Abstract
Purpose To perform a pilot study on the prevalence of familial thrombophilia in all cases of retinal vein occlusion with no known risk factors.
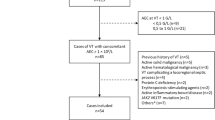
Methods Over the 1 year study period 71 patients presented with a new diagnosis of retinal vein occlusion (age 28-90 years). Fifty-five (77%) were excluded because of local predisposing factors. The remaining 16 (23%) had a full risk factor history taken and blood investigations of rheological factors and thrombophilia including tests for the factor V Leiden mutation, prothrombin G20210A allele and hyperhomocysteinaemia.
Results Of those with no local predisposing factors, 3 patients had antiphospholipid antibodies, 3 had raised fibrinogen levels, 4 had hyperhomocysteinaemia and 1 was heterozygous for the Leiden mutation. Other lifestyle risk factors such as obesity, smoking and a positive family history of venous thrombosis were not uncommon. No patient had the prothrombin G20210A variant.
Conclusions It seems likely that several risk factors, both genetic and acquired, need to be present for thrombosis to occur. In investigating a new patient with a retinal vein occlusion one should test for hypertension, glaucoma and diabetes mellitus. Estimation of plasma viscosity and a full blood count are cheap investigations which may reveal neoplasia or vasculitis, and lipid levels should be estimated. In a young patient or one with an unexpected vein occlusion and a personal or family history of thrombosis, a hypercoagulable state may rarely be identified. This additional testing should include testing for antiphospholipid antibodies and a full thrombophilia screen including the factor V Leiden mutation, homocysteine and the prothrombin variant as part of a clinical trial. Until the role of these markers in thrombosis is better defined in relation to causation of retinal vein occlusion and treatment has been shown to improve outcome, we can not recommend them for routine testing. If a hereditary defect is found, referral should be made to a haematologist and consideration given to anticoagulation and screening of family members to prevent further thrombotic episodes. Retinal vein occlusions are multifactorial in origin except in rare cases.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
The Eye Disease Case-Control Study Group. Risk factors for branch retinal vein occlusion. Am J Ophthalmol 1993;116:286–96.
The Eye Disease Case-Control Study Group. Risk factors for central retinal vein occlusion. Arch Ophthalmol 1996;114:545–54.
The Eye Disease Case-Control Study Group. Risk factors for hemiretinal vein occlusion: comparison with risk factors for central and branch retinal vein occlusion. Ophthalmology 1998;105:765–71.
Rath EZ, Frank RN, Shin DH, et al. Risk factors for retinal vein occlusions: a case-control study. Ophthalmology 1992;99:509–14.
Appiah AP, Trempe CL . Risk factors associated with branch vs central retinal vein occlusion. Ann Ophthalmol 1989;21:153–7.
Glacet-Bernard A, Chabanel A, Lelong F, et al. Elevated erythrocyte aggregation in patients with CRVO with and without conventional risk factors. Ophthalmology 1994;101:1483–7.
Arend O, Remky A, Jung F, et al. Role of rheologic factors in patients with acute central retinal vein occlusion. Ophthalmology 1996;103:80–6.
Bandello F, Vigano D'Angelo S, Parlavecchia M, et al. Hypercoagulability and high lipoprotein (a) levels in patients with central retinal vein occlusion. Thromb Haemost 1994;72:39–43.
Larsson J, Olafsdottir E, Bauer B . Activated protein C resistance in young adults with central retinal vein occlusion. Br J Ophthalmol 1996;80:200–2.
Kumar B, Yu D, Morgan W, et al. The distribution of angioarchitectural changes within the vicinity of the arteriovenous crossing in branch retinal vein occlusion. Ophthalmology 1998;105:424–7.
Larsson J, Sellman A, Bauer B . Activated protein C resistance in patients with central retinal vein occlusion. Br J Ophthalmol 1997;81:832–4.
Zoller B, Svensson PJ, He X, et al. Identification of the same factor V gene mutation in 47 out of 50 thrombosis-prone families with inherited resistance to activated protein C. J Clin Invest 1994;94:2521–4.
Graham SL, Goldberg I, Murray B, et al. Activated protein C resistance: low incidence in glaucomatous optic disc haemorrhage and central retinal vein occlusion. Aust NZ J Ophthalmol 1996;24:199–205.
Hodgkins PR, Perry DJ, Sawcer SJ, et al. Factor V and antithrombin gene mutations in patients with idiopathic central retinal vein occlusion. Eye 1995;9:760–2.
Raguenes O, Mercier B, Escoffre M, et al. 1691 G to A mutation of the factor V gene: no association with thrombosis of the central retinal vein. Presse Med 1996;25:460.
Linna T, Ylikorkala A, Kontula K, et al. Prevalence of factor V Leiden in young adults with retinal vein occlusion. Thromb Haemost 1997;77:214–5.
Gottlieb JL, Blice JP, Mestichelli B . Activated protein C resistance, factor V Leiden and central retinal vein occlusion in young adults. Arch Ophthalmol 1998;116:577–9.
Bertina RM, Koeleman BP, Koster T, et al. Mutation in blood coagulation factor V associated with resistance to activated protein C. Nature 1994;369:64–7.
Bowen DJ, Bowley S, John M, et al. al. Wales population of the UK. Thromb Haemost 1998;79:949–54.
Cox MJ, Rees DC, Martinson JJ, et al. Evidence for a single origin of factor V Leiden. Br J Haematol 1996;92:1022–5.
Rees DC, Cox M, Clegg JB . World distribution of factor V Leiden. Lancet 1995;346:1133–4.
Vandenbroucke JP, Koster T, Briet E, et al. Increased risk of venous thrombosis in oral contraceptive users who are carriers of factor V Leiden mutation. Lancet 1994;344:1453–7.
Baglin C, Brown K, Luddington R, et al. Risk of recurrent venous thromboembolism in patients with the factor V Leiden (FVR506Q) mutation: effect of warfarin and prediction by precipitating factors. Br J Haematol 1998;100:764–8.
Clark P, Brennand J, Conkie JA, et al. Activated protein C sensitivity, protein C, Protein S and coagulation in normal pregnancy. Thromb Haemost 1998;79:1166–70.
Rosendaal FR, Doggen CJ, Zivelin A, et al. Geographic distribution of the 20210G to A prothrombin variant. Thromb Haemost 1998;79:706–8.
Poort SR, Rosendaal FR, Reitsma PH, et al. A common genetic variation in the 3'-untranslated region of the prothrombin gene is associated with elevated plasma prothrombin levels and an increase in venous thrombosis. Blood 1996;88:3698–703.
Hillarp A, Zoller B, Svensson PJ, et al. The 20210A allele of the prothrombin gene is a common risk factor among Swedish outpatients with verified deep venous thrombosis. Thromb Haemost 1997;78:990–2.
Longstreth WT, Rosendaal FR, Siscovick DS, et al. Risk of stroke in young women and two prothrombotic mutations: factor V Leiden and prothrombin gene variant (G20210A). Stroke 1998;29:577–80.
McCully KS . Homocysteine and vascular disease. Nature Med 1996;2:386–9.
Wenzler EM, Rademakers AJ, Boers GH, et al. Hyperhomocysteinaemia in retinal artery and retinal vein occlusion. Am J Ophthalmol 1993;115:162–7.
Biousse V, Newman NJ, Sternberg P . Retinal vein occlusion and transient monocular visual loss associated with hyperhomocystinemia. Am J Ophthalmol 1997;124:257–60.
Stein JH, McBride PE . Hyperhomocysteinemia and atherosclerotic vascular disease. Arch Intern Med 1998;158:1301–6.
Mayer EL, Jacobsen DW, Robinson K . Homocysteine and coronary atherosclerosis. J Am Coll Cardiol 1996;27:517–27.
Rees MM, Rodgers GM . Homocysteinemia: association of a metabolic disorder with vascular disease and thrombosis. Thromb Res 1993;71:337–59.
Homocysteine Lowering Trialists' Collaboration. Lowering blood homocysteine with folic acid based supplements: meta-analysis of randomised trials. BMJ 1998;316:894–8.
Peterson JC, Spense JD . Vitamins and progression of atherosclerosis in hyperhomocysteinaemia. Lancet 1998;351:263.
Graham IM, Daly LE, Refsum HM, et al. Plasma homocysteine as a risk factor for vascular disease. JAMA 1997;277:1775–81.
Still RA, McDowell IF . Clinical implications of plasma homocysteine measurements in cardiovascular disease. J Clin Pathol 1998;51:183–8.
Asherson RA, Khamashta MA, Ordi-Ros J, et al. The ‘primary’ antiphospholipid syndrome: major clinical and serological features. Medicine 1989;68:366–74.
Vila P, Hernandez MC, Lopez-Fernandez MF, et al. Prevalence, follow-up and clinical significance of the anticardolipin antibodies in normal subjects. Thromb Haemost 1994;72:209–13.
Rosove MH, Brewer PM . Antiphospholipid thrombosis: clinical course after the first thrombotic event in 70 patients. Ann Intern Med 1992;117:303–8.
Boumpas DT, Fessler BJ, Austin HA, et al. Systemic lupus erythematosus: emerging concepts. 2. Dermatologic and joint disease, the antiphospholipid antibody syndrome, pregnancy and hormonal therapy, morbidity and mortality and pathogenesis. Ann Intern Med 1995;123:42–53.
Ames PR, Tommasino C, E'Andrea G, et al. Thrombophilic genotypes in subjects with idiopathic antiphospholipid antibodies: prevalence and significance. Thromb Haemost 1998;79:46–9.
Khamashta MA, Cuadrado MJ, Mujic F, et al. The management of thrombosis in the antiphospholipid syndrome. N Engl J Med 1995;332:993–7.
Guareschi G, Vigano D'Angelo S, Foresti V . Normal activities of protein C protein S and antithrombin III in young patients with retinal vein occlusion. Haematologica 1990;75:483–4.
Chung MM, Trese MT, Hong YJ . Protein C levels in retinal vein occlusions. Invest Ophthalmol Vis Sci 1989;30:477.
Rosendaal FR . Thrombosis in the young: epidemiology and risk factors. A focus on venous thrombosis. Thromb Haemost 1997;78:1–6.
Author information
Authors and Affiliations
Additional information
Presented at the Royal College of Ophthalmologists Annual Congress, Cardiff 1999
Rights and permissions
About this article
Cite this article
Backhouse, O., Parapia, L., Mahomed, I. et al. Familial thrombophilia and retinal vein occlusion. Eye 14, 13–17 (2000). https://doi.org/10.1038/eye.2000.4
Received:
Accepted:
Issue date:
DOI: https://doi.org/10.1038/eye.2000.4
Keywords
This article is cited by
-
Venous thromboembolism does not share familial susceptibility with retinal vascular occlusion or glaucoma: a nationwide family study
Journal of Thrombosis and Thrombolysis (2016)
-
Central retinal vein occlusion and thrombophilia
Eye (2002)