Abstract
The aim of our study was to assess the theoretical and practical knowledge of French obstetricians about the surgical management of postpartum haemorrhage (PPH). Our study is a national anonymous self-administered survey. A total of 363 obstetricians responded to this questionnaire between December 2013 and April 2014. Questionnaire sent through email to all French obstetricians who are members of either of two federations of hospital-based obstetricians. Answers were collected until the end of June 2014. The main outcome measure was obstetricians’ level of mastery of each surgical technique. The results were analysed descriptively (proportions). Only the 286 questionnaires fully completed were analysed; the complete response rate was 23% (286/1246). In all, 33% (95/286) of the responding obstetricians reported that they had not mastered sufficiently or even at all the technique for bilateral ligation of the uterine arteries, 37% (105/286) for uterine compression suture, 62% (178/286) for ligation of the internal iliac arteries, and 47% (134/286) for emergency peripartum hysterectomy. In all, 18% (52/286) of respondents stated that they had not mastered any of these techniques. Our study shows that a worrisome number of French obstetricians reported insufficient mastery of the surgical techniques for PPH management.
Similar content being viewed by others
Introduction
Postpartum haemorrhage (PPH) remains the leading cause of maternal mortality both worldwide, causing 150 000 deaths a year, and in France, where it accounts for 15.5% of maternal deaths1. Approximately 1.7% of births are complicated by severe PPH (blood loss ≥ 1000 ml in the 24 hours after delivery)2. It appears that at least 80% of maternal deaths from PPH are avoidable, since they appear very often to follow a delay in diagnosis or management, or insufficient treatment3.
A recent observational study in France observed that arterial embolization is used in 2.7% (183/6660) of PPH, while uterine-sparing surgical procedures are used in 1.3% (86/6660) and hysterectomy in 1.1% (72/6660)4. A retrospective study in Ireland found that the prevalence of emergency hysterectomy after PPH was around 1/2000 deliveries5. Surgical treatment of PPH is used as a last resort when earlier procedures (prostaglandins, intrauterine tamponade, embolization) have failed, or sometimes from the start, when a severe life-threatening PPH requires that bleeding stop in the shortest time possible. All obstetricians can face these situations during their practice. They must therefore have the surgical skills to perform a hysterectomy, even if they work in a facility where they can seek help from a colleague on-call at home, or an abdominal surgeon on-call onsite. Failure to perform a surgical procedure necessary for PPH, most especially an emergency hysterectomy, or delay due to awaiting assistance from a colleague can lead to criminal and civil liability.
The principal objective of our study was to assess the theoretical and practical knowledge of French obstetricians about the surgical management of PPH. As secondary objectives, we sought to determine the surgical procedure that they would use as first, second, and third line treatments.
Material and Methods
Our study is an anonymous survey, self-administered online. French obstetricians working in either the private or public sector and members of one of two federations of French hospital-based obstetricians (the federation of perinatal networks or the federation of circles of gynaecologists-obstetricians in non-university hospital centres) (n = 1248) received an explanatory email with a link to a survey containing 60 questions.
A first email was sent to each obstetrician in December 2013, and reminders were sent in February and in April, 2014. Only fully completed questionnaires were analysed. We considered a questionnaire fully completed when every question had a response (or several, when more than one choice was allowed). Answers were collected until the end of June 2014. Informed consent was obtained from all participants. The study protocol was approved by the Committee of Ethics and Research in Gynaecology-Obstetrics (CEROG-2014-08) and conducted in accordance with relevant guidelines.
The obstetricians worked in different types of maternity units. In France, these are classified in 3 levels: level III (full-time obstetric, paediatric, neonatal intensive care and anaesthesia staff) for premature births before 32 weeks of gestation, level II (full-time obstetric, paediatric and anaesthesia staff, and no long-term assisted ventilation) for premature births after 32 weeks of gestation and level I (no facilities for special care)6.
Because our research found no validated questionnaire about the topic of our survey in the literature, we — that is, all the co-authors — designed our own questionnaire, which was approved by CEROG. Evidence supports the reliability of self-assessment of technical skills in surgery7.
Some questions were dichotomous, and others open-ended. The questionnaire was designed on the website of www.limesurvey.com; responses were forced for each question, skip logic and a progress bar were used, and data were collected via Web-link and email and downloaded to a spreadsheet.
Each email sent to the obstetricians included a cover letter informing them of the time we estimated it would take them to complete the questionnaire (10–15 minutes) and stating that participation was voluntary, anonymous and unremunerated. An internet link enabled the physicians to accede to the questionnaire and complete it online. Unique identifiers were assigned to each participant’s computer, thereby ensuring that each individual could complete only one questionnaire.
The final questionnaire (Appendix) contained 3 sections. The first comprised demographic and institutional questions (n = 21). The second focused on the participants’ theoretical and practical knowledge (36 questions). The third section included questions about the sequence of techniques that they would use for surgical management of PPH for a young woman who wanted more children, was haemodynamically stable and managed by a multidisciplinary team (surgeon and anaesthesiologist) (3 questions).
The different surgical techniques mentioned in the questionnaire were: uterine compression sutures (UCS), including the B-Lynch and Cho suturing techniques8,9, bilateral uterine artery ligation (UAL)10, triple uterine artery ligation (TUAL)11,12, peripartum hysterectomy (PH)13, bilateral internal iliac artery ligation (IIAL), and stepwise uterine devascularisation (SUD)14,15,16.
The principal endpoint of the study was the obstetricians’ self-assessed level of mastery of each surgical technique that might be performed during the management of severe PPH. The physicians were asked for each technique whether they considered that they had mastered it completely, sufficiently, insufficiently, or not at all (questions 27, 33, 39, 45, 51 and 57).
As secondary outcome measures, we asked participants what surgical technique they would use as first, second, and third line treatments for severe PPH (questions 58–60).
Descriptive statistics were used to detail demographic characteristics, theoretical and practical knowledge, and the different management strategies employed by survey participants. For the quantitative data, comparisons were performed with the Mann-Whitney-Wilcoxon test for independent samples. Proportions were compared with the chi-square test. We used SPSS software, version 15.0 for Windows, SPSS Inc., Chicago, IL, USA. Statistical significance was defined as a P value < 0.05.
Results
When we take incomplete as well as unreturned questionnaires into account, the participation rate was 23% (286/1246); there were 286 complete responses. The 77 questionnaires not fully completed were excluded from the study.
Table 1 summarises the participants’ demographic data. Their median age was 45 years (range: 35–55). The mean age of hospital staff physicians was not significantly different from that of the physicians working exclusively in the private sector (respectively, 45.9+/−4.6 and 46.0+/4.7; P = 0.9). The mean time in practice since the end of their residencies was 15.5+/−11.7 years. Most (78%, 224/286) worked in the public sector; 57% (164/286) were hospital staff physicians. Preferred subspecialties were obstetrics 55% (156/286), surgery 32% (93/286), prenatal diagnosis 9% (25/286) and reproductive medicine 4% (12/286). The median number of on-call duty sessions monthly was 4 (range: 3–5), and 46% (133/286) worked in level III units. Almost all (98%, 279/286) reported that they could always call a colleague if needed. Sixty percent (171/286) reported that their department had a written protocol for surgical management of severe PPH.
An embolization centre was available onsite for 51% (145/286) and a blood bank for 56% (160/286). On the other hand, 85 doctors (26%) worked more than 20 km from an embolization centre.
Surgical management of PPH was considered extremely stressful by 22% (63/286) and stressful by 66% (190/286).
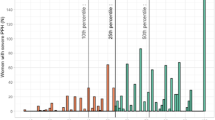
Overall, 93% (267/286) of participants considered that they knew the theory of the UCS techniques, 98% (279/286) UAL, 89% (255/286) TUAL, 31% (89/286), SUD, 97% (278/286) IIAL and 99% (284/286) PH. On the other hand, 37% (105/286) reported they had not mastered the techniques of UCS, 33% (95/286) UAL, 40% (115/286) TUAL, 86% (247/286) SUD, 62% (178/286) IIAL, and 47% (134/286) PH. Moreover, 18% (52/286) reported that they had not mastered any of these techniques.
As Table 2 shows, 49% (140/286) had performed UCS alone, without help from a colleague, 57% (163/286) UAL, 47% (134/286) TUAL, 8% (22/286) SUD, 33% (93/286) IIAL, and 54% (154/286) a PH, while 27% (77/286) had never performed any of these procedures alone. In addition, 17.5% (50/286) had already performed UCS with a colleague, 17% (48/276) UAL, 15% (44/286) TUAL, 2% (6/286) SUD, 26% (74/286) IIAL and 34% (97/286) PH. At the same time, 26% (74/286), had never seen UCS performed, 31% (90/286) TUAL, or 24% (68/286) IIAL (Table 2).
These obstetricians considered that UCS could be completely mastered after performing 5 procedures (IQR: 3–10), UAL 4 (1–5), TUAL 5 (3–10), SUD 4 (1–5.5), IIAL 9 (3–20) and PH 8 (4–10). Table 3 reports these results as medians and their interquartile ranges. Comparing the median of the IIAL to that for UAL (9 vs 4), that for TUAL (9 vs 5) and finally that for UCS (9 vs 5) shows a significant difference in all 3 cases (P < 0.05).
In response to a hypothetical severe PPH requiring surgical management in a young, haemodynamically stable woman who wanted to be able to have more children, 51% (145/286) of the obstetricians said that their first line treatment would be a distal ligation technique (UAL, TUAL or SUD), 36% (103/286) UCS, 12% (35/286) IIAL and 1% (2/286) PH. Their second line choices were distal ligation (39%, 111/286), IIAL (32%, 90/286), UCS (17%, 50/286) and PH (11%, 32/286). Finally, their third-line choices were PH (55%, 156/286), IIAL (26%, 74/286), UCS (7%, 21/286) and distal ligation (1%, 3/286). Table 4 reports these results.
The surgical sequences used most often by the obstetricians were: (1) distal ligation (TUAL or UAL), then IIAL, and then PH for 22% of the participants, and (2) UCS, then distal ligation, then IIAL, and then PH for 18%.
Discussion
Our study shows that most participants report that they know the theory of the different surgical techniques that can be used for severe PPH. On the other hand, a worrisome number of obstetricians (18%) reported they had not mastered any of these techniques, and 47% that they had not sufficiently (or not at all) mastered the technique of hysterectomy, the last-ditch treatment for severe PPH.
The high proportion of obstetricians with limited surgical skills for dealing with severe PPH may be the cause of the delayed management observed in deaths due to PPH in France1. Fortunately, 98% of the respondents reported that they could always call a colleague if they were having difficulty managing a case of severe PPH.
It is reassuring to note that 99% of participants report that their unit has a written protocol for medical management of PPH. Nonetheless, only 60% of participants mentioned the existence of a written protocol for its surgical management. Current French guidelines for PPH recommend that each obstetrical unit draft a full protocol for surgical management based on the local conditions and especially the environment quickly available in delivery room17.
Several hypotheses may explain the low level of mastery of this set of surgical techniques. First, the advent of uterine artery embolization in France has reduced recourse to haemostatic surgery in cases of severe PPH: embolization is used here at a rate at least double that of both uterine-sparing surgical procedures and hysterectomy4,13,18.
Second, developments in surgical technique and especially the emergence of laparoscopy for gynaecologic surgery may have contributed to reducing the practice and/or learning of laparotomic hysterectomies by obstetricians19, especially the youngest20.
Finally, early orientation during residency in gynaecology-obstetrics toward subspecialties such as prenatal diagnosis or reproductive medicine may be reducing the exposure of young obstetricians to the practice of laparotomic hysterectomies.
As a first line treatment, these obstetricians preferred the use of distal ligation techniques (51%) or uterine compression sutures (36%) to those for IIAL (12%). The learning curves for the first two appear to be significantly faster than that for the latter. Participants considered that they had mastered the distal ligation or uterine compression techniques after 4 or 5 procedures while it took them 9 to master IIAL. We have not found other studies in the literature comparing the perceptions of physicians about the number of procedures to be performed before mastery. On the other hand, several authors have already mentioned that IIAL is a difficult procedure, especially in emergencies; it requires real learning and practice and is not very reproducible, except perhaps by gynaecological surgeons specialised in oncology21,22.
Moreover, IIAL appears to be less effective than UAL or UCS techniques13,14,21. Doumouchtsis et al. have reviewed the literature about the effectiveness of ligation of the internal iliac arteries23. They report a mean effectiveness rate for IIAL of 69% compared with 93% for UAL and 83% for uterine compression23. No comparative study has yet demonstrated the superiority of one of these techniques compared with another. Accordingly there are no international guidelines proning the use of one technique of conservative surgery compared with another24,25.
Nonetheless, given the high number of physicians (18%) mastering none of these techniques for haemostatic surgery and the long learning time for IIAL, and considering that most obstetricians do not subspecialise in gynaecologic oncology surgery, it appears important to focus training on mastery of UAL, UCS and hysterectomy. Accordingly, our team12,26 uses UAL or uterine compression (but not IIAL) as the first line conservative choice when PPH is resistant to medical treatment.
No guidelines provide specific indications for postpartum hysterectomy27. The Royal College of Obstetricians and Gynaecologists (RCOG) recommend hysterectomy “sooner rather than later” and with the assistance of a second consultant25. French guidelines note that peripartum hysterectomy must be considered as the first line surgical treatment of massive PPH that is not responsive to earlier interventions or which is accompanied by cardiovascular instability17.
Different paedagogical tools are available to develop continuing medical education and to promote the learning of these techniques: videos of techniques performed in real time available on DVD28 or the internet29, the acquisition of different surgical techniques with the help of specific books30,31 or instructional charts17,21 or participation in simulation workshops32, such as those proposed by the RCOG33.
It is important that obstetricians be aware of the various learning difficulties. Despite the presence of different pedagogical tools, experienced obstetricians mastering the complex surgical techniques should take part in promoting and teaching these skills among their junior and less experienced colleagues. Moreover, they could assist their fellow senior obstetricians less at ease with these techniques in order to expedite their learning34.
On the other hand, the national Obstetrics and Gynecology residency training program should include special training modules on the surgical management of PPH, using all the pedagogical tools previously mentioned. Finally, considering the relative rare occurrence of PPH in everyday practice, workshops and seminars on the surgical management should be part of the continuous medical education programs in the annual congresses and meetings attended by obstetricians.
This study has significant strengths and is, to our knowledge, the first to assess obstetricians’ theoretical and practical knowledge about the surgical management of PPH. Data came from a large survey with a diverse range of participants from throughout France. Our study has several limitations: it was a self-reported survey with a low response rate and what might be viewed as limited generalizability. In particular, respondents in private practice are probably underrepresented35. In France, 35% of deliveries take place in the private sector while 12% of participants reported working solely in this sector and 10% working both in the private and public sectors35. Most respondents (57%) reported that they worked in the public sector; the mean age of these two groups was, however, similar.
In conclusion, our survey showed that 18% of responding obstetricians working onsite on-call duty at hospitals reported that they had not mastered any of the techniques of emergency obstetric surgery. Moreover, 47% reported that they had not mastered sufficiently (or at all) the technique of hysterectomy, which is the essential procedure for maternal salvage in severe PPH resistant to medical treatment. Our results suggest there are extreme deficiencies in the training of modern day obstetricians in France, and that adjustments in the national residency training program are required to address these weaknesses. It might be useful for other countries to perform a similar survey to help determine if these alarming results are particular to France.
Additional Information
How to cite this article: Bouet, P.-E. et al. Surgical management of postpartum haemorrhage: survey of French obstetricians. Sci. Rep. 6, 30342; doi: 10.1038/srep30342 (2016).
References
Deneux-Tharaux, C., Bonnet, M. P. & Tort, J. Epidemiology of post-partum haemorrhage. J Gynecol Obstet Biol Reprod. 43, 936–950 (2014).
Dupont, C. et al. Incidence and management of postpartum haemorrhage following the disseminations of guideline in a network of 16 maternity units in France. Int J Obstet Anesth. 18, 320–7 (2009).
Sentilhes, L. et al. Postpartum hemorrhage: Guidelines for clinical practice - Text of the guidelines (short text). J Gynecol Obstet Biol Reprod. 43, 1170–1179 (2014).
Kayem, G., Dupont, C., Bouvier-Colle, M. H., Rudigoz, R. C. & Deneux-Tharaux, C. Invasive therapies for primary postpartum haemorrhage: a population-based study in France. BJOG, doi: 10.1111/1471-0528.13477 (2015).
Flood, K. M. et al. Changing trends in peripartum hysterectomy over the last 4 decades. Am J Obstet Gynecol. 200, 632.e1–6 (2009).
Ancel, P. Y., Goffinet, F. & EPIPAGE 2 Writing Group. EPIPAGE 2: a preterm birth cohort in France in 2011. BMC Pediatr. 14, 97 (2014).
Rizan, C., Ansell, J., Tilston, T. W., Warren, N. & Torkington, J. Are general surgeons able to accurately self-assess their level of technical skills? Ann R Coll Surg Engl. 97, 549–55 (2015).
B-Lynch, C., Coker, A., Lawal, A. H., Abu, J. & Cowen, M. J. The B-Lynch surgical technique for the control of massive postpartum haemorrhage: an alternative to hysterectomy? Five cases reported. BJOG. 104, 372–5 (1997).
Sentilhes, L. et al. B-Lynch suture for massive persistent postpartum hemorrhage following stepwise uterine devascularization. Acta Obstet Gynecol Scand. 16, 1–7 (2008).
O’Leary, J. A. Uterine artery ligation in the control of postcesarean hemorrhage. J Reprod Med. 40, 189–193 (1995).
Tsirulnikov, M. S. La ligature des vaisseaux utérins au cours des hémorragies obstétricales. J Gynecol Obstet Biol Reprod. 8, 751–753 (1979).
Sentilhes, L. et al. Fertility and pregnancy outcomes following uterine devascularization for postpartum haemorrhage. Hum Reprod. 23, 1087–92 (2008).
Sentilhes, L., Kayem, G. & Descamps, P. Factors associated with peripartum hysterectomy. Obstet Gynecol. 114, 927 (2009).
Sentilhes, L. & Descamps, P. Which surgery should be the first-line uterine-sparing procedure to control severe postpartum hemorrhage? Fertil Steril. 95, e71 (2011).
AbdRabbo, S. Stepwise uterine devascularization: a novel technique for management of uncontrollable postpartum hemorrhage with preservation of the uterus. Am J Obstet Gynecol. 171, 694–700 (1994).
Sentilhes, L. et al. Fertility after B-Lynch suture and stepwise uterine devascularization. Fertil Steril. 91, 934.e5–9 (2009).
Sentilhes, L. et al. Guidelines for clinical practice from the French College of Gynaecologists and Obstetricians. Eur J Obstet Gynecol Reprod Biol. In press (2016).
Sentilhes, L. et al. Fertility and pregnancy following pelvic arterial embolization for postpartum haemorrhage. BJOG. 117, 84–93 (2010).
Perron-Burdick, M., Calhoun, A., Idowu, D., Pressman, A. & Zaritsky, E. Minilaparotomy vs. laparoscopic hysterectomy: comparison of length of hospital stay. J Minim Invasive Gynecol. 21, 619–23 (2014).
Washburn, E. E., Cohen, S. L., Manoucheri, E., Zurawin, R. X. & Elnarsson, J. I. Trends in reported resident surgical experience hysterectomy. J Minim Invasive Gynecol. 21, 1067–70 (2014).
Sentilhes, L. et al. Traitements chirurgicaux et alternatives non médicales des hémorragies de la délivrance. EMC Techniques chirurgicales. p1–20, 41–905 (2010).
Ducarme, G. et al. Surgical management of peripartum hemorrhage: a retrospective study. Gynecol Obstet Fertil. 35, 1209–14 (2005).
Doumouchtsis, S. K., Papageorghiou, A. T. & Arulkumaran, S. Systematic review of conservative management of postpartum hemorrhage: what to do when medical treatment fails. Obstet Gynecol Surv. 62, 540–7 (2007).
American College of Obstetricians and Gynecologists. Clinical Management Guidelines for Obstetricians-Gynecologists: postpartum hemorrhage. ACOG Practice bulletin no. 76. Obstet Gynecol. 108, 1039–47 (2006).
Royal College of Obstetrician and Gynaecologists. Postpartum hemorrhage: prevention and management. April 2011. Available at: http://www.rcog.uk/womens-health/clinical-guidance/prevention-and-management-postpartum-haemorrhage-green-top-52. Accessed Nov. 1, 2013.
Sentilhes, L. et al. Predictors of failed pelvic arterial embolization for severe postpartum hemorrhage. Obstet Gynecol. 113, 992–9 (2009).
Dahlke, J. D. et al. Prevention and management of postpartum haemorrhage: a comparison of 4 national guidelines. Am J Obstet Gynecol. 213, 76.e1–10 (2015).
Resch, B. et al. Prise en charge chirurgicale des hémorragies de la délivrance. Techniques chirurgicales et obstétricales en vidéo. http://www.cngof.asso.fr/D_PAGES/MARCH_00.HTM#video (2006) Date of access: 04/02/2016.
Joshi, V. M. Internal iliac artery ligation. http://www.youtube.com/watch?v=_Tbb_M (2013) Date of access 04/02/2016.
Arulkumaran, S., Karoshi, M., Keith, L. G., Lalonde, A. B. & B-Lynch, C. A comprehensive textbook of postpartum hemorrhage. An essential clinical referrence for effective management (2nd edition). Sapiens Publishing Ltd, London, 2012.
Deruelle, P., Kayem, G. & Sentilhes, L. Chirurgie en obstétrique. Chirurgie de la femme enceinte et de l’accouchement. Elsevier-Masson, Paris, 2015.
Fialkow, M. F. et al. An in situ standardized patient-based simulation to train postpartum hemorrhage and team skills on a labor and delivery unit. Simul Healthc. 9, 65–71 (2014).
Yoong, W., Karoshi, M., Lodhi, W. & Navaratnarajah, R. Masterclass in management of PPH. https://www.rcog.org.uk/globalassets/events/masterclass-in-management-of-pph-programme.pdf (2015) Date of access 04/02/2016.
Rashid, P., Narra, M. & Woo, H. Mentoring in surgical training. ANZ J Surg. 85, 225–9 (2015).
Blondel, B. & Kermarec, M. Enquête Nationale Périnatale 2010. Les naissances en 2010 et leur évolution depuis 2003. http://www.sante.gouv.fr/IMG/pdf/Les_naissances_en_2010_et_leur_evolution_depuis_2003.pdf (2003) Date of access 04/02/2016.
Author information
Authors and Affiliations
Contributions
P.E.B. analysed the data and wrote the first draft of the manuscript. L.S. conceived and designed the study, analysed the data and provided critical revision of the manuscript for important intellectual content. S.B., H.M., E.S. and B.M. made a substantial contribution to the acquisition of data. S.B., H.M., E.S. and B.M. provided critical revision of the manuscript for important intellectual content. All authors approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Bouet, PE., Brun, S., Madar, H. et al. Surgical management of postpartum haemorrhage: survey of French obstetricians. Sci Rep 6, 30342 (2016). https://doi.org/10.1038/srep30342
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep30342
This article is cited by
-
Surgical treatment of postpartum haemorrhage: national survey of French residents of obstetrics and gynecology
BMC Pregnancy and Childbirth (2019)