Abstract
Purpose
Despite demonstrated cost effectiveness, not all corneal disorders are amenable to type I Boston keratoprosthesis (KPro) implantation. This includes patients with autoimmune diseases, such as Stevens–Johnson syndrome/toxic epidermal necrolysis. Type II KPro is implanted through the eyelids in severe dry eye and cicatricial diseases, and its cost effectiveness was sought.
Patients and methods
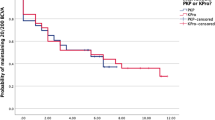
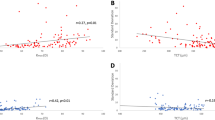
In a retrospective chart review, 29 patients who underwent type II KPro surgery at the Massachusetts Eye and Ear Infirmary between the years 2000 and 2009 were identified. A total of 11 patients had 5-year follow-up data. Average cost effectiveness was determined by cost-utility analysis, comparing type II KPro surgery with no further intervention.
Results
Using the current parameters, the cost utility of KPro from third-party insurer (Medicare) perspective was 63 196 $/quality-adjusted life year.
Conclusion
Efforts to refer those less likely to benefit from traditional corneal transplantation or type I KPro, for type II KPro surgery, may decrease both patient and societal costs.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Ament JD, Stryjewski TP, Ciolino JB, Todani A, Chodosh J, Dohlman CH . Cost-Effectiveness of the Boston Keratoprosthesis. Am J Ophthalmol 2010; 149 (2): 221–228.
Foster CS . Immunologic disorders of the conjunctiva, cornea, and sclera. In: Albert DM, Jakobiec FA (eds). Principles and practice of ophthalmology, 2nd ed Philadelphia, Pennsylvania: WB Saunders, 1999; 821–823.
Tugal-Tutkun I, Akova YA, Foster CS . Penetrating keratoplasty in cicatrizing conjunctival diseases. Ophthalmology 1995; 102: 576–585.
Solomon A, Ellies P, Anderson DF, Touhami A, Grueterich M, Espana EM et al. Long-term outcome of keratolimbal allograft with or without penetrating keratoplasty for total limbal stem cell deficiency. Ophthalmology 2002; 109: 1159–1166.
Dohlman CH, Doane M . Keratoprosthesis in end-stage dry eye. Adv Exp Med Biol 1994; 350: 561–564.
Dohlman CH, Terada H . Keratoprosthesis in pemphigoid and Stevens-Johnson syndrome. Adv Exp Med Biol 1998; 438: 1021–1025.
Yaghouti F, Nouri M, Abad JC, Power WJ, Doane MG, Dohlman CH . Keratoprosthesis: preoperative prognostic categories. Cornea 2001; 20: 19–23.
Sayegh RR, Ang LPK, Foster S, Dohlman CH . The Boston Keratoprosthesis in Stevens-Johnson Syndrome. Am J Ophthalmol 2008; 145 (3): 438–444.
Geerling G, Liu CSC, Collin JRO, Dart JKG . Costs and gains of complex procedures to rehabilitate end stage ocular surface disease. Br J Ophthalmol 2002; 86: 1220–1221.
Falcinelli G, Falsini B, Taloni M, Colliardo P, Falcinelli G . Modified osteo-odonto-keratoprosthesis for treatment of corneal blindness: long-term anatomical and functional outcomes in 181 cases. Arch Ophthalmol 2005; 123 (10): 1319–1329.
Liu C, Okera S, Tandon R, Herold J, Hull C, Thorp S . Visual rehabilitation in end-stage inflammatory ocular surface disease with the osteo-odonto-keratoprosthesis: results from the UK. Br J Ophthalmol 2008; 92 (9): 1211–1217.
Dohlman JG, Foster CS, Dohlman CH . Boston Keratoprosthesis in Steven-Johnson Syndrome: a case of using infliximab to prevent tissue necrosis. DJO 2009; 15 (1).
Aldave AJ, Kamal KM, Vo RC, Yu F . The Boston type I keratoprosthesis: improving outcomes and expanding indications. Ophthalmology 2009; 116 (4): 640–651.
Brown MM, Brown GC . How to interpret a healthcare economic analysis. Curr Opin Ophthalmol 2005; 16 (3): 191–194.
Brown GC, Brown MM, Sharma S . Health care economic analyses. Retina 2004; 24 (1): 139–146.
Dohlman CH, Harissi-Dagher M, Khan BF, Sippel K, Aquavella JV, Graney JM . Introduction to the use of the Boston keratoprosthesis. Expert Rev Ophthalmol 2006; 1 (1): 41–48.
Gold MR, Siegel JE, Russell LB, Weinstein MC . Cost-effectiveness in Health and Medicine. Oxford University Press: New York, 1996; 1–413.
Brown MM, Brown GC, Sharma S, Garrett S . Evidence-based medicine, utilities, and quality of life. Curr Opin Ophthalmol 1999; 10 (3): 221–226.
Hirneiss C, Neubauer AS, Niedermeir A, Messmer EM, Ulbig M, Kampik A . Cost utility for penetrating keratoplasty in patients with poor binocular vision. Ophthalmology 2006; 113: 2176–2180.
McCabe C, Claxton K, Culyer AJ . The NICE cost-effectiveness threshold—What it is and what that means. Pharmacoeconomics 2008; 26 (9): 733–744.
Devlin N, Parkin D . Does NICE have a cost-effectiveness threshold and what other factors influence its decisions? A binary choice analysis. Health Econ 2004; 13 (5): 437–452.
Summary of VELCADE Response Scheme. National Institute for Health and Clinical Excellence, October 2008. Available at http://www.nice.org.uk/nicemedia/pdf/MyelomaDofHSummaryResponderScheme.pdf. Accessed 30 January 2010.
CPI Inflation Calculator. U.S. Bureau of Labor Statistics: Washington, DC, 2010 Available at http://www.bls.gov/data/inflation_calculator.htm. Accessed on: March 3.
Busbee BG, Brown MM, Brown GC, Sharma S . Incremental cost-effectiveness of initial cataract surgery. Ophthalmology 2002; 109 (3): 606–612.
Busbee BG, Brown MM, Brown GC, Sharma S . Cost-utility analysis of cataract surgery in the second eye. Ophthalmology 2003; 110 (12): 2310–2317.
Sharma S, Brown GC, Brown MM, Hollands H, Shah GK . The cost-effectiveness of photodynamic therapy for fellow eyes with subfoveal choroidal neovascularization secondary to age-related macular degeneration. Ophthalmology 2001; 108 (11): 2051–2059.
Losina E, Walensky RP, Kessler CL, Emrani PS, Reichmann WM, Wright EA et al. Cost-effectiveness of total knee arthroplasty in the United States. Arch Intern Med 2009; 169 (12): 1113–1121.
Cummins JS, Tomek IM, Kantor SR, Furnes O, Engesaeter LB, Finlayson SR . Cost-effectiveness of antibiotic-impregnated bone cement used in primary total hip arthroplasty. J Bone Joint Surg Am 2009; 91 (3): 634–641.
Griffin SC, Barber JA, Manca A, Sculpher MJ, Thompson SG, Buxton MJ et al. Cost effectiveness of clinically appropriate decisions on alternative treatments for angina pectoris: prospective observational study. BMJ 2007; 334 (7594): 624–628.
Pinkerton SD, Holtgrave DR, Pinkerton HJ . Cost-effectiveness of chemoprophylaxis after occupational exposure to HIV. Arch Intern Med 1997; 157 (17): 1972–1980.
Dayton JD, Kanter KR, Vincent RN, Mahle WT . Cost-effectiveness of pediatric heart transplantation. J Heart Lung Transplant 2006; 25 (4): 409–415.
Kontodimopoulos N, Niakas D . An estimate of lifelong costs and QALYs in renal replacement therapy based on patients’ life expectancy. Health Policy 2008; 86 (1): 85–96.
Xie F, Lo NN, Tarride JE, O’Reilly D, Goeree R, Lee HP . Total or partial knee replacement? Cost-utility analysis in patients with knee osteoarthritis based on a 2-year observational study. Eur J Health Econ 2010; 11 (1): 27–34.
Chang RW, Pellisier JM, Hazen GB . A cost-effectiveness analysis of total hip arthroplasty for osteoarthritis of the hip. JAMA 1996; 275 (11): 858–865.
Mushlin AI, Mooney C, Holloway RG, Detsky AS, Mattson DH, Phelps CE . The cost-effectiveness of magnetic resonance imaging for patients with equivocal neurological symptoms. Int J Technol Assess Health Care 1997; 13 (1): 21–34.
Faucett SC, Genuario JW, Tosteson AN, Koval KJ . Is prophylactic fixation a cost-effective method to prevent a future contralateral fragility hip fracture? J Orthop Trauma 2010; 24 (2): 65–74.
Jacobson JJ, Schweitzer SO, Kowalski CJ . Chemoprophylaxis of prosthetic joint patients during dental treatment—a decision-utility analysis. Oral Surgery Oral Med Oral Pathol 1991; 72 (2): 167–177.
Geerling G, Liu CS, Collin JR, Dart JK . Costs and gains of complex procedures to rehabilitate end stage ocular surface disease. Br J Ophthalmol 2002; 86 (11): 1220–1221.
Acknowledgements
We thank Kathy Colby, MD, PhD—Massachusetts Eye and Ear Infirmary and Ann Burke—Cost and Budget Manager. Both contributed to cost data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Dr Dohlman receives no personal profits from the sale of the Boston Keratoprosthesis. Proceeds go to the Massachusetts Eye and Ear Infirmary, and are used to support research and development. The authors are/were employees of the Massachusetts Eye and Ear Infirmary, and receive no financial benefit from the publication of this data. Dr Ament is a Clinical Research Fellow who is paid directly from Dr Dohlman's research and development fund.
Additional information
This work was presented as a poster at the World Cornea Congress Meeting in Boston, April 2010.
Author contributions
Design of the study (JA, TS, SP, SS, JC, and CD); conduct of the study (JA, TS, SP, SS, JC, and CD); analysis and interpretation (JA, GP, JC, and TS); writing the article (JA and TS); critical revision (JA, TS, SP, SS, GP, JC, and CD); final approval (JA, TS, SP, SS, GP, JC, and CD); data collection (JA, TS, SP, SS, and GP); provision of materials (SP, SS, GP, JC, and CD); statistical expertise (JA and JC); and literature search (JA and TS).
Ethics
The study was found to be exempted from review by the Human Studies Committee under Paragraph no. 4 of the Code of Federal Regulations 45 CFR 46.101(b). An IRB approval was received to collect data from medical records of patient. The project does not fall under HIPAA requirements because no protected health information is recorded or linked by code to data. The manuscript, its design, and implementation are in full adherence to the Declaration of Helsinki and all federal or state laws in the USA.
Rights and permissions
About this article
Cite this article
Ament, J., Stryjewski, T., Pujari, S. et al. Cost effectiveness of the type II Boston keratoprosthesis. Eye 25, 342–349 (2011). https://doi.org/10.1038/eye.2010.197
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/eye.2010.197