Abstract
Purpose
To investigate whether interleukine-8 (IL-8) and monocyte chemoattractant protein-1 (MCP-1) are related with macular oedema in patients with branch retinal vein occlusions (BRVOs).
Design
Retrospective case–control study.
Participants
Nineteen patients who had macular oedema due to BRVO and nine patients with non-ischaemic ocular diseases (control group).
Methods
Macular oedema was examined by optical coherence tomography. Both venous blood and vitreous samples were obtained at the time of vitreoretinal surgery. IL-8 and MCP-1 levels in vitreous fluid and plasma were determined with enzyme-linked immunosorbent assay kits. Variables were compared with the Mann–Whitney U-test, Wilcoxon's signed-ranked test, and the χ2-test, when appropriate. To examine correlations, Spearman's rank-order correlation coefficients were calculated. Statistical significance was set at P<0.05.
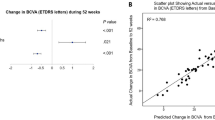
Results
The vitreous fluid levels of IL-8 (median: 63.5 pg/ml) and MCP-1 (median: 1522.4 pg/ml) were significantly higher in the patients with BRVO than in the control group (median: 5.1 and 746.5 pg/ml respectively; P<0.001 and <0.001 respectively). Vitreous IL-8 and MCP-1 were significantly correlated in patients with BRVO (P=0.009).
Conclusions
Both IL-8 and MCP-1 were elevated in the vitreous fluid of patients with BRVO and macular oedema. Both chemokines may contribute to the pathogenesis of macular oedema in patients with BRVO.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Ryan SJ . Retina. 3rd Vol, 3rd ed. Mosby: St Louis, 2001.
Vinores SA, Derevjanik NL, Ozaki H, Okamoto N, Campochiaro PA . Cellular mechanisms of blood–retinal barrier dysfunction in macular edema. Doc Ophthalmol 1999; 97: 217–228.
Gardner TW, Antonetti DA, Barber AJ, Lieth E, Tarbell JA, Penn State Retina Research Group. The molecular structure and function of the blood–retina barrier. Doc Ophthalmol 1999; 97: 229–237.
Maruo N, Morita I, Shirao M, Murota S . IL-6 increases endothelial permeability in vitro. Endocrinology 1992; 131: 710–714.
Noma H, Minamoto A, Funatsu H, Tsukamoto H, Nakano K, Yamashita H et al. Intravitreal levels of vascular endothelial growth factor and interleukine-6 are correlated with macular edema in branch retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol 2006; 244: 309–315.
Noma H, Funatsu H, Mimura T, Harino S, Hori S . Vitreous levels of interleukine-6 and vascular endothelial growth factor in macular edema with central retinal vein occlusion. Ophthalmology 2009; 116: 87–93.
Theoharides TC, Rozmieki JJ, Sahagian G, Jocobson S, Kempuraj D, Conti P et al. Impact of stress and mast cells on brain metastases. J Neuroimmunol 2008; 205: 1–7.
Veldhuis WB, Floris S, van der Meide PH, Vos IM, de Vries HE, Dijkstra CD et al. Interferon-beta prevents cytokine neutrophil infiltration and attenuates blood–brain barrier disruption. J Cereb Flow Metab 2003; 23: 1060–1069.
Stamatovic SM, Shakui P, Keep RF, Moore BB, Kunkel SL, Van Rooijen N et al. Monocyte chemoattractant protein-1 regulation of blood–brain barrier permeability. J Cereb Blood Flow Metab 2005; 25: 593–606.
Crane IJ, Wallace CA, MCkillop-Smith S, Forrester JV . Control of chemokine production at the blood–retina barrier. Immunology 2000; 101: 426–433.
The Branch Vein Occlusion Study Group. Argon laser photocoagulation for macular edema in branch vein occlusion. Am J Ophthalmol 1984; 98: 271–282.
Hara A, Nagatomo M . Branch retinal vein occlusion decreases the potential of the inner retinal layer. Nippon Ika Daigaku Zasshi 1995; 62: 50–54.
The Branch Vein Occlusion Study Group. Argon laser scatter photocoagulation for prevention of retinal neovascularization and vitreus haemorrhage in branch vein occlusion. A randomized clinical trial. Arch Ophthalmol 1986; 104: 34–41.
Barbazetto IA, Schmidt-Erfurth MD . Evaluation of functional defects in branch retinal vein occlusion before and after treatment with scanning laser perimetry. Ophthalmology 2000; 107: 1089–1098.
Kriechbaum K, Michels S, Prager F, Georgopoulos M, Funk M, Geitzenauer W et al. Intravitreal Avastin for macular oedema secondary to retinal vein occlusion: a prospective study. Br J Ophthalmol 2007; 92: 518–522.
Rosenfeld PJ, Fung AE, Puliafito CA . Optical coherence findings after an intravitreal injection of bevacizumab (Avastin) for macular edema from central retinal vein occlusion. Ophthalmic Surg Lasers Imaging 2005; 36: 336–339.
Iturralde D, Spaide RF, Meyerle CB, Klancnik JM, Yannuzzi LA, Fisher YL et al. Intravitreal bevacizumab (Avastin) treatment for macular edema in central retinal vein occlusion: a short term study. Retina 2006; 26: 279–284.
Roth DB, Cukras C, Radhakrishnan R, Feuer WJ, Yarian DL, Green SN et al. Intravitreal triamcinolone acetonide injections in the treatment of retinal vein occlusions. Ophthalmic Surg Lasers Imaging 2008; 39: 446–454.
Cakir M, Dogan M, Bayraktar Z, Bayraktar S, Acar N, Altan T et al. Efficacy of intravitreal triamcinolone for the treatment of macular edema secondary to branch retinal vein occlusions in eyes with or without grid laser photocoagulation. Retina 2008; 28: 465–472.
Karacorlu M, Karacorlu SA, Ozdemir H, Senturk F . Intravitreal triamcinolone for the treatment of the serous detachment in central retinal vein occlusions. Retina 2007; 27: 1026–1030.
Moschos MM, Brouzas D, Loukianou E, Apostolopoulos M, Moschos M . Intraocular triamcinolone acetonide for macular edema due to CRVO A multifocal-ERG and OCT study. Doc Ophthalmol 2007; 114: 1–7.
Stamatovic SM, Keep RF, Kunkel SL, Andjelkovic AV . Potential role of MCP-1 in endothelial cell tight junction ‘opening’: signaling via Rho and Rho kinase. J Cell Sci 2003; 116: 4615–4628.
Talavera D, Castillo AM, Dominguez MC, Gutierrez AE, Meza I . IL8 release, tight junction and cytoskeleton dynamic reorganization conducive to permeability increase are induced by dengue virus infection of microvascular endothelial monolayers. J Gen Virol 2004; 85: 1801–1813.
Xu H, Dawson R, Crane IJ, Liversidge J . Leucocyte diapedesis in vivo induces transient loss of tight junction protein at the blood–retina barrier. Invest Ophthalmol Vis Sci 2005; 46: 2487–2494.
Funk M, Kriechbaum K, Prager F, Benesch T, Georgopoulos M, Zlabinger GJ et al. Intraocular concentrations of growth factors and cytokines in retinal vein occlusions and the effect of therapy with bevacizumab. Invest Ophthalmol Vis Sci 2009; 50: 1025–1032.
Roumen-Klappe EM, den Heijer M, van Uum SHM, van der Ven-Jongekrijg J, van der Graaf F, Wollersheim H . Inflammatory response in the acute phase of deep vein thrombosis. J Vasc Surg 2002; 35: 701–706.
Wakefield TW, Greenfield LJ, Rolfe MW, DeLucia III A, Strieter RM, Abrams GD et al. Inflammatory and procoagulant mediator interactions in an experimental baboon model of venous thrombosis. Thromb Haemost 1993; 69: 164–172.
Yoshida A, Elner SG, Bian ZM, Kunkel SL, Lukacs NW, Elner VM . Thrombin regulates chemokine induction during human retinal pigment epithelial cell/monocyte interaction. Am J Pathol 2001; 159: 1171–1180.
Shbaklo H, Holcroft CA, Kahn SR . Levels of inflammatory markers and the development of the post-thrombotic syndrome. Thromb Haemost 2009; 101: 505–512.
Hao Q, Wang L, Tang H . Vascular endothelial growth factor induces protein kinase D-dependent production of pro-inflammatory cytokines in endothelial cells. Am J Physiol Cell Physiol 2009; 296 (4): C821–C827.
Jo N, Wu GS, Rao Na . Upregulation of chemokine expression in the retinal vasculature in ischemia- reperfusion injury. Invest Ophthalmol Vis Sci 2003; 44: 4054–4060.
Davies MH, Eubanks JP, Powers MR . Microglia and macrophages are increased in response to ischemia-induced retinopathy in the mouse retina. Mol Vis 2006; 12: 467–477.
Yoshida S, Yoshida A, Ishibashi T, Elner SG, Elner VM . Role of MCP-1 and MIP-alpha in retinal neovascularization during postischemic inflammation in a mouse model of retinal neovascularization. J Leukoc Biol 2003; 73: 137–144.
Yoshida S, Yoshida A, Ishibashi T . Induction of IL-8, MCP-1 and bFGF by TNF in retinal ganglion cells: implications for retinal neovascularization during post-ischemic inflammation. Graefes Arch Clin Exp Ophthalmol 2004; 242: 409–413.
Acknowledgements
This study was financially supported by Instituto de Salud Carlos III, Madrid, Grant number FIS PI/060803.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This study was partially presented in 2009 ARVO meeting as a poster.
Rights and permissions
About this article
Cite this article
Fonollosa, A., Garcia-Arumi, J., Santos, E. et al. Vitreous levels of interleukine-8 and monocyte chemoattractant protein-1 in macular oedema with branch retinal vein occlusion. Eye 24, 1284–1290 (2010). https://doi.org/10.1038/eye.2009.340
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/eye.2009.340
Keywords
This article is cited by
-
The correlation between cytokine levels in the aqueous humor and the prognostic value of anti-vascular endothelial growth factor therapy for treating macular edema resulting from retinal vein occlusion
Graefe's Archive for Clinical and Experimental Ophthalmology (2021)
-
Mo-derived perivascular macrophage recruitment protects against endothelial cell death in retinal vein occlusion
Journal of Neuroinflammation (2019)
-
Combination of Bevacizumab and NGF Reduces the Risk of Diabetic Retinopathy
Cell Biochemistry and Biophysics (2015)