Abstract
Hypothyroidism was confirmed to be associated with both dyslipidemia and renal dysfunction. However, the impact of thyroid function on the relationship between serum lipid levels and renal function has never been given sufficient attention. In this large-scale multicenter cross-sectional study, the ratio of triglyceride to high-density lipoprotein cholesterol (TG/HDL) and the prevalence of hypothyroidism in CKD subjects were significantly higher than those in non-CKD ones (P < 0.001). After adjustment for potential confounding factors, TG/HDL was shown to be significantly associated with serum Cr levels (β = 0.551; 95%CI, 0.394–0.708) and eGFR (β = −0.481; 95%CI, −0.731–−0.230). The risk for CKD was significantly increased as TG/HDL ratio was elevated (adjusted odds ratio = 1.20; 95%CI, 1.11–1.27). These significant associations were found among subjects with euthyroidism and hypothyroidism rather than hyperthyroidism. Furthermore, the associations between TG/HDL and Cr or CKD status were significantly greater in hypothyroidism than those in euthyroidism (P < 0.05). These results suggested that elevated TG/HDL ratio was associated with renal dysfunction; it exhibited a significantly stronger association with Cr and CKD in hypothyroidism than in euthyroidism. Therefore, more attention should be paid on lipid profile to prevent or delay the occurrence and progression of renal dysfunction, especially for those with hypothyroidism.
Similar content being viewed by others
Introduction
Renal dysfunction is becoming a serious public health issue worldwide due to its high prevalence and significant association with the morbidity and mortality of many fatal chronic diseases1,2. It is highly desirable to identify and manage the risk factors associated with renal dysfunction. Evidence suggesting that abnormal lipid metabolism may be a possible cause of kidney dysfunction has mounted significantly in recent years3,4. High triglyceride (TG) levels and/or low high-density lipoprotein cholesterol (HDL-C) levels were illustrated to predict an increased risk of renal dysfunction in many studies5,6,7. Recently, the ratio of TG/HDL, a more reasonable indicator of insulin resistance and cardiovascular events, has increasingly drawn researchers’ attention8. Actually, the association between TG/HDL and chronic kidney disease (CKD) has been confirmed in Korean adults9 and Japanese population4 and it was also shown to be the unique lipid-related ratio independently associated with CKD stage 3 or more10. Nevertheless, none of the above researches considered the other confounding lipid metabolism factors including total cholesterol and low-density lipoprotein cholesterol in their statistical analyses. Furthermore, few attempts were systematically conducted, especially for large-scale Chinese population, to explore the association between TG/HDL and the renal function parameters including serum creatinine (Cr), estimated glomerular filtration rate (eGFR) and CKD status.
On the other hand, hypothyroidism, the most common thyroid dysfunction11, has been confirmed to be associated with both dyslipidemia and renal dysfunction in a lot of epidemiological studies7,11,12,13. However, it remains poorly elucidated whether thyroid function has impact on the relationship between TG/HDL and renal function. Sometimes even when exposed to the same TG/HDL level, renal function might be different from one individual to another according to different thyroid function status. Some subjects could experience marked changes in renal function, while others were unresponsive. Thus, the interactions between TG/HDL and thyroid function might play important roles in the pathogenesis of renal dysfunction and should be further explored.
Thus, based on REACTION study, we first systematically detected the association between TG/HDL and the renal function parameters including Cr, eGFR and CKD status and further ascertained the impact of thyroid function on this relationship in a large multicenter Chinese population. Our results may have important clinical implications for guidelines aiming at preventing renal disease.
Results
Clinical characteristics of the study population
Table 1 showed the clinical characteristics of the 22,133 participants (7,806 men and 14,327 women), with 268 subjects having CKD (the prevalence was 1.2%). Among participants with CKD, the median of TG/HDL was significantly higher and the prevalence of hypothyroidism was elevated. In addition, the CKD subjects had older age, higher percentage of female participants, increased blood pressure, elevated serum levels of lipid profiles, fasting plasma glucose and aspartate aminotrasferase.
The association between TG/HDL and renal function
Table 2 presented the univariate and multivariate association between TG/HDL and Cr, eGFR and risk of CKD in the linear mixed model (for Cr and eGFR) and generalized linear mixed model (for CKD status). As shown in Table 2, after adjustment for potential confounding factors, TG/HDL ratio was positively correlated with serum Cr levels (β = 0.551; 95%CI, 0.394–0.708) and there was significantly negative association between TG/HDL ratio and eGFR (β = −0.481; 95%CI, −0.731–−0.230). Consistently, the risk for CKD was increased as TG/HDL ratio was elevated (odds ratio = exp (β) = 1.20; 95%CI, 1.11–1.27). Subgroup analysis showed that the associations between TG/HDL and eGFR and CKD disappeared in males, while all adjusted associations between TG/HDL and the three renal function parameters could also be significantly found in the other three subgroups (Table S1-S4).
The association between TG/HDL and renal function according to thyroid function status
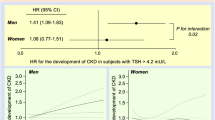
To determine the presence of Cr, eGFR and CKD status across the spectrum of TG/HDL, we stratified TG/HDL into three groups (tertiles) in different thyroid function status. As shown in Fig. 1 and Table 3, following the elevated TG/HDL, the trends of eGFR were gradually decreased in both euthyroidism (β = −1.37, P < 0.001) and hypothyroidism (β = −1.48, P < 0.001), respectively, but the trend in hyperthyroidism (β = −0.55, P = 0.31) was different from those in euthyroidism and hypothyroidism. Analogously, the trends for Cr and CKD status were also similar in euthyroidism and hypothyroidism but different from that in hyperthyroidism. Further adjusted investigation of the association between TG/HDL and renal function according to thyroid function status was shown in Table 3. TG/HDL ratio was not significantly correlated with all three renal function parameters among subjects with hyperthyroidism. The same phenomenon was observed in subgroup analysis (Table S5-S8). Significant associations emerged in euthyroidism and hypothyroidism, though the P value for eGFR in hypothyroidism was a little higher (P = 0.06) than given significance level. However, subgroup analysis illustrated that this phenomenon only existed in females and also in the group with age older than 65 years (Table S5-S8). Furthermore, compared to euthyroidism, the associations between TG/HDL and Cr and CKD status were significantly greater in subjects with hypothyroidism.
Correlation of TG/HDL with renal function according to thyroid function status.
The data are presented as the means (Cr and eGFR) or prevalence (CKD status). The tertile ranges are as follows: Tertile 1 (<0.79), Tertile 2 (0.79–1.38), Tertile 3 (>1.38). TG, triglyceride; HDL, high-density lipoprotein; Cr, creatinine; eGFR, estimated glomerular filtration rate; CKD, chronic kidney diseases.
Discussion
In this large-scale multicenter cross-sectional study, we first demonstrated that TG/HDL ratio was independently associated with Cr, eGFR and risk of CKD after adjustment of potential confounding factors. Then we confirmed that the associations between TG/HDL and renal function were greater in subjects with hypothyroidism than euthyroidism, while the significant association was not observed in hyperthyroidism. Our study indicated that TG/HDL ratio was associated with renal function and this association could be modified by thyroid function status.
As a considerably important lipid ratio, TG/HDL was used as a surrogate for small density LDL-C and insulin resistance and predicted coronary heart disease independently14,15. For the association between TG/HDL and renal function, several studies had obtained results similar to ours. Tsuruya K et al. observed that the prevalence of CKD, low eGFR and proteinuria increased significantly with elevating quartiles of TG/HDL-C in both genders in a large Japanese population4. Similarly, Kim J.Y. et al. showed that the prevalence with CKD stage 3 or more increased with increasing quartile group in both sexes in Koreans8. Remarkably, a follow-up study demonstrated that the TG/HDL-C ratio was positively associated with an increased risk of incident CKD in type 2 diabetes mellitus patients16. However, the above studies didn’t consider the other confounding lipid metabolism factors including total cholesterol and low-density lipoprotein cholesterol in their statistical analyses, or were performed in a specific population (for example, type 2 diabetes mellitus patients). In this study, we performed the analyses in a general population and observed the association between TG/HDL ratio and renal function after adjustment for potential confounding factors including serum cholesterol levels and thyroid function.
Another important finding for our present study was that the association between TG/HDL and renal function would become greater in hypothyroidism. Although intensive mechanism was not fully elucidated, hypothyroidism was confirmed to be closely associated with both dyslipidemia and renal dysfunction. In the Colorado research, lipid levels increased in a graded fashion as thyroid function declined12. In the HUNT study, Asvold B.O. et al. demonstrated that CKD was more common in subjects with hypothyroidism; even within the reference range, the prevalence of CKD was gradually increased as serum thyrotropin levels increased13. It seems quite clear that both renal function and lipid metabolism could be modulated by thyroid function. However, so far, no previous works paid attention to the influence of thyroid function on the relationship between TG/HDL and renal function. The present study illustrated the modification of thyroid function on the association between TG/HDL and renal function, suggesting that more attention should be paid to lipid profiles to prevent or delay the occurrence and progression of renal dysfunction, especially for those with hypothyroidism. Further laboratory studies are also essential to determine the involved mechanism.
In this large-scale multicenter study, a mixed model was employed to investigate the association between lipid and renal function. The mixed model is particularly useful in settings where measurements are made on clusters of related statistical units and subjects are observed nested within larger units. Within-cluster correlation is more likely to be captured in mixed model through adding random cluster effects into the traditional regression model17,18. In our study, data were collected from three different provinces (clusters) and subjects within each cluster were obviously correlated, thus mixed model was preferred. Further analysis showed that the estimated standard deviation of the random effects for Cr, eGFR and risk of CKD was 3.29, 7.01 and 1.39 respectively (data not shown) and all values were significantly higher than zero (P < 0.001), indicating that it was indeed necessary to incorporate random effects in the model.
Previous studies have provided strong evidence suggesting that lipid abnormality might lead to kidney dysfunction. In vivo studies, Levi M. et al. demonstrated that in mice fed a high-fat diet, lipids accumulated in the glomerular and tubulo-interstitial cells with increased expression of sterol regulatory element binding protein (SREBP), a transcription factor which plays a key role in lipogenesis. These changes were associated with significant glomerulosclerosis and proteinuria19,20. In addition, Tanaka Y. et al. showed a protecting effect of fenofibrate (a potent PPAR-α agonist) reducing glomerular lipid accumulation and oxidative stress associated with decreased albuminuria and glomerulosclerosis in mice fed a high-fat diet21. Further more, in vitro studies indicated that the mechanisms associated with lipid induced kidney injury may be linked to insulin resistance. The blocking of insulin signaling in podocytes and proximal tubular cells induced by palmitic acid or insulin receptor deletion may finally contribute to the renal dysfunction22,23. On the other hand, while several causes were determined to result in decreased GFR, the involved mechanisms have not been fully elucidated. Firstly, hypothyroidism is associated with pathophysiological status which could lead to decreased renal perfusion, including decreased cardiac output and circulating volume, impaired activity of the renin-angiotensin-aldosterone system (RAAS) and a decreased atrial natriuretic peptide (ANP) level24,25,26. Secondly, growth retardation in the parenchyma of the kidney may lead to the decreased glomerular surface area27. Thirdly, in the proximal tubule, a filtrate overload caused by deficient sodium and water reabsorption could result in adaptive preglomerular vasoconstriction28. Fourthly, in the distal tubule, the decreased expression of the chloride channel ClC-2 contributed to the declined GFR by the tubulo-glomerular feedback29. Finally, a reduction of the expression of several glomerular vasodilators, including insulin-like growth factor 1 and vascular endothelial growth factor, might cause the reduction of GFR30. From the above, both lipid abnormality and hypothyroidism could result in renal dysfunction; this might be a plausible explanation for the greater effect of TG/HDL on renal function in subjects with hypothyroidism in the present study.
The prevalence of CKD based on eGFR was about 1.2% in the present study, which was lower than that in US population31. However, this prevalence was similar to that reported in the first national survey of CKD across China (1.7%)32. One plausible explanation for the lower prevalence of decreased eGFR in China might be that hypertension and diabetes have increased rapidly in the past 15–20 years in China, but for these diseases to affect CKD at a population level might take another 10 years33.
Recently, serum cystatin C was reported to be used as an alternative to serum Cr for estimating GFR. Vega A. et al. compared the accuracy of the recently used equations for estimating GFR and found that cystatin C was the most accurate method34. In Shlipak MG’s meta-analysis, the use of cystatin C strengthened the association between the eGFR and the risks of death and end-stage renal disease35. However, whether GFR estimated using cystatin C is superior to that using Cr requires additional studies. Utility of cystatin C could also be added in our future researches.
The strengths of our study included the relatively large sample size (n = 22,133) and the employment of mixed model for the analyses of the association between lipid and renal function in Chinese population and to our knowledge, this was the first study indicating the interactions between TG/HDL ratio and thyroid function on renal function. However, some limitations should also be mentioned. First, due to absence of urine sample, albuminuria was not able to be evaluated in the present study. Lack of albuminuria data might lead to misclassification of CKD, especially for those early-stage patients32. Therefore, it seems more appropriate to restrict our findings and conclusions to late CKD stages (3 to 5). In addition, proteinuria could lead to thyroid hormone loss with albumin, finally resulting in thyroid dysfunction. Since we investigated the modification effect of thyroid function on the relationship between TG/HDL and renal function, it was better to evaluate the urine data. Second, serum creatinine was measured using the Jaffé method and the measurements were essential to be corrected for further renal function estimation36. However, the Roche enzymatic assay, which is traceable to gold-standard reference methods, could not be implemented in our clinical laboratory. Therefore, the creatinine measurements were not corrected. The methods for serum creatinine measurements will be improved in our future study. Third, no distribution information of risk factors over the period of follow-up was available and thus no conclusions could be made about causal inference. Well-designed experimental research and prospective clinical studies were certainly warranted.
In conclusion, this large-scale multicenter cross-sectional study in Chinese population indicated that TG/HDL ratio was associated with renal dysfunction and it exhibited a significantly stronger association between Cr and CKD in hypothyroidism than in euthyroidism while no significant correlation was observed in subjects with hyperthyroidism. More attention should be paid to lipid profiles to prevent or delay the occurrence and progression of renal dysfunction, especially for those with hypothyroidism. Further laboratory studies are also needed to investigate the involved complex mechanism.
Methods
Study participants
The present large-scale multicenter cross-sectional study was part of the REACTION study which was a national community-based program37,38,39,40. Three communities were selected from Shandong, Gansu and Jiangsu Province, including both rural and urban areas with different degrees of urbanization and economic development. All registered Han Chinese residents aged 40 years and older who had lived in their current residence for at least 5 years were invited by telephone or door-by-door visits to undergo a screening examination at the specified hospital or local health clinics. A total of 24,256 persons participated and the response rate was over 85% for each community. All participants provided an overnight fasting blood sample as well as a self-reported questionnaire. The study has been approved by the ethics committee of Shanghai Jiao Tong University37 and the research was carried out in accordance with this approved guidelines. Written informed consent was obtained from each participant.
We excluded subjects based on the following criteria: (1) missing vital data, such as age, gender, lipid profiles, serum Cr and thyroid function; (2) complications or conditions that affect lipid metabolism, renal function and thyroid status, such as pregnancy, lactation, malignant tumors or severe hepatic dysfunction (either or both alanine aminotransferase and aspartate aminotransferase levels above 100 U/L); and (3) taking any medicine that affects the lipid metabolism, renal or thyroid function, such as statins, fibrates, nonsteroidal anti-inflammation drugs, diuretics, thyroid hormone, anti-thyroid drugs, amiodarone or steroid hormones in the past 3 months. Finally, a total of 22,133 subjects were selected and the excluded subjects were not significantly different from the total population in terms of age and gender.
Data collection
All study investigators successfully completed a training program. Training sessions were standardized and scripted for all testing sites to minimize instructor variability. Weight and height were measured, with body mass index calculated as the ratio of weight/height2. Waist circumference was measured in centimeters. Blood pressure was the mean value of the three 3-minute interval measurements for each individual with an electronic sphygmomanometer (HEM-7117; Omron, Kyoto, Japan). Gender, age and other essential information were obtained from the standard questionnaire by trained investigators41.
Blood samples were collected from all of the participants between 8:00 A.M. and 10:00 A.M. after a minimum 10-hour fast. The glucose samples were measured within two hours. Serum samples were separated and shipped on dry ice. Chemiluminescent methods (Cobas E601; Roche, Basel, Switzerland) were used to quantitate thyroid function based on free tri-iodothyronine (FT3), free thyroxine (FT4) and thyrotropin (TSH) levels. The serum lipid profiles and hepatic and renal function were determined using the ARCHITECT ci16200 Integrated System (Abbott, Illinois, USA) at the central laboratory in the Shanghai Institute of Endocrine and Metabolic Diseases. The intraassay and interassay coefficients of variation were always below 5% for all above parameters.
Definition of CKD and thyroid dysfunction
The eGFR was calculated using the simplified Modification of Diet in Renal Disease (MDRD) equation for Chinese42: eGFR (ml/min/1.73 m2) = 175 × Cr (mg/dl)−1.234 × age (year)−0.179 × (if, female × 0.79). CKD was defined as the eGFR below 60 ml/min/1.73 m2 43.
The thyroid dysfunction was defined based on serum TSH, FT4 and FT3 levels. The laboratory reference ranges were 3.1–6.8 pmol/L for FT3, 12–22 pmol/L for FT4 and 0.27–4.2 mIU/L for TSH. Euthyroidism was defined by TSH, FT4 and FT3 levels within the reference ranges. Hyperthyroidism was a condition with decreased TSH concentration and normal or increased thyroid hormones levels including both FT4 and FT3 and hypothyroidism was defined by elevated TSH levels and normal or decreased FT4 levels44.
Statistical analyses
All continuous variables were presented as means with standard deviations, or medians with interquartile ranges as appropriate, based on whether the distribution was normal or skewed, which was judged by histogram. Categorical data were summarized as percentage. We grouped subjects according to the development of CKD and compared continuous variables with two sample T-test or Wilcox rank sum test and categorical variables with chi-square test.
Considering the data were obtained from different clusters (provinces), mixed model was preferred since it was better to capture the specific within-cluster correlation through adding random cluster effects into the traditional regression model. The details of the mixed model were shown in the Supplemental Materials. We conducted linear mixed model17 to examine the associations between TG/HDL and Cr and eGFR, while generalized linear mixed model with “logit” link function was used for CKD status18. In addition to TG/HDL, independent variables included in the multivariate adjusted mixed model for Cr were age, gender, body mass index, waist circumference, total cholesterol, low-density lipoprotein cholesterol, fasting plasma glucose, systolic blood pressure, diastolic blood pressure, alanine aminotransferase, aspartate aminotransferase and thyroid function status, while all factors except age and gender were adjusted for eGFR and CKD given that these two dependent variables are derived from age and gender. U-test was then adopted to compare the difference of the association between TG/HDL and renal function (regression coefficients) between euthyroidism and hypothyroidism. Furthermore, we also conducted four subgroup analyses including male, female, age less or equal to 65 and age larger than 65. Two-sided P values less than 0.05 were considered to be significant. All analyses were performed with R package lme4 (http://cran.r-project.org/).
Additional Information
How to cite this article: Yuan, Z. et al. Thyroid function modifies the association between ratio of triglyceride to high-density lipoprotein cholesterol and renal function: a multicenter cross-sectional study. Sci. Rep. 5, 11052; doi: 10.1038/srep11052 (2015).
References
Matsushita, K. et al. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet 375, 2073–2081 (2010).
Go, A. S., Chertow, G. M., Fan, D., McCulloch, C. E. & Hsu, C. Y. Chronic kidney disease and the risks of death, cardiovascular events and hospitalization. N Engl J Med 351, 1296–1305 (2004).
Guebre-Egziabher, F. et al. Ectopic lipid accumulation: A potential cause for metabolic disturbances and a contributor to the alteration of kidney function. Biochimie 95, 1971–1979 (2013).
Tsuruya, K. et al. Association of the triglycerides to high-density lipoprotein cholesterol ratio with the risk of chronic kidney disease: analysis in a large Japanese population. Atherosclerosis 233, 260–267 (2014).
Ritz, E. & Wanner, C. Lipid changes and statins in chronic renal insufficiency. J Am Soc Nephrol 17, S226–230 (2006).
Parikh, N. I. et al. Cardiovascular disease risk factors in chronic kidney disease: overall burden and rates of treatment and control. Arch Intern Med 166, 1884–1891 (2006).
Muntner, P. et al. The prevalence of nontraditional risk factors for coronary heart disease in patients with chronic kidney disease. Ann Intern Med 140, 9–17 (2004).
Pacifico, L. et al. Association of serum triglyceride-to-HDL cholesterol ratio with carotid artery intima-media thickness, insulin resistance and nonalcoholic fatty liver disease in children and adolescents. Nutr Metab Cardiovasc Dis 24, 737–743 (2014).
Kang, H. T. et al. Association between the ratio of triglycerides to high-density lipoprotein cholesterol and chronic kidney disease in Korean adults: the 2005 Korean National Health and Nutrition Examination Survey. Kidney Blood Press Res 34, 173–179 (2011).
Kim, J. Y., Kang, H. T., Lee, H. R., Lee, Y. J. & Shim, J. Y. Comparison of lipid-related ratios for prediction of chronic kidney disease stage 3 or more in Korean adults. J Korean Med Sci 27, 1524–1529 (2012).
Cooper, D. S. & Biondi, B. Subclinical thyroid disease. Lancet 379, 1142–1154 (2012).
Canaris, G. J., Manowitz, N. R., Mayor, G. & Ridgway, E. C. The Colorado thyroid disease prevalence study. Arch Intern Med 160, 526–534 (2000).
Asvold, B. O., Bjoro, T. & Vatten, L. J. Association of thyroid function with estimated glomerular filtration rate in a population-based study: the HUNT study. Eur J Endocrinol 164, 101–105 (2011).
Salazar, M. R. et al. Identification of cardiometabolic risk: visceral adiposity index versus triglyceride/HDL cholesterol ratio. Am J Med 127, 152–157 (2014).
Fan, X. et al. Triglyceride/high-density lipoprotein cholesterol ratio: a surrogate to predict insulin resistance and low-density lipoprotein cholesterol particle size in nondiabetic patients with schizophrenia. J Clin Psychiatry 72, 806–812 (2011).
Zoppini, G. et al. Triglyceride-high-density lipoprotein cholesterol is associated with microvascular complications in type 2 diabetes mellitus. Metabolism 61, 22–29 (2012).
Gilmour, A. R., Thompson, R. & Cullis, B. R. Average information REML: an efficient alogrithm for variance parameter estmation in linear mixed models. Biometrics 51, 1440–1450 (1995).
Breslow, N. & Clayton, D. Approximate inference in generalized linear mixed models. JAMA 88, 9–25 (1993).
Sun, L., Halaihel, N., Zhang, W., Rogers, T. & Levi, M. Role of sterol regulatory element-binding protein 1 in regulation of renal lipid metabolism and glomerulosclerosis in diabetes mellitus. J Biol Chem 277, 18919–18927 (2002).
Jiang, T. et al. Diet-induced obesity in C57BL/6J mice causes increased renal lipid accumulation and glomerulosclerosis via a sterol regulatory element-binding protein-1c-dependent pathway. J Biol Chem 280, 32317–32325 (2005).
Tanaka, Y. et al. Fenofibrate, a PPARalpha agonist, has renoprotective effects in mice by enhancing renal lipolysis. Kidney Int 79, 871–882 (2011).
Soumura, M. et al. Oleate and eicosapentaenoic acid attenuate palmitate-induced inflammation and apoptosis in renal proximal tubular cell. Biochem Biophys Res Commun 402, 265–271 (2010).
Lennon, R. et al. Saturated fatty acids induce insulin resistance in human podocytes: implications for diabetic nephropathy. Nephrol Dial Transplant 24, 3288–3296 (2009).
Gillum, D. M., Falk, S. A., Hammond, W. S. & Conger, J. D. Glomerular dynamics in the hypothyroid rat and the role of the renin-angiotensin system. Am J Physiol 253, F170–179 (1987).
Zimmerman, R. S., Gharib, H., Zimmerman, D., Heublein, D. & Burnett, J. C., Jr. Atrial natriuretic peptide in hypothyroidism. J Clin Endo Metab 64, 353–355 (1987).
Suher, M., Koc, E., Ata, N. & Ensari, C. Relation of thyroid disfunction, thyroid autoantibodies and renal function. Ren Fail 27, 739–742 (2005).
Bradley, S. E., Coelho, J. B., Sealey, J. E., Edwards, K. D. & Stephan, F. Changes in glomerulotubular dimensions, single nephron glomerular filtration rates and the renin-angiotensin system in hypothyroid rats. Life Sci 30, 633–639 (1982).
Zimmerman, R. S. et al. Cardiorenal endocrine dynamics during volume expansion in hypothyroid dogs. Am J Physiol 255, R61–66 (1988).
van Hoek, I. & Daminet, S. Interactions between thyroid and kidney function in pathological conditions of these organ systems: a review. Gen Comp Endocrinol 160, 205–215 (2009).
Schmid, C., Brandle, M., Zwimpfer, C., Zapf, J. & Wiesli, P. Effect of thyroxine replacement on creatinine, insulin-like growth factor 1, acid-labile subunit and vascular endothelial growth factor. Clin Chem 50, 228–231 (2004).
Grams, M. E. et al. Trends in the prevalence of reduced GFR in the United States: a comparison of creatinine- and cystatin C-based estimates. Am J Kidney Dis 62, 253–260 (2013).
Zhang, L. et al. Prevalence of chronic kidney disease in China: a cross-sectional survey. Lancet 379, 815–822 (2012).
Zhang, L. & Wang, H. Chronic kidney disease epidemic: cost and health care implications in China. Semin Nephrol 29, 483–486 (2009).
Vega, A. et al. Evaluation of methods based on creatinine and cystatin C to estimate glomerular filtration rate in chronic kidney disease. Int Urol Nephrol 46, 1161–1167 (2014).
Shlipak, M. G. et al. Cystatin C versus creatinine in determining risk based on kidney function. N Engl J Med 369, 932–943 (2013).
Selvin, E. et al. Calibration of serum creatinine in the National Health and Nutrition Examination Surveys (NHANES) 1988-1994, 1999-2004. Am J Kidney Dis 50, 918–926 (2007).
Ning, G. Risk Evaluation of cAncers in Chinese diabeTic Individuals: a lONgitudinal (REACTION) study. J Diabetes 4, 172–173 (2012).
Bi, Y. et al. Cohort profile: risk evaluation of cancers in Chinese diabetic individuals: a longitudinal (REACTION) study. J Diabetes 6, 147–157 (2014).
Lu, J. et al. The relationship between insulin-sensitive obesity and cardiovascular diseases in a Chinese population: results of the REACTION study. Int J Cardiol 172, 388–394 (2014).
Ning, G. & Bloomgarden, Z. Diabetes and cancer: findings from the REACTION studyREACTION. J Diabetes 7, 143–144 (2015).
Luepker, R. V., Evans, A., McKeigue, P. & Reddy, K. S. Cardiovascular survey methods. (World Health Organization, Geneva, 2004).
Ma, Y. C. et al. Modified glomerular filtration rate estimating equation for Chinese patients with chronic kidney disease. J Am Soc Nephrol 17, 2937–2944 (2006).
Wanner, C. & Tonelli, M. KDIGO Clinical Practice Guideline for Lipid Management in CKD: summary of recommendation statements and clinical approach to the patient. Kidney Int 85, 1303–1309 (2014).
Garber, J. R. et al. Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Thyroid 22, 1200–1235 (2012).
Acknowledgements
This research was supported in part by grants from the National Natural Science Foundation (81430020 and 81273177), the Special Fund for Shandong Province Post-doctoral Innovation (2014), the National Clinical Research Center for Metabolic Diseases (2013BAI09B13) and the National Key New Drug Creation and Manufacturing Program of Ministry of Science and Technology (2012ZX09303006-001). The authors gratefully acknowledge the Reaction Study Group for organizing the REACTION Study which was a national epidemiological survey.
Author information
Authors and Affiliations
Contributions
L.G. and J.Z. designed research; Z.Y., M.Z., H.Z., X.Z., Q.G. and G.N. conducted research; B.Z. offered essential reagents/materials; Z.Y. and F.X. analyzed data; Z.Y. and M.Z. wrote manuscript; the REACTION Study Group organized the REACTION study which was a national epidemiological survey; F.X. and J.Z. had primary responsibility for final content. All authors read and approved the final manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Yuan, Z., Zhao, M., Zhang, B. et al. Thyroid function modifies the association between ratio of triglyceride to high-density lipoprotein cholesterol and renal function: a multicenter cross-sectional study. Sci Rep 5, 11052 (2015). https://doi.org/10.1038/srep11052
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep11052