Abstract
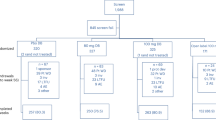
Hepatic parenchymal vasoconstriction increases cytotoxic drug uptake into hepatic metastases by increasing the tumour to liver blood flow ratio. Prolonged infusion of the vasoconstrictor vasopressin does not result in sustained vasoconstriction, and this may limit the benefit of vasopressin in infusional chemotherapy. We have assessed whether loss of vasopressin-induced vasoconstriction is mediated by nitric oxide. Hepatic and tumour blood flow were continuously monitored, in an animal hepatic tumour model, by laser Doppler flowmetry. The response to regionally infused vasopressin and the nitric oxide inhibitor N-nitro-L-arginine methyl ester (L-NAME) were assessed over a 30 min infusion period. The vasopressin-induced vasoconstrictor effect diminished after 15 min despite continued infusion. Vasoconstriction was significantly prolonged when L-NAME was infused in addition to vasopressin. The increase in tumour to normal blood flow ratio was greater over the infusion period when L-NAME was co-administered with vasopressin. Our results suggest that the loss of vasopressin-induced vasoconstriction seen in liver parenchyma after regional infusion is prevented by the nitric oxide synthase inhibitor L-name and may be mediated by nitric oxide.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Dworkin, M., Carnochan, P. & Allen-Mersh, T. Nitric oxide inhibition sustains vasopressin-induced vasoconstriction. Br J Cancer 71, 942–944 (1995). https://doi.org/10.1038/bjc.1995.182
Issue date:
DOI: https://doi.org/10.1038/bjc.1995.182
This article is cited by
-
Discovery of novel selective hypotensive vasopressin peptides that exhibit little or no functional interactions with known oxytocin/vasopressin receptors
British Journal of Pharmacology (1998)