Abstract
Purpose
To determine the incidence of glaucomatous progression at mean intraocular pressure (IOP) levels in patients with ocular hypertension (OHT).
Methods
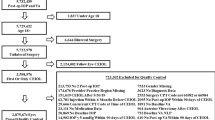
A retrospective, multicentre, cohort analysis of 230 OHT patients with 5 years of follow-up evaluated for risk factors associated with progressive optic disc and visual field loss to determine the incidence of glaucomatous progression.
Results
Forty percent of patients with IOPs ⩾24 mmHg, 18% of patients with IOPs of 21–23 mmHg, 11% of patients with IOPs with 18–20 mmHg, and 3% of patients with IOPs of ⩽17 mmHg progressed to glaucoma. The mean IOP was 19.8±2.4 mmHg in the stable group and 21.7±2.6 mmHg in the progressed group (P=0.0004). The highest average peak IOP was 23.4±4.0 mmHg in the stable group and 25.2±3.1 mmHg in the progressed group (P=0.006). Based on the pachymetry values for central corneal thickness, patients with thinner corneas more often progressed to glaucoma (P<0.0001). A multivariant regression analysis to determine risk factors for progression was positive primarily for higher peak IOPs, older age, male gender, argon laser trabeculoplasty, visual acuity ⩾20/50, and no topical medical therapy or β-blocker therapy prior to the study.
Conclusions
IOP reduction within the normal range over 5 years of follow-up reduces the chance of progression to primary open-angle glaucoma in OHT patients.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Brandt JD, Beiser JA, Kass MA, Gordon MO . Central corneal thickness in the ocular hypertension treatment study (OHTS). Ophthalmology 2001; 108: 1779–1788.
Book SA . Essentials of Statistics. McGraw-Hill Book Company:New York, 1978; 122: 205.
Stewart WC, Chorak RP, Hunt HH, Sethuraman G . Factors associated with visual loss in patients with advanced glaucomatous changes in the optic nerve head. Am J Ophthalmol 1993; 116: 176–181.
Stewart WC, Kolker AE, Sharpe ED, Day DG, Holmes KT, Leech JN et al. Factors associated with long-term progression or stability in primary open-angle glaucoma. Am J Ophthalmol 2000; 130: 274–279.
Konstas AGP, Hollo G, Astakhov YS, Teus MA, Akopov EL, Jenkins JN et al. Factors associated with long-term progression or stability in exfoliation glaucoma. Arch Ophthalmol 2004; 122: 29–33.
The AGIS Investigators. The advanced glaucoma intervention study (AGIS):7. The relationship between control of intraocular pressure and visual field deterioration. Am J Ophthalmol 2000; 130: 429–440.
Quigley HA, Maumenee AE . Long-term follow-up of treated open-angle glaucoma. Am J Ophthalmol 1979; 87: 519–525.
Kolker AE . Visual prognosis in advanced glaucoma: a comparison of medical and surgical therapy for retention of vision in 101 eyes with advanced glaucoma. Trans Am Ophthalmol Soc 1977; 75: 539.
Odberg T . Visual field prognosis in advanced glaucoma. Acta Ophthalmol 1987; 65: 27–29.
Schulzer M, Mikelberg FS, Drance SM . Some observations on the relation between intraocular pressure reduction and the progression of glaucomatous visual loss. Br J Ophthalmol 1987; 71: 486–488.
Grant WM, Burke JF . Why do some people go blind from glaucoma? Ophthalmology 1982; 89: 991–998.
Stewart WC, Sine CS, Lo Presto C . Surgical vs medical management of chronic open-angle glaucoma. Am J Ophthalmol 1996; 122: 767–774.
Mao LK, Stewart WC, Shields MB . Correlation between intraocular pressure control and progressive glaucomatous damage in primary open-angle glaucoma. Am J Ophthalmol 1991; 111: 51–55.
Herndon LW, Weizer JS, Stinnett SS . Central corneal thickness as a risk factor for advanced glaucoma damage. Arch Ophthalmol 2004; 122: 17–21.
Medeiros FA, Sample PA, Zangwill LM, Bowd C, Aihara M, Weinreb RN . Corneal thickness as a risk factor for visual field loss in patients with preperimetric glaucomatous optic neuropathy. Am J Ophthalmol 2003; 136: 805–813.
Stewart WC, Day DG, Jenkins JN, Passmore CL, Stewart JA . Mean intraocular pressure and progression based on corneal thickness in primary open-angle glaucoma. J Ocul Pharmacol Ther 2006; 22: 26–33.
Stewart WC, Jenkins JN, Stewart JA . Changes of intraocular pressure measurements and central corneal thickness following refractive surgery. Ophthalmology 2005; 112: 1637.
Hedman K, Watson PG, Alm A . The effect of latanoprost on intraocular pressure during 2 years of treatment. Surv Ophthalmol 2002; 47(Suppl 1): S65–S76.
Acknowledgements
This study was not supported by any public or private funding agency.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Konstas, A., Irkec, M., Teus, M. et al. Mean intraocular pressure and progression based on corneal thickness in patients with ocular hypertension. Eye 23, 73–78 (2009). https://doi.org/10.1038/sj.eye.6702995
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/sj.eye.6702995
Keywords
This article is cited by
-
Aqueous humor cytokine levels are associated with the severity of visual field defects in patients with primary open-angle glaucoma
BMC Ophthalmology (2023)
-
Thinner retinal nerve fibre layer in healthy myopic eyes with thinner central corneal thickness
Graefe's Archive for Clinical and Experimental Ophthalmology (2020)
-
Short-term reproducibility of intraocular pressure and ocular perfusion pressure measurements in Chinese volunteers and glaucoma patients
BMC Ophthalmology (2016)