Abstract
Purpose
To compare the structural changes, clinical course, and treatment outcomes of vertical and horizontal vitreomacular traction (VMT) induced impending macular holes (IMHs) and full-thickness macular holes (FTMHs).
Methods
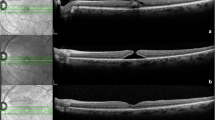
In this retrospective study, 23 and 32 cases of IMHs and FTMHs, respectively, were analyzed. The IMH cases were divided into two subgroups: IMH with and without foveal detachment. Vitreofoveal traction angles (TAs) between the inner retinal surface and posterior hyaloid were measured from horizontal and vertical optical coherence tomography (OCT) images by using the trigonometric function (the angle equals the arctangent of the height over the base) after adjustments for magnification factors. The largest angle was defined as the vitreomacular TA for the examined case. The critical angle—the TA differentiating cases with (vertical traction) or without (horizontal traction) foveal detachment (vertical traction)—was determined using regression analysis. Pretreatment and posttreatment OCT images, clinical courses, and treatment outcomes were compared between the two groups.
Results
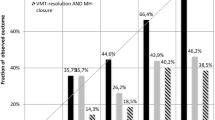
The critical angle was 27.2°. Cases of vertical traction had higher foveal height in the IMH group and wider bases in the FTMH group (P<0.05 respectively). IMHs with vertical traction had greater VM attachment than those with horizontal traction. In the FTMH group, postoperative visual improvement was lower (P=0.002); in the vertical traction group, inner segment:outer segment defects persisted longer (P=0.02).
Conclusions
The critical angle separating vertical from horizontal traction was 27.2°. Vertical VMT results in greater foveal structural changes in IMHs and possibly less favorable surgical outcomes in FTMHs.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Johnson MW, Van Newkirk MR, Meyer KA . Perifoveal vitreous detachment is the primary pathogenic event in idiopathic macular hole formation. Arch Ophthalmol 2001; 119: 215–222.
Ezra E . Idiopathic full thickness macular hole: natural history and pathogenesis. Br J Ophthalmol 2001; 85: 102–109.
Kim JW, Freeman WR, El-Haig W, Maguire AM, Arevalo JF, Azen SP et al. Baseline characteristics, natural history, and risk factors to progression in eyes with stage 2 macular holes: results from a prospective randomized clinical trial. Ophthalmology 1995; 102: 1818–1829.
Smiddy WE, Flynn HW . Pathogenesis of macular holes and therapeutic implications. Am J Ophthalmol 2004; 137: 525–537.
Gass JDM . Idiopathic senile macular hole: its early stages and pathogenesis. Arch Ophthalmol 1988; 106: 629–639.
Duker JS, Kaiser PK, Binder S, De Smet MD, Gaudric A, Reichel E et al. The International Vitreomacular Traction Study Group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology 2013; 120: 2611–2619.
Asrani S, Zeimer R, Goldberg MF, Zou S . Serial optical sectioning of macular holes at different stages of development. Ophthalmology 1998; 105: 66–77.
Azzolini C, Patelli F, Brancato R . Correlation between optical coherence tomography data and biomicroscopic interpretation of idiopathic macular hole. Am J Ophthalmol 2001; 132: 348–355.
Haouchine B, Massin P, Gaudric A . Foveal pseudocyst as the first step in macular hole formation: a prospective study by optical coherence tomography. Ophthalmology 2001; 108: 15–22.
Kishi S, Kamei Y, Shimizu K . Tractional elevation of Henle’s fiber layer in idiopathic macular holes. Am J Ophthalmol 1995; 120: 486–496.
Kishi S, Takahashi H . Three-dimensional observations of developing macular holes. Am J Ophthalmol 2000; 130: 65–75.
McDonnell PJ, Fine SL, Hillis AI . Clinical features of idiopathic macular cysts and holes. Am J Ophthalmol 1982; 93: 777–786.
Takahashi A, Nagaoka T, Yoshida A . Stage 1-A macular hole: a prospective spectral-domain optical coherence tomography study. Retina 2011; 31: 127–147.
Yeh PT, Chen TC, Yang CH, Ho TC, Chen MS, Huang JS et al. Formation of idiopathic macular hole—reappraisal. Graefes Arch Clin Exp Ophthalmol 2010; 248: 793–798.
Takahashi A, Nagaoka T, Ishiko S, Kameyama D, Yoshida A . Foveal anatomic changes in a progressing stage 1 macular hole documented by spectral-domain optical coherence tomography. Ophthalmology 2010; 117: 806–810.
Takahashi A, Yoshida A, Nagaoka T, Kagokawa H, Kato Y, Takamiya A et al. Macular hole formation in fellow eyes with a perifoveal posterior vitreous detachment of patients with a unilateral macular hole. Am J Ophthalmol 2011; 151: 981–989.
Theodossiadis G, Petrou P, Eleftheriadou M, Kagokawa S, Kato Y, Takamiya A et al. Focal vitreomacular traction: a prospective study of the evolution to macular hole: the mathematical approach. Eye 2014; 28: 1452–1460.
Gass JDM . Reappraisal of biomicroscopic classification of stages of development of a macular hole. Am J Ophthalmol 1995; 119: 752–759.
Spaide RF, Wong D, Fisher Y, Goldbaum M . Correlation of vitreous attachment and foveal deformation in early macular hole states. Am J Ophthalmol 2002; 133: 226–229.
Kishi S, Demaria C, Shimizu K . Vitreous cortex remnants at the fovea after spontaneous vitreous detachment. Int Ophthalmol 1986; 9: 253–260.
Ullrich S, Haritoglou C, Gass Ct, Schaumberger M, Ulbig W, Kampik A . Macular hole size as a prognostic factor in macular hole surgery. Br J Ophthalmol 2002; 86: 390–393.
de Bustros S, Group VfPoMHS. Vitrectomy for prevention of macular holes: results of a randomized multicenter clinical trial. Ophthalmology 1994; 101: 1055–1060.
Hikichi T, Yoshida A, Akiba J, Trempe CL . Natural outcomes of stage 1, 2, 3, and 4 idiopathic macular holes. Br J Ophthalmol 1995; 79: 517–520.
La Cour M, Friis J . Macular holes: classification, epidemiology, natural history and treatment. Acta Ophthalmol Scand 2002; 80: 579–587.
Acknowledgements
We thank the National Taiwan University Hospital for supporting this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Tsai, CY., Hsieh, YT., Lai, TT. et al. Idiopathic macular holes and direction of vitreomacular traction: structural changes and surgical outcomes. Eye 31, 1689–1696 (2017). https://doi.org/10.1038/eye.2017.141
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/eye.2017.141
This article is cited by
-
Systemic oxidative stress biomarkers in patients with vitreomacular traction syndrome
International Ophthalmology (2021)
-
OCT proves that vitreomacular adhesion is significantly more likely to develop vision-threatening retinal complications than vitreomacular separation
BMC Ophthalmology (2020)