Abstract
Aim:
To evaluate the clinical impact of reduced heparin responsiveness (HRreduced) on the incidence of myocardial infarction (MI) following off-pump coronary artery bypass graft surgery (OPCAB), and to identify the predictors of HRreduced.
Methods:
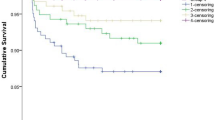
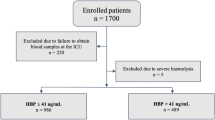
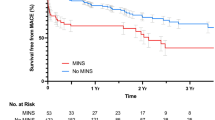
A total of 199 patients scheduled for elective OPCAB were prospectively enrolled. During anastomosis, 150 U/kg of heparin was injected to achieve an activated clotting time (ACT) of ≥300 s, and the heparin sensitivity index (HSI) was calculated. HSIs below 1.0 were considered reduced (HRreduced). The relationships between the HSI and postoperative MI, cardiac enzyme levels and preoperative risk factors of HRreduced were investigated.
Results:
There was no significant relationship between the HSI and cardiac enzyme levels after OPCAB. The incidence of MI after OPCAB was not higher in HRreduced patients. HRreduced occurred more frequently in patients with low plasma albumin concentrations and high platelet counts.
Conclusion:
HRreduced was not associated with adverse ischemic outcomes during the perioperative period in OPCAB patients, which seemed to be attributable to a tight prospective protocol for obtaining a target ACT regardless of the presence of HRreduced.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Avidan MS, Levy JH, van Aken H, Feneck RO, Latimer RD, Ott E, et al. Recombinant human antithrombin III restores heparin responsiveness and decreases activation of coagulation in heparin-resistant patients during cardiopulmonary bypass. J Thorac Cardiovasc Surg 2005; 130: 107–13.
Karmanoukian H, Attuwabi B, Nader ND . Antithrombotic controversies in off-pump coronary bypass. Semin Thorac Cardiovasc Surg 2005; 17: 59–65.
Levy JH . Heparin resistance and antithrombin: should it still be called heparin resistance? J Cardiothorac Vasc Anesth 2004; 18: 129–30.
Cloyd GM, D'Ambra MN, Akins CW . Diminished anticoagulant response to heparin in patients undergoing coronary artery bypass grafting. J Thorac Cardiovasc Surg 1987; 94: 535–8.
Staples MH, Dunton RF, Karlson KJ, Leonardi HK, Berger RL . Heparin resistance after preoperative heparin therapy or intraaortic balloon pumping. Ann Thorac Surg 1994; 57: 1211–6.
Kaku B, Katsuda S, Taguchi T, Nitta Y, Hiraiwa Y . A case of acute myocardial infarction with repetitive stent thrombosis during emergent percutaneous coronary intervention. Transient decrease in antithrombin III activity and heparin resistance. Int Heart J 2009; 50: 111–9.
Ferguson JJ, Dougherty KG, Gaos CM, Bush HS, Marsh KC, Leachman DR . Relation between procedural activated coagulation time and outcome after percutaneous transluminal coronary angioplasty. J Am Coll Cardiol 1994; 23: 1061–5.
Narins CR, Hillegass WB Jr, Nelson CL, Tcheng JE, Harrington RA, Phillips HR, et al. Relation between activated clotting time during angioplasty and abrupt closure. Circulation 1996; 93: 667–71.
Brener SJ, Moliterno DJ, Lincoff AM, Steinhubl SR, Wolski KE, Topol EJ . Relationship between activated clotting time and ischemic or hemorrhagic complications: analysis of 4 recent randomized clinical trials of percutaneous coronary intervention. Circulation 2004; 110: 994–8.
Tolleson TR, O'Shea JC, Bittl JA, Hillegass WB, Williams KA, Levine G, et al. Relationship between heparin anticoagulation and clinical outcomes in coronary stent intervention: observations from the ESPRIT trial. J Am Coll Cardiol 2003; 41: 386–93.
Ranucci M, Frigiola A, Menicanti L, Cazzaniga A, Soro G, Isgro G . Risk factors for fatal myocardial infarction after coronary bypass graft surgery. Eur J Anaesthesiol 2001; 18: 322–9.
Chan T, Hwang NC, Lim CH . A statistical analysis of factors predisposing patients to heparin resistance. Perfusion 2006; 21: 99–103.
Moller CH, Steinbruchel DA . Platelet function after coronary artery bypass grafting: is there a procoagulant activity after off-pump compared with on-pump surgery? Scand Cardiovasc J 2003; 37: 149–53.
Mariani MA, Gu YJ, Boonstra PW, Grandjean JG, van Oeveren W, Ebels T . Procoagulant activity after off-pump coronary operation: is the current anticoagulation adequate? Ann Thorac Surg 1999; 67: 1370–5.
Englberger L, Streich M, Tevaearai H, Carrel TP . Different anticoagulation strategies in off-pump coronary artery bypass operations: a European survey. Interact Cardiovasc Thorac Surg 2008; 7: 378–82.
Ranucci M, Isgro G, Cazzaniga A, Ditta A, Boncilli A, Cotza M, et al. Different patterns of heparin resistance: therapeutic implications. Perfusion 2002; 17: 199–204.
French JK, White HD . Clinical implications of the new definition of myocardial infarction. Heart 2004; 90: 99–106.
Shroyer AL, Coombs LP, Peterson ED, Eiken MC, DeLong ER, Chen A, et al. The Society of Thoracic Surgeons: 30-day operative mortality and morbidity risk models. Ann Thorac Surg 2003; 75: 1856–64; discussion 1864–5.
Keeley EC, Velez CA, O'Neill WW, Safian RD . Long-term clinical outcome and predictors of major adverse cardiac events after percutaneous interventions on saphenous vein grafts. J Am Coll Cardiol 2001; 38: 659–65.
Avidan MS, Levy JH, Scholz J, Delphin E, Rosseel PM, Howie MB, et al. A phase III, double-blind, placebo-controlled, multicenter study on the efficacy of recombinant human antithrombin in heparin-resistant patients scheduled to undergo cardiac surgery necessitating cardiopulmonary bypass. Anesthesiology 2005; 102: 276–84.
Choi YS, Shim JK, Hong SW, Kim DH, Kim JC, Kwak YL . Risk factors of atrial fibrillation following off-pump coronary artery bypass graft surgery: predictive value of C-reactive protein and transfusion requirement. Eur J Cardiothorac Surg 2009; 36: 838–43.
Tanaka KA, Thourani VH, Williams WH, Duke PG, Levy JH, Guyton RA, et al. Heparin anticoagulation in patients undergoing off-pump and on-pump coronary bypass surgery. J Anesth 2007; 21: 297–303.
Bittl JA, Ahmed WH . Relation between abrupt vessel closure and the anticoagulant response to heparin or bivalirudin during coronary angioplasty. Am J Cardiol 1998; 82: 50P–56P.
Hansen KH, Hughes P, Steinbruchel DA . Antithrombotic- and anticoagulation regimens in OPCAB surgery. A Nordic survey. Scand Cardiovasc J 2005; 39: 369–74.
Raivio P, Kuitunen A, Suojaranta-Ylinen R, Lassila R, Petaja J . Thrombin generation during reperfusion after coronary artery bypass surgery associates with postoperative myocardial damage. J Thromb Haemost 2006; 4: 1523–9.
Na S, Shim JK, Chun DH, Kim DH, Hong SW, Kwak YL . Stabilized infective endocarditis and altered heparin responsiveness during cardiopulmonary bypass. World J Surg 2009; 33: 1862–7.
Lemmer JH Jr, Despotis GJ . Antithrombin III concentrate to treat heparin resistance in patients undergoing cardiac surgery. J Thorac Cardiovasc Surg 2002; 123: 213–7.
Matthai WH Jr, Kurnik PB, Groh WC, Untereker WJ, Siegel JE . Antithrombin activity during the period of percutaneous coronary revascularization: relation to heparin use, thrombotic complications and restenosis. J Am Coll Cardiol 1999; 33: 1248–56.
Loubser PG, McCarthy JJ, Attar M . Coronary thrombosis associated with antithrombin-III deficiency. J Cardiothorac Vasc Anesth 1997; 11: 756–9.
Hashimoto K, Yamagishi M, Sasaki T, Nakano M, Kurosawa H . Heparin and antithrombin III levels during cardiopulmonary bypass: correlation with subclinical plasma coagulation. Ann Thorac Surg 1994; 58: 799–804; discussion 804–5.
Sindermann JR, March KL . Heparin responsiveness in vitro as a prognostic tool for vascular graft stenosis: a tale of two cell types? Circulation 1998; 97: 2486–90.
Refson JS, Schachter M, Patel MK, Hughes AD, Munro E, Chan P, et al. Vein graft stenosis and the heparin responsiveness of human vascular smooth muscle cells. Circulation 1998; 97: 2506–10.
Patti G, Nusca A, Mangiacapra F, Gatto L, D'Ambrosio A, Di Sciascio G . Point-of-care measurement of clopidogrel responsiveness predicts clinical outcome in patients undergoing percutaneous coronary intervention results of the ARMYDA-PRO (Antiplatelet therapy for Reduction of MYocardial Damage during Angioplasty-Platelet Reactivity Predicts Outcome) study. J Am Coll Cardiol 2008; 52: 1128–33.
Acknowledgements
This study was supported by a faculty research grant (6-2008-0187) of Yonsei University College of Medicine of 2008.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chun, Dh., Baik, Sw., Kim, S. et al. Heparin responsiveness during off-pump coronary artery bypass graft surgery: predictors and clinical implications. Acta Pharmacol Sin 32, 133–138 (2011). https://doi.org/10.1038/aps.2010.180
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/aps.2010.180