Abstract
Purpose
To compare the diagnostic abilities of structural (ganglion cell-inner plexiform layer (GCIPL) thickness measured using spectral domain optical coherence tomography (SDOCT)) and functional (visual sensitivities measured using standard automated perimetry (SAP) and microperimetry (MP)) assessments of macula in glaucoma.
Methods
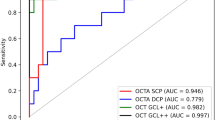
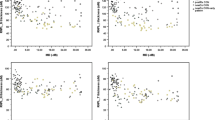
In a prospective study, 46 control eyes (28 subjects) and 61 glaucoma eyes (46 patients) underwent visual sensitivity estimation at macula (central 10°) by SAP and MP, and GCIPL thickness measurement at macula by SDOCT. Glaucoma was diagnosed by experts based on the optic disc and retinal nerve fiber layer changes. Area under the receiver-operating characteristic (AUC) curves and sensitivities at 95% specificity were used to assess the diagnostic ability of visual sensitivity and GCIPL measurements at various macular sectors.
Results
AUCs of GCIPL parameters ranged between 0.58 and 0.79. AUCs of SAP and MP sensitivities ranged between 0.59 and 0.71, and 0.59 and 0.72, respectively. There were no statistically significant differences between the AUCs of corresponding sector measurements (P>0.10 for all comparisons). Sensitivities at 95% specificities ranged from 31–59% for GCIPL parameters, 16–34% for SAP, and 8–38% for MP parameters. Sensitivities were significantly better with GCIPL compared with SAP and MP parameters in diagnosing glaucoma. Inferotemporal, inferior, and superotemporal sector measurements of GCIPL and visual sensitivity showed the best abilities to diagnose glaucoma.
Conclusions
Comparing the diagnostic abilities of structural and functional tests at macula in glaucoma, GCIPL thickness measurements with SDOCT performed better than the visual sensitivity measurements by SAP and MP.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Rao HL, Zangwill LM, Weinreb RN, Sample PA, Alencar LM, Medeiros FA . Comparison of different spectral domain optical coherence tomography scanning areas for glaucoma diagnosis. Ophthalmology 2010; 117: 1692–1699.
Rao HL, Babu JG, Addepalli UK, Senthil S, Garudadri CS . Retinal nerve fiber layer and macular inner retina measurements by spectral domain optical coherence tomograph in Indian eyes with early glaucoma. Eye (Lond) 2012; 26: 133–139.
Takayama K, Hangai M, Durbin M, Nakano N, Morooka S, Akagi T et al. A novel method to detect local ganglion cell loss in early glaucoma using spectral-domain optical coherence tomography. Invest Ophthalmol Vis Sci 2012; 53: 6904–6913.
Mwanza JC, Durbin MK, Budenz DL, Sayyad FE, Chang RT, Neelakantan A et al. Glaucoma diagnostic accuracy of ganglion cell-inner plexiform layer thickness: comparison with nerve fiber layer and optic nerve head. Ophthalmology 2012; 119: 1151–1158.
Kotowski J, Folio LS, Wollstein G, Ishikawa H, Ling Y, Bilonick RA et al. Glaucoma discrimination of segmented cirrus spectral domain optical coherence tomography (SD-OCT) macular scans. Br J Ophthalmol 2012; 96: 1420–1425.
Jeoung JW, Choi YJ, Park KH, Kim DM . Macular ganglion cell imaging study: glaucoma diagnostic accuracy of spectral-domain optical coherence tomography. Invest Ophthalmol Vis Sci 2013; 54: 4422–4429.
Akashi A, Kanamori A, Nakamura M, Fujihara M, Yamada Y, Negi A . Comparative assessment for the ability of Cirrus, RTVue, and 3D-OCT to diagnose glaucoma. Invest Ophthalmol Vis Sci 2013; 54: 4478–4484.
Nouri-Mahdavi K, Nowroozizadeh S, Nassiri N, Cirineo N, Knipping S, Giaconi J et al. Macular ganglion cell/inner plexiform layer measurements by spectral domain optical coherence tomography for detection of early glaucoma and comparison to retinal nerve fiber layer measurements. Am J Ophthalmol 2013; 156: 1297–1307.
Begum VU, Addepalli UK, Yadav RK, Shankar K, Senthil S, Garudadri CS et al. Ganglion cell-inner plexiform layer thickness of high definition optical coherence tomography in perimetric and preperimetric glaucoma. Invest Ophthalmol Vis Sci 2014; 55: 4768–4775.
Drasdo N, Millican CL, Katholi CR, Curcio CA . The length of Henle fibers in the human retina and a model of ganglion receptive field density in the visual field. Vision Res 2007; 47: 2901–2911.
Hood DC, Raza AS, de Moraes CG, Liebmann JM, Ritch R . Glaucomatous damage of the macula. Prog Retin Eye Res 2013; 32: 1–21.
Schiefer U, Flad M, Stumpp F, Malsam A, Paetzold J, Vonthein R et al. Increased detection rate of glaucomatous visual field damage with locally condensed grids: a comparison between fundus-oriented perimetry and conventional visual field examination. Arch Ophthalmol 2003; 121: 458–465.
Traynis I, De Moraes CG, Raza AS, Liebmann JM, Ritch R, Hood DC . Prevalence and nature of early glaucomatous defects in the central 10 degrees of the visual field. JAMA Ophthalmol 2014; 132: 291–297.
Rohrschneider K, Bultmann S, Springer C . Use of fundus perimetry (microperimetry) to quantify macular sensitivity. Prog Retin Eye Res 2008; 27: 536–548.
Mwanza JC, Oakley JD, Budenz DL, Anderson DR . Ability of cirrus HD-OCT optic nerve head parameters to discriminate normal from glaucomatous eyes. Ophthalmology 2011; 118: 241–248.
Mwanza JC, Oakley JD, Budenz DL, Chang RT, Knight OJ, Feuer WJ . Macular ganglion cell-inner plexiform layer: automated detection and thickness reproducibility with spectral domain-optical coherence tomography in glaucoma. Invest Ophthalmol Vis Sci 2011; 52: 8323–8329.
Sato S, Hirooka K, Baba T, Tenkumo K, Nitta E, Shiraga F . Correlation between the ganglion cell-inner plexiform layer thickness measured with cirrus HD-OCT and macular visual field sensitivity measured with microperimetry. Invest Ophthalmol Vis Sci 2013; 54: 3046–3051.
Hood DC, Kardon RH . A framework for comparing structural and functional measures of glaucomatous damage. Prog Retin Eye Res 2007; 26: 688–710.
Glynn RJ, Rosner B . Accounting for the correlation between fellow eyes in regression analysis. Arch Ophthalmol 1992; 110: 381–387.
Zhou XH, Obuchowski NA, McClish DK . Analysis of correlated ROC data. In: Zhou XH, Obuchowski NA, McClish DK (eds). Statistical Methods in Diagnostic Medicine. Wiley: New York, NY, USA, 2002, pp 274–306.
Alonzo TA, Pepe MS . Distribution-free ROC analysis using binary regression techniques. Biostatistics 2002; 3: 421–432.
Zhou XH, Obuchowski NA, McClish DK . Comparing the accuracy of two diagnostic tests. In: Zhou XH, Obuchowski NA, McClish DK (eds). Statistical Methods in Diagnostic Medicine. Wiley: New York, NY, USA, 2002, pp 165–194.
DeLong ER, DeLong DM, Clarke-Pearson DL . Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 1988; 44: 837–845.
Pepe MS . The Statistical Evaluation of Medical Tests for Classification and Prediction. Oxford University Press: Oxford, UK, 2003, pp 130–167.
Ozturk F, Yavas GF, Kusbeci T, Ermis SS . A comparison among Humphrey field analyzer, microperimetry, and Heidelberg retina tomograph in the evaluation of macula in primary open angle glaucoma. J Glaucoma 2008; 17: 118–121.
Klamann MK, Grunert A, Maier AK, Gonnermann J, Joussen AM, Huber KK . Comparison of functional and morphological diagnostics in glaucoma patients and healthy subjects. Ophthalmic Res 2013; 49: 192–198.
Lima VC, Prata TS, De Moraes CG, Kim J, Seiple W, Rosen RB et al. A comparison between microperimetry and standard achromatic perimetry of the central visual field in eyes with glaucomatous paracentral visual-field defects. Br J Ophthalmol 2010; 94: 64–67.
Orzalesi N, Miglior S, Lonati C, Rosetti L . Microperimetry of localized retinal nerve fiber layer defects. Vision Res 1998; 38: 763–771.
Garway-Heath DF, Hitchings RA . Sources of bias in studies of optic disc and retinal nerve fibre layer morphology. Br J Ophthalmol 1998; 82: 986.
Kim MJ, Jeoung JW, Park KH, Choi YJ, Kim DM . Topographic profiles of retinal nerve fiber layer defects affect the diagnostic performance of macular scans in preperimetric glaucoma. Invest Ophthalmol Vis Sci 2014; 55: 2079–2087.
Mwanza JC, Budenz DL, Godfrey DG, Neelakantan A, Sayyad FE, Chang RT et al. Diagnostic performance of optical coherence tomography ganglion cell-inner plexiform layer thickness measurements in early glaucoma. Ophthalmology 2014; 121: 849–854.
Acknowledgements
Rao HL: Allergan (C), Cipla (C); Hussain SM: none; Januwada M: none; Pillutla LN: none; Begum VU: none; Chaitanya A: none; Senthil S: none; Garudadri CS: Alcon (C).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Rao, H., Hussain, R., Januwada, M. et al. Structural and functional assessment of macula to diagnose glaucoma. Eye 31, 593–600 (2017). https://doi.org/10.1038/eye.2016.277
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/eye.2016.277
This article is cited by
-
Border tissue morphology is associated with macular ganglion cell thickness in open-angle glaucoma
Scientific Reports (2022)
-
Microperimetry, Humphrey field analyzer, and optical coherence tomography in detecting glaucoma: a comparative performance study
International Ophthalmology (2022)
-
Understanding the role of microperimetry in glaucoma
International Ophthalmology (2022)
-
A Comparison Among Microperimetry, Standard Automated Perimetry and Spectral Domain Optical Coherence Tomography in the Evaluation of the Macula in Glaucoma Eyes with Hemifield Defects
Ophthalmology and Therapy (2022)
-
Circumpapillary microperimetry to detect glaucoma: a pilot study for sector-based comparison to circumpapillary retinal nerve fiber layer measurement
International Ophthalmology (2019)