJ, Reichley RM, Fraser VJ, Kollef MH . Pseudomonas aeruginosa bloodstream infection: importance of appropriate initial antimicrobial treatment. Antimicrob Agents Chemother 2005; 49: 1306–1311.
Traugott KA, Echevarria K, Maxwell P, Green K, Lewis JS . Monotherapy or combination therapy? The Pseudomonas aeruginosa conundrum. Pharmacotherapy 2011; 31: 598–608.
Lim CJ, Cheng AC, Kennon J, Spelman D, Hale D, Melican G et al. Prevalence of multidrug-resistant organisms and risk factors for carriage in long-term care facilities: a nested case–control study. J Antimicrob Chemother 2014; 69: 1972–1980.
Kang CI, Kim SH, Park WB, Lee KD, Kim HB, Oh MD et al. Bloodstream infections caused by Enterobacter species: predictors of 30-day mortality rate and impact of broad-spectrum cephalosporin resistance on outcome. Clin Infect Dis 2004; 39: 812–818.
Deal EN, Micek ST, Ritchie DJ, Reichley RM, Dunne WM, Kollef MH . Predictors of in-hospital mortality for bloodstream infections caused by Enterobacter species or Citrobacter freundii. Pharmacotherapy 2007; 27: 191–199.
Chang EP, Chiang DH, Lin ML, Chen TL, Wang FD, Liu CY . Clinical characteristics and predictors of mortality in patients with Enterobacter aerogenes bacteremia. J Microbiol Immunol Infect 2009; 42: 329–335.
Kim BN, Woo JH, Ryu J, Kim YS . Resistance to extended-spectrum cephalosporins and mortality in patients with Citrobacter freundii bacteremia. Infection 2003; 31: 202–207.
Kollef MH, Sherman G, Ward S, Fraser VJ . Inadequate antimicrobial treatment of infections: a risk factor for hospital mortality among critically ill patients. Chest 1999; 115: 462–474.
Montgomerie JZ . Infections in patients with spinal cord injuries. Clin Infect Dis 1997; 25: 1282–1285.
Obritsch MD, Fish DN, MacLaren R, Jung R . Nosocomial infections due to multidrug-resistant Pseudomonas aeruginosa: epidemiology and treatment options. Pharmacotherapy 2005; 25: 1353–1364.
Falagas ME, Karageorgopoulos DE . Pandrug resistance (PDR), extensive drug resistance (XDR), and multidrug resistance (MDR) among Gram-negative bacilli: need for international harmonization in terminology. Clin Infect Dis 2008; 46: 1121–1122.
Falagas ME, Koletsi PK, Bliziotis IA . The diversity of definitions of multidrug-resistant (MDR) and pandrug-resistant (PDR) Acinetobacter baumannii and Pseudomonas aeruginosa. J Med Microbiol 2006; 55: 1619–1629.
Hachem RY, Chemaly RF, Ahmar CA, Jiang Y, Boktour MR, Rjaili GA et al. Colistin is effective in treatment of infections caused by multidrug-resistant Pseudomonas aeruginosa in cancer patients. Antimicrob Agents Chemother 2007; 51: 1905–1911.
Acknowledgements
We are thankful to the patients and Elodie Choisy.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on the Spinal Cord website
Rights and permissions
About this article
Cite this article
Saliba, M., Saadeh, D., Bouchand, F. et al. Outcome of bloodstream infections among spinal cord injury patients and impact of multidrug-resistant organisms. Spinal Cord 55, 148–154 (2017). https://doi.org/10.1038/sc.2016.176
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/sc.2016.176