Abstract
Aim
To report the vitreoretinal (VR) surgical case mix in the United Kingdom, the intraoperative complication rate of pars plana vitrectomy (PPV), and the incidence of post-vitrectomy cataract extraction.
Methods
Participating hospitals prospectively collected ophthalmic data using a single electronic medical record system, with automatic extraction of anonymised data to a national database. This study included the subset of 11 618 VR operations undertaken on 9619 eyes, of 8741 patients, over 8 years, from 27 sites. Surgical data included the indication for surgery, all procedure elements, and whether or not an intraoperative complication occurred. Post-vitrectomy cataract data were also analysed. The main outcome measures were a description of the indications for surgery, intraoperative PPV complication rate, and percentage of eyes undergoing post-vitrectomy cataract surgery (PVCS).
Results
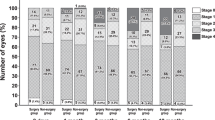
The most common indications for VR intervention were retinal breaks and rhegmatogenous retinal detachment (48.5%), macular hole (9.8%), epiretinal membrane (9.6%), and diabetic eye disease (7.3%). Overall, 7.8% of PPVs had at least one intraoperative complication—the most common were iatrogenic retinal breaks (3.2%), and lens touch (1.2–1.6% of phakic eyes). PVCS occurred in 50.2, 68.7, and 74.0% of eyes at 1, 2, and 3 years, respectively.
Conclusion
VR surgery is undertaken for a wide range of conditions, but a small number of diagnoses encompass the majority of cases. Intraoperative PPV complications are not uncommon, and post-vitrectomy cataract is to be expected in most phakic eyes.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Johnston RL, Sparrow JM, Canning CR, Tole D, Price NC . Pilot national electronic cataract surgery survey: I. Method, descriptive, and process features. Eye 2005; 19: 788–794.
Javitt JC . Rule Britannia. Eye 2005; 19: 727–728.
Jaycock P, Johnston RL, Taylor H, Adams M, Tole DM, Galloway P et al. The cataract national dataset electronic multi-centre audit of 55,567 operations: updating benchmark standards of care in the United Kingdom and internationally. Eye 2009; 23: 38–49.
Narendran N, Jaycock P, Johnston RL, Taylor H, Adams M, Tole DM et al. The cataract national dataset electronic multicentre audit of 55 567 operations: risk stratification for posterior capsule rupture and vitreous loss. Eye 2009; 23: 31–37.
Sparrow JM, Taylor H, Qureshi K, Smith R, Johnston RL . The cataract national data set electronic multi-centre audit of 55 567 operations: case-mix adjusted surgeon’s outcomes for posterior capsule rupture. Eye 2011; 25: 1010–1015.
NHS Connecting for Health. OPCS Classification of Interventions and Procedures Version 4.6 (Vols 1 and 2). The Stationery Office: London, 2011.
Kaplan EL, Meier P . Nonparametric estimation from incomplete observations. J Am Statist Assn 1958; 53: 457–481.
Misra A, Ho-Yen G, Burton RL . 23-Gauge sutureless vitrectomy and 20-gauge vitrectomy: a case series comparison. Eye 2009; 23: 1187–1191.
Ehrlich R, Goh YW, Ahmad N, Polkinghorne P . Retinal breaks in small-gauge pars plana vitrectomy. Am J Ophthalmol 2012; 153: 868–872.
Ramkissoon YD, Aslam SA, Shah SP, Wong SC, Sullivan PM . Risk of iatrogenic peripheral retinal breaks in 20-G pars plana vitrectomy. Ophthalmology 2010; 117: 1825–1830.
Gosse E, Newsom R, Lochhead J . The incidence and distribution of iatrogenic retinal tears in 20-gauge and 23-gauge vitrectomy. Eye 2012; 26: 140–143.
Issa SA, Connor A, Habib M, Steel DHW . Comparison of retinal breaks observed during 23 gauge transconjunctival vitrectomy versus conventional 20 gauge surgery for proliferative diabetic retinopathy. Clin Ophthalmol 2011; 5: 109–114.
Submacular Surgery Trials Pilot Study Investigators. Submacular surgery trials randomized pilot trial of laser photocoagulation versus surgery for recurrent choroidal neovascularization secondary to age-related macular degeneration: I. Ophthalmic outcomes. SST pilot study report no. 1. Am J Ophthalmol 2000; 130: 387–407.
Anon. Two-year course of visual acuity in severe proliferative diabetic retinopathy with conventional management. Diabetic retinopathy vitrectomy study (DRVS) report #1. Ophthalmology 1985; 92: 492–502.
Wickham L, Bunce C, Wong D, McGurn D, Charteris DG . Randomized controlled trial of combined 5-Fluorouracil and low-molecular-weight heparin in the management of unselected rhegmatogenous retinal detachments undergoing primary vitrectomy. Ophthalmology 2007; 114: 698–704.
Heimann H, Bartz-Schmidt KU, Bornfeld N, Weiss C, Hilgers RD, Foerster MH et al. Scleral buckling versus primary vitrectomy in rhegmatogenous retinal detachment: a prospective randomized multicenter clinical study. Ophthalmology 2007; 114: 2142–2154.
Dugel PU, Bebchuk JD, Nau J, Reichel E, Singer M, Barak A et al. Epimacular brachytherapy for neovascular age-related macular degeneration: (CABERNET): a randomized, controlled trial. Ophthalmology 2013; 120: 317–327.
Dogramaci M, Lee EJ, Williamson TH . The incidence and the risk factors for iatrogenic retinal breaks during pars plana vitrectomy. Eye 2012; 26: 718–722.
Rizzo S, Belting C, Genovesi-Ebert F, di Bartolo E . Incidence of retinal detachment after small-incision, sutureless pars plana vitrectomy compared with conventional 20-gauge vitrectomy in macular hole and epiretinal membrane surgery. Retina 2010; 30: 1065–1071.
Ho JD, Kuo NW, Tsai CY, Liou SW, Lin HC . Surgeon age and operative outcomes for primary rhegmatogenous retinal detachment: a 3-year nationwide population-based study. Eye 2010; 24: 290–296.
Ramulu PY, Do DV, Corcoran KJ, Corcoran SL, Robin AL . Use of retinal procedures in medicare beneficiaries from 1997–2007. Arch Ophthalmol 2010; 128: 1335–1340.
Jackson TL, Donechie PHJ, Sparrow JM, Johnston RL . United Kingdom national ophthalmology database study of vitreoretinal surgery: report 2, macular hole. Ophthalmology 2012 e-pub ahead of print 1 December 2012; doi: 10.1016/j.ophtha.2012.09.003.
Acknowledgements
We thank the vitreoretinal surgeons from the following sites for contributing data: Aintree Hospitals NHS Trust; Airedale NHS Foundation Trust & Bradford Teaching Hospitals NHS Foundation Trust; Barking, Havering and Redbridge University hospitals NHS Trust; Bedford Hospital NHS Trust; Cambridge University Hospitals NHS Foundation Trust; Calderdale and Huddersfield NHS Foundation Trust; Dumfries and Galloway Community Health NHS Trust; Epsom and St Helier University Hospitals NHS Trust; Gloucestershire Hospitals NHS Foundation Trust; Grampian Healthcare NHS Trust; King's College Hospital NHS Foundation Trust; Leeds Teaching Hospitals NHS Trust; Mid Cheshire Hospitals NHS Foundation Trust; Mid Yorkshire Hospitals NHS Trust; Norfolk and Norwich University Hospitals NHS Foundation Trust; North Devon Healthcare NHS Trust; Peterborough and Stamford Hospitals NHS Foundation Trust; Portsmouth Hospitals NHS Trust; Royal Berkshire NHS Foundation Trust; Royal United Hospital Bath NHS Trust; South London Healthcare NHS Trust; South Warwickshire NHS Foundation Trust; The Hillingdon Hospital NHS Trust; University Hospitals Birmingham NHS Foundation Trust; University Hospitals Bristol NHS Foundation Trust; Winchester and Eastleigh Healthcare NHS Trust; Wirral University Teaching Hospital NHS Foundation Trust.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
T. Jackson and P. Donachie’s employer received unrestricted funding from Thrombogenics to analyse these data. Thrombogenics had no data access, nor any input in the study design, data analysis, or manuscript preparation. R. Johnston is the Medical Director of Medisoft Limited, which developed the electronic medical record from which data were extracted, for the first iteration of the National Ophthalmology Database.
Rights and permissions
About this article
Cite this article
Jackson, T., Donachie, P., Sparrow, J. et al. United Kingdom National Ophthalmology Database Study of Vitreoretinal Surgery: Report 1; Case mix, complications, and cataract. Eye 27, 644–651 (2013). https://doi.org/10.1038/eye.2013.12
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/eye.2013.12
Keywords
This article is cited by
-
Twenty-seven-gauge vitrectomy: a consecutive, single-centre case series with exclusive use over a 4-year period
BMC Ophthalmology (2023)
-
Two-port dry vitrectomy for rhegmatogenous retinal detachment: a pilot study
Eye (2023)
-
The effect of ethnicity on anatomic success following macular hole surgery: a multicentre cohort study
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)
-
A simple twist technique for lens-sparing one-handed peripheral vitrectomy in phakic patients: a learning approach for junior surgeons
International Journal of Retina and Vitreous (2022)
-
Influence of the scleral indentation technique on the re-detachment rate following retinal detachment surgery
International Journal of Retina and Vitreous (2022)