Summary:
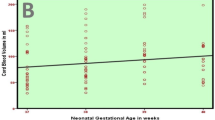
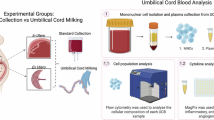
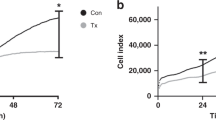
The use of cord blood (CB) for transplantation has increased greatly in recent years. The collection strategy is the first step in collecting good-quality CB units. There are two main techniques for collecting CB from the umbilical vein: in the delivery room while the placenta is still in the uterus by midwives and obstetricians or in an adjacent room after placental delivery by CB bank trained personnel. In this study, the benefits and disadvantages between the two different CB collection strategies were evaluated, in order to improve CB bank methodology. Valencia CB bank maintains the two different collection strategies. CB was obtained from 569 vaginal and 70 caesarean deliveries and obstetrical and clinical charts were reviewed. Before processing CB units, volume was calculated and samples were drawn for cell counts. After processing and before cryopreservation samples were drawn for cell counts, CD34+cell analysis, viability, clonogenic assays and microbiology were drawn directly from the bags. We compared the efficiency of the two collection techniques. Obstetric data and umbilical CB were obtained from 569 vaginal (264 collected in utero and 305 collected ex utero) and 70 caesarean deliveries. The proportion of excluded CB units before processing was 33% for vaginal ex utero, 25% for vaginal in utero and 46% for caesarean deliveries. Differences were statistically significant. For vaginal deliveries a larger volume and a higher number of nucleated cells, percentage of CD34+ cells and colony-forming units (CFUs) were harvested in the in utero collection group. There was no statistical difference between CB collected after placental expulsion from vaginal and caesarean deliveries. Comparison between all vaginal and caesarean deliveries did not show any difference.
We conclude that the mode of collection influences the haematopoietic content of CB donations. Collection before placental delivery is the best approach to CB collection and allows optimisation of CB bank methodology. Caesarean deliveries seem to contain similar progenitor content to vaginal deliveries.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Gluckman E, Broxmeyer HE, Auerbach AD et al. Haematopoietic reconstitution in a patient with Fanconi's anemia by means of umbilical-cord blood from an HLA-identical sibling. N Engl J Med 1989; 321: 1174–1178.
Gluckman E . Current status of umbilical cord blood haematopoietic stem cell transplantation. Exp Hematol 2000; 28: 1197–1205.
Stanworth S, Warwick R, Fehily D et al. An international survey of unrelated umbilical cord blood banking. Vox Sang 2001; 80: 236–243.
Gluckman E . Cellular characteristics of cord blood and cord blood transplantation. In Broxmeyer HE (ed). Cord Blood Banking and Transplantation in Europe. AABB Press: Bethesda, 1998, pp 147–164.
Elchalal U, Fasouliotis SJ, Shtockheim D et al. Postpartum umbilical cord blood collection for transplantation: a comparison of three methods. Am J Obstet Gynecol 2000; 182: 227–232.
Rubinstein P, Taylor PE, Scaradavou A et al. Unrelated placental blood for bone marrow reconstitution: organization of the placental blood program. Blood Cells 1994; 20: 587–596.
Jefferies LC, Albertus M, Morgan MA, Moolten D . High deferral rate for maternal–neonatal donor pairs for an allogeneic umbilical cord blood bank. Transfusion 1999; 40: 122–123.
Donaldson C, Armitage WJ, Laundy V et al. Impact of obstetric factors on cord blood donation for transplantation. Br J Haematol 1999; 106: 128–132.
Ballen KK, Wilson M, Wuu J et al. Bigger is better: maternal and neonatal predictors of haematopoietic potential of umbilical cord blood units. Bone Marrow Transplant 2001; 27: 7–14.
Lim FTH, Scherjon SA, van Beckhoven JM et al. Association of stress during delivery with increased numbers of nucleated cells and haematopoietic progenitor cells in umbilical cord blood. Am J Obstet Gynecol 2000; 183: 1144–1151.
Surbek DV, Aufderhaar U, Holzgreve W . Umbilical cord blood collection for transplantation: which technique should be preferred? Am J Obstet Gynecol 2000; 183: 1587–1588.
Surbek DV, Schonfeld B, Tichelli A et al. Optimizing cord blood mononuclear cell yield: a randomized comparison of collection before vs after placenta delivery. Bone Marrow Transplant 1998; 22: 311–312.
Wong A, Yuen PM, Li K et al. Cord blood collection before and after placental delivery: levels of nucleated cells, haematopoietic progenitor cells, leukocyte subpopulations and macroscopic clots. Bone Marrow Transplant 2001; 27: 133–138.
Lim F, Beckhoven J, Brand A et al. The number of nucleated cells reflects the haematopoietic content of umbilical cord blood for transplantation. Bone Marrow Transplant 1999; 24: 965–970.
Surbek DV, Visca E, Steinmann C et al. Umbilical cord blood collection before placental delivery during cesarean delivery increases cord blood volume and nucleated cell number available for transplantation. Am J Obstet Gynecol 2000; 183: 218–221.
Sparrow RL, Cauchi JA, Ramadi LT et al. Influence of mode of birth and collection on WBC yields of umbilical cord blood units. Transfusion 2002; 42: 210–215.
Yamada T, Okamoto Y, Kasamatu H et al. Factors affecting the volume of umbilical cord blood collections. Acta Obstet Gynecol Scand 2000; 79: 830–833.
Grisaru D, Deutsch V, Pick M . Placing the newborn on the maternal abdomen after delivery increases the volume and CD34 cell content in the umbilical CB collected: an old maneuver with new applications. Am J Obstet Gynecol 1999; 180: 1240–1243.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Solves, P., Moraga, R., Saucedo, E. et al. Comparison between two strategies for umbilical cord blood collection. Bone Marrow Transplant 31, 269–273 (2003). https://doi.org/10.1038/sj.bmt.1703809
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/sj.bmt.1703809
Keywords
This article is cited by
-
Factors associated with blood cord unit bankability: an analysis of a 15-year-long case series
Cell and Tissue Banking (2020)
-
Association of cord blood platelet count and volume with hemoglobin in healthy term infants
Journal of Perinatology (2011)