Abstract
Purpose
To identify the causal factors in wrong intraocular lens (IOL) events from a national data set and to compare with similar historical data (2003–2010) prior to mandatory checklist use, for the purpose of developing strategies to prevent never events.
Methods
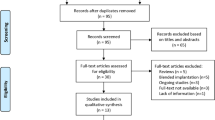
Data from wrong IOL patient safety incidents (PSIs) submitted to the National Reporting and Learning System (2010–2014) were reviewed by thematic analysis and compared with the data previously collected by the group using the same methodology.
Results
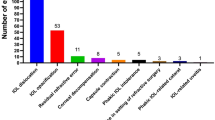
One hundred and seventy eight wrong IOL PSIs were identified. The contributory factors included: transcription errors (n=26); wrong patient biometry (n=21); wrong IOL selection (n=16); changes in planned procedure (n=16); incorrect IOL brought into theatre (n=11); left/right eye selection errors (n=9); communication errors (n=9); and positive/negative IOL power errors (n=9). In 44 PSIs, no causal factor was reported, limiting the learning value of such reports. Compared with the data from previous years, biometry errors were much reduced but IOL transcription and documentation errors were greater, particularly if further checks did not refer to the original source documentation. IOL exchange surgery was reported in 45 cases.
Conclusions
The selection and implantation of the correct IOL is a complex process which is not adequately addressed by existing checking procedures. Despite the introduction of surgical checklists, wrong IOL incidents continue to occur and are probably under-reported. Human or behavioural factors are heavily implicated in these errors and need to be addressed by novel approaches, including simulation training. There is also scope to further improve the quality and detail of incident reporting and analysis to enhance patient safety.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Health and Social Care Information Centre. Hospital episode statistics admitted patient care England 2013–2014. Available at http://www.hscic.gov.uk/catalogue/PUB16719/hosp-epis-stat-admi-summ-rep-2013-14-rep.pdf. (accessed 26 November 2015).
Agarwal A, Kumar DA . Cost effectiveness of cataract surgery. Curr Opin Ophthalmol 2011; 22: 15–18.
National Patient Safety Agency. Never Events Framework 2009/2010. National Patient Safety Agency: London, 2009. Available at www.nrls.npsa.nhs.uk/neverevents/?entryid45=59859. (accessed 26 November 2015).
Neily J, Mills PD, Eldridge N, Carney BT, Pfeffer D, Turner JR et al. Incorrect Surgical procedures within and outside of the operating room: a follow–up report. Arch Surg 2011; 146: 1235–1239.
Haynes AB, Weiser TG, Berry WR, Lipsitz SR, Breizat AH, Dellinger EP et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med 2009; 360: 491–499.
de Vries EN, Prins HA, Crolla RM, den Outer AJ, van Andel G, van Helden SH et al. Effect of a comprehensive surgical safety system on patient outcomes. N Engl J Med 2010; 363: 1928–1937.
Neily J, Mills PD, Young-Xu Y, Carney BT, West P, Berger DH et al. Association between implementation of a medical team training program and surgical mortality. JAMA 2010; 304: 1693–1700.
Lum F, Schachat AP . The quest to eliminate never events. Ophthalmology 2009; 116: 1021–1022.
National Patient Safety Agency WHO Surgical Safety Checklist: For Cataract Surgery Only. National Patient Safety Agency: London, 2010 Available at http://www.nrls.npsa.nhs.uk/resources/clinical-specialty/surgery/?entryid45=74132.
Department of Health An Organisation With a Memory. Department of Health: London, 2000 Available at http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4065086.pdf.
Kelly SP . Guidance on patient safety in ophthalmology from the Royal College of Ophthalmologists. Eye 2009; 23: 2143–2151.
NHS England National Reporting and Learning System. NHS England: London, Available at https://report.nrls.nhs.uk/nrlsreporting/.
Kelly SP, Jalil A . Wrong intraocular lens implant; learning from reported patient safety incidents. Eye 2011; 25: 730–734.
Health and Social Care Information Centre. Hospital episode statistics admitted patient care England 2010, 2013 and 2014. Available at http://www.hscic.gov.uk/article/2021/Website-Search?q=title%3a+%22hospital+outpatient+activity%22&sort=Most+recent&size=10&page=1&area=both#top.
Sari AB, Sheldon TA, Cracknell A, Turnbull A . Sensitivity of routine system for reporting patient safety incidents in an NHS hospital: retrospective patient case note review. BMJ 2007; 334: 79.
Panesar SS, Noble DJ, Mirza SB, Patel B, Mann B, Emerton M et al. Can the surgical checklist reduce the risk of wrong site surgery in orthopaedics?—Can the checklist help? Supporting evidence from analysis of a national patient incident reporting system. J Orthop Surg Res 2011; 6: 18.
NHS England Never Events List 2013/14 update. NHS England: London, 2013 Available at http://www.england.nhs.uk/wp-content/uploads/2013/12/nev-ev-list-1314-clar.pdf.
NHS England Never Events list 2015/2016. NHS England: London, 2015. http://www.england.nhs.uk/wp-content/uploads/2015/03/never-evnts-list-15-16.pdf.
Hingorani M, Flanagan D . Wrong IOLs and never events in ophthalmology. College News 2014.
Neily J, Chomsky A, Orcutt J, Paull DE, Mills PD, Gilbert C et al. Examining wrong eye implant adverse events in the Veterans Health Administration with a focus on prevention: a preliminary report. J Patient Saf 2015; e-pub ahead of print 16 March 2015.
NHS England Standardise, educate, harmonise. Commissioning the conditions for safer surgery Summary of the report of the NHS England Never Events Taskforce. NHS England: London, 2014. Available at http://www.england.nhs.uk/wp-content/uploads/2014/02/sur-nev-ev-tf-sum-rep.pdf.
NHS England Never Events Reported As Occurring Between 1 April 2013 and 31 March 2014. NHS England: London, 2014. Available at http://www.england.nhs.uk/wp-content/uploads/2014/12/2013-14-NE-data-FINAL.pdf.
Ali N . A decade of clinical negligence in ophthalmology. BMC Ophthalmol 2007; 7: 20.
Mathew RG, Ferguson V, Hingorani M . Clinical negligence in ophthalmology: fifteen years of national health service litigation authority data. Ophthalmology 2013; 120: 859–864.
Zamir E, Beresova-Creese K, Miln L . Intraocular lens confusions: a preventable “Never Event”—The Royal Victorian Eye and Ear Hospital Protocol. Surv Ophthalmol 2012; 57: 430–447.
The Royal College of Ophthalmologists Significant Events in Cataract Surgery. The Royal College of Ophthalmologists: London, Available at https://www.rcophth.ac.uk/professional-resources/revalidation/clinical-sub-specialties/cataract/significant-events-in-cataract-surgery/.
Azuara-Blanco A, Reddy A, Wilkinson G, Flin R . Safe eye surgery: non-technical aspects. Eye 2011; 25: 1109–1111.
Sendlhofer G, Mosbacher N, Karina L, Kober B, Jantscher L, Berghold A et al. Implementation of a surgical safety checklist: interventions to optimize the process and hints to increase compliance. PLoS ONE 2015; 10: e0116926.
Gillespie BM, Marshall A . Implementation of safety checklists in surgery: a realist synthesis of evidence. Implement Sci 2015; 10: 137.
NHS England Patient Safety Domain. Patient Safety Alert. Stage 2, supporting the introduction of the National Safety Standards for Invasive Procedures 2015. Available at http://www.england.nhs.uk/wp-content/uploads/2015/09/psa-natssips.pdf. (accessed 26 November 2015)..
NHS England Patient Safety Domain. National Safety Standards for Invasive Procedures 2015 Available at http://www.england.nhs.uk/patientsafety/wp-content/uploads/sites/32/2015/09/natssips-safety-standards.pdf. (accessed 26 November 2015)..
Paull DE, Mazzia LM, Neily J, Mills PD, Turner JR, Gunnar W et al. Errors upstream and downstream to the Universal Protocol associated with wrong surgery events in the Veterans Health Administration. Am J Surg 2015; 210: 6–13.
Urbach DR, Govindarajan A, Saskin R, Wilton AS, Baxter NN . Introduction of surgical safety checklists in Ontario, Canada. N Engl J Med 2014; 370: 1029–1038.
Gagliardi AR, Straus SE, Shojania KG, Urbach DR . Multiple interacting factors influence adherence, and outcomes associated with surgical safety checklists: a qualitative study. PLoS One 2014; 9: e108585.
Helmreich RL, Merritt AC, Wilhelm JA . The evolution of crew resource management training in commercial aviation. Int J Aviat Psychol 1999; 9: 19–32.
Holzman RS, Cooper JB, Gaba DM, Philip JH, Small SD, Feinstem D . Anesthesia crisis resource management: real-life simulation training in operating room crises. J Clin Anesth 1995; 7: 675–687.
Cook DA, Hatala R, Brydges R, Zendejas B, Szostek JH, Wang AT et al. Technology-enhanced simulation for health professions education: a systematic review and meta-analysis. JAMA 2011; 306: 978–988.
Hempel S, Maggard-Gibbons M, Nguyen DK, Dawes AJ, Miake-Lye I, Beroes JM et al. Wrong-site surgery, retained surgical items, and surgical fires: a systematic review of surgical never events. JAMA Surg 2015; 150: 796–805.
National Patient Safety Agency Seven Steps to Patient Safety. National Patient Safety Agency: London, 2004. Available at http://www.nrls.npsa.nhs.uk/resources/collections/seven-steps-to-patient-safety/?entryid45=59787.
Patient Safety Information. Checklist Examples. The Royal College of Ophthalmologists 2015. Available at https://www.rcophth.ac.uk/standards-publications-research/patient-safety-information/. (accessed 26 November 2015)..
Acknowledgements
We are grateful to the staff at the National Reporting and Learning System for data extraction.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Steeples, L., Hingorani, M., Flanagan, D. et al. Wrong intraocular lens events—what lessons have we learned? A review of incidents reported to the National Reporting and Learning System: 2010–2014 versus 2003–2010. Eye 30, 1049–1055 (2016). https://doi.org/10.1038/eye.2016.87
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/eye.2016.87
This article is cited by
-
Principles of simulation and their role in enhancing cataract surgery training
Eye (2022)
-
Comparisons between cataract surgery and aviation
Eye (2022)
-
Development of the HUman Factors in intraoperative Ophthalmic Emergencies Scoring System (HUFOES) for non-technical skills in cataract surgery
Eye (2021)
-
Validity of scoring systems for the assessment of technical and non-technical skills in ophthalmic surgery—a systematic review
Eye (2021)
-
Refractive surprise after cataract surgery secondary to smeared optics of swept-source optical coherence tomography biometer: a case report
BMC Ophthalmology (2020)