Abstract
Prognostic scores, such as the PRISM and APACHE II, have been established, predicting with reasonable accuracy the outcome of patients admitted to intensive care units (ICU). In keeping with previous reports, we found, however, that these scores failed to perform in a series of 28 recipients of hematopoietic auto- or allografts (BMT) who required ICU admission for reasons including respiratory (82%) and multi-organ (36%) failure. We therefore retrospectively analyzed the charts of these patients, evaluating predisposing factors and prognostic variables which might confound the validity of these ICU tools which in other clinical scenarios have proven so valuable. Of all the parameters tested, logistic analysis established the following as predictors for poor outcome: increased C-reactive protein (CRP) to >10 mg/dl (P = 0.04), macroscopic hemorrhage (P = 0.04), hypotension (mean arterial pressure < normal) (P = 0.04) and GVHD ⩾ III (P = 0.002). Most of these factors are not accounted for by the standard prognostic questionnaires. The development of an ‘oncological’ or ‘post-BMT’ risk of mortality score, taking into account these patients’ specific clinical problems, might improve the risk assessment for this patient group, and might thus facilitate the timely recognition of those patients most in need of more intensive therapeutic measures. Bone Marrow Transplantation (2000) 25 , Suppl. 2, S32–S34.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Bönig, H., Schneider, D., Sprock, I. et al. ‘Sepsis’ and multi-organ failure: predictors of poor outcome after hematopoietic stem cell transplantation in children. Bone Marrow Transplant 25 (Suppl 2), S32–S34 (2000). https://doi.org/10.1038/sj.bmt.1702350
Published:
Issue date:
DOI: https://doi.org/10.1038/sj.bmt.1702350
Keywords
This article is cited by
-
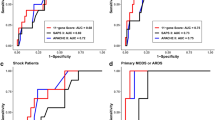
Net reclassification improvement with serial biomarkers and bed-sided spirometry to early predict the need of organ support during the early post-transplantation in-hospital stay in allogeneic HCT recipients
Bone Marrow Transplantation (2019)
-
Hospital charges and length of stay associated with septicemia among children hospitalized for leukemia treatment in the United States
World Journal of Pediatrics (2012)
-
Prognostic value of T-1 cell numbers prior to allogeneic stem cell transplantation in patients with severe graft-versus-host disease
Bone Marrow Transplantation (2005)
-
Prognostic value of C-reactive protein and cytokine assays for transplant-related mortality
Bone Marrow Transplantation (2004)
-
Serial evaluation of the oncological pediatric risk of mortality (O-PRISM) score following allogeneic bone marrow transplantation in children
Bone Marrow Transplantation (2002)