Abstract
Background:
Prolonged, moderate-intensity exercise training is routinely prescribed to subjects with obesity. In the general population, this type of exercise can lead to fluid and sodium imbalance. However, little is known whether obesity alters the risk of fluid and sodium imbalances.
Objective:
This study examined physiological responses, such as core body temperature, fluid and sodium balance, in lean (BMI<25), overweight (25<BMI<30) and obese (BMI>30) subjects during prolonged moderate-intensity exercise.
Subjects:
A total of 93 volunteers (24–80 years), stratified for BMI, participated in the Nijmegen Marches and walked 30–50 km at a self-selected pace. Heart rate and core body temperature were recorded every 5 km. Subjects reported fluid intake, while urine output was measured and sweat rate was calculated. Baseline and post-exercise plasma sodium levels were determined, and urinary specific gravity levels were assessed before and after exercise.
Results:
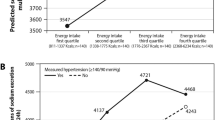
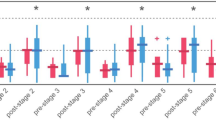
BMI groups did not differ in training status preceding the experiment. Exercise duration (8 h 41±1 h 36 min) and intensity (72±9% HRmax) were comparable across groups, whereas obese subjects tended to have a higher maximum core body temperature than lean controls (P=0.06). Obese subjects demonstrated a significantly higher fluid intake (P<0.001) and sweat rate (P<0.001), but lower urine output (P<0.05) compared with lean subjects. In addition, higher urine specific gravity levels were observed in obese versus lean subjects after exercise (P<0.05). Furthermore, plasma-sodium concentration did not change in lean subjects after exercise, whereas plasma-sodium levels increased significantly (P<0.001) in overweight and obese subjects. Also, overweight and obese subjects demonstrated a significantly larger decrease in body mass after exercise than lean controls (P<0.05).
Conclusion:
Obese subjects demonstrate a larger deviation in markers of fluid and sodium balance than their lean counterparts during prolonged moderate-intensity exercise. These findings suggest that overweight and obese subjects, especially under strenuous environmental conditions, have an increased risk to develop fluid and sodium imbalances.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Gelber RP, Gaziano JM, Orav EJ, Manson JE, Buring JE, Kurth T . Measures of obesity and cardiovascular risk among men and women. J Am Coll Cardiol 2008; 52: 605–615.
Must A, Spadano J, Coakley EH, Field AE, Colditz G, Dietz WH . The disease burden associated with overweight and obesity. Jama 1999; 282: 1523–1529.
Wilson PW, D’Agostino RB, Sullivan L, Parise H, Kannel WB . Overweight and obesity as determinants of cardiovascular risk: the Framingham experience. Arch Intern Med 2002; 162: 1867–1872.
Rissanen A, Heliovaara M, Knekt P, Reunanen A, Aromaa A, Maatela J . Risk of disability and mortality due to overweight in a Finnish population. Bmj 1990; 301: 835–837.
Malnick SD, Knobler H . The medical complications of obesity. Qjm 2006; 99: 565–579.
Flegal KM, Graubard BI, Williamson DF, Gail MH . Cause-specific excess deaths associated with underweight, overweight, and obesity. Jama 2007; 298: 2028–2037.
Prentice AM, Jebb SA . Obesity in Britain: gluttony or sloth? BMJ (Clinical research ed) 1995; 311: 437–439.
Weinsier RL, Hunter GR, Heini AF, Goran MI, Sell SM . The etiology of obesity: relative contribution of metabolic factors, diet, and physical activity. Am J Med 1998; 105: 145–150.
Pietilainen KH, Kaprio J, Borg P, Plasqui G, Yki-Jarvinen H, Kujala UM et al. Physical inactivity and obesity: a vicious circle. Obesity (Silver Spring, Md) 2008; 16: 409–414.
Lee CD, Blair SN, Jackson AS . Cardiorespiratory fitness, body composition, and all-cause and cardiovascular disease mortality in men. Am J Clin Nutr 1999; 69: 373–380.
Lee DC, Sui X, Church TS, Lee IM, Blair SN . Associations of cardiorespiratory fitness and obesity with risks of impaired fasting glucose and type 2 diabetes in men. Diabetes care 2009; 32: 257–262.
Fagard RH . Physical activity in the prevention and treatment of hypertension in the obese. Med Sci Sports Exerc 1999; 31: S624–S630.
Borodulin K, Laatikainen T, Lahti-Koski M, Lakka TA, Laukkanen R, Sarna S et al. Associations between estimated aerobic fitness and cardiovascular risk factors in adults with different levels of abdominal obesity. Eur J Cardiovasc Prev Rehabil 2005; 12: 126–131.
Despres JP, Lemieux I, Prud’homme D . Treatment of obesity: need to focus on high risk abdominally obese patients. BMJ (Clinical research ed) 2001; 322: 716–720.
Grundy SM, Hansen B, Smith Jr SC, Cleeman JI, Kahn RA . Clinical management of metabolic syndrome: report of the American Heart Association/National Heart, Lung, and Blood Institute/American Diabetes Association conference on scientific issues related to management. Circulation 2004; 109: 551–556.
Logue J, Thompson L, Romanes F, Wilson DC, Thompson J, Sattar N . Management of obesity: summary of SIGN guideline. BMJ (Clinical research ed) 2010; 340: c154.
Sawka MN, Burke LM, Eichner ER, Maughan RJ, Montain SJ, Stachenfeld NS . American College of Sports Medicine position stand. Exercise and fluid replacement. Med Sci Sports Exerc 2007; 39: 377–390.
Sawka MN . Physiological consequences of hypohydration: exercise performance and thermoregulation. Med Sci Sports Exerc 1992; 24: 657–670.
Armstrong LE, Maresh CM, Gabaree CV, Hoffman JR, Kavouras SA, Kenefick RW et al. Thermal and circulatory responses during exercise: effects of hypohydration, dehydration, and water intake. J Appl Physiol 1997; 82: 2028–2035.
Cheuvront SN, Carter III R, Sawka MN . Fluid balance and endurance exercise performance. Curr Sports Med Rep 2003; 2: 202–208.
Casa DJ, Armstrong LE, Hillman SK, Montain SJ, Reiff RV, Rich BS et al. National athletic trainers’ association position statement: fluid replacement for athletes. J Athl Train 2000; 35: 212–224.
Havenith G, van Middendorp H . The relative influence of physical fitness, acclimatization state, anthropometric measures and gender on individual reactions to heat stress. Eur j Appl Physiol Occupational Physiology 1990; 61: 419–427.
Robinson S . The effect of body size upon energy exchange in work. Am J Physiol 1942; 36: 363–368.
Chung NK, Pin CH . Obesity and the occurrence of heat disorders. Military medicine 1996; 161: 739–742.
Gardner JW, Kark JA, Karnei K, Sanborn JS, Gastaldo E, Burr P et al. Risk factors predicting exertional heat illness in male Marine Corps recruits. Med Sci Sports Exerc 1996; 28: 939–944.
Dubois D, Dubois EF . A formula to estimate the approximate surface area if height and weight are known. Arch Intern Med 1916; 17: 863–871.
Durnin JV, Womersley J . Body fat assessed from total body density and its estimation from skinfold thickness: measurements on 481 men and women aged from 16 to 72 years. Br J Nutr 1974; 32: 77–97.
Sawka MN, Noakes TD . Does dehydration impair exercise performance? Med Sci Sports Exerc 2007; 39: 1209–1217.
Armstrong LE . Hydration assessment techniques. Nutr Rev 2005; 63: S40–S54.
Hew-Butler T, Ayus JC, Kipps C, Maughan RJ, Mettler S, Meeuwisse WH et al. Statement of the Second International Exercise-Associated Hyponatremia Consensus Development Conference, New Zealand, 2007. Clin J Sport Med 2008; 18: 111–121.
Adrogue HJ, Madias NE . Hypernatremia. N Engl J Med 2000; 342: 1493–1499.
Dill DB, Costill DL . Calculation of percentage changes in volumes of blood, plasma, and red cells in dehydration. J Appl Physiol 1974; 37: 247–248.
Byrne C, Lim CL . The ingestible telemetric body core temperature sensor: a review of validity and exercise applications. Br J Sports Med 2007; 41: 126–133.
Gant N, Atkinson G, Williams C . The validity and reliability of intestinal temperature during intermittent running. Med Sci Sports Exerc 2006; 38: 1926–1931.
Tanaka H, Monahan KD, Seals DR . Age-predicted maximal heart rate revisited. J Am Coll Cardiol 2001; 37: 153–156.
Armstrong LE, Casa DJ, Millard-Stafford M, Moran DS, Pyne SW, Roberts WO . American College of Sports Medicine position stand. Exertional heat illness during training and competition. Med Sci Sports Exerc 2007; 39: 556–572.
ACSM. American College of Sports Medicine Position Stand. The recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, and flexibility in healthy adults. Med Sci Sports Exerc 1998; 30: 975–991.
Byrne NM, Hills AP . Relationships between HR and (.)VO(2) in the obese. Med S Sports Exerc 2002; 34: 1419–1427.
Ball SG . Vasopressin and disorders of water balance: the physiology and pathophysiology of vasopressin. Ann Clin Biochem 2007; 44: 417–431.
Treschan TA, Peters J . The vasopressin system: physiology and clinical strategies. Anesthesiology 2006; 105: 599–612; quiz 639–540.
Stricker EM, Sved AF . Controls of vasopressin secretion and thirst: similarities and dissimilarities in signals. Physiol Behav 2002; 77: 731–736.
Thornton SN . Thirst and hydration: physiology and consequences of dysfunction. Physiol Behav 2010; 100: 15–21.
Medicine IO . Water. National Academy Press: Washington, DC, 2005. pp 73–185.
Chumlea WC, Guo SS, Zeller CM, Reo NV, Siervogel RM . Total body water data for white adults 18–64 years of age: the Fels Longitudinal Study. Kidney Int 1999; 56: 244–252.
Casa DJ, Clarkson PM, Roberts WO . American College of Sports Medicine roundtable on hydration and physical activity: consensus statements. Curr Sports Med Rep 2005; 4: 115–127.
Kavouras SA . Assessing hydration status. Curr Opin Clin Nutr Metab Care 2002; 5: 519–524.
Sawka MN, Young AJ . Physiological systems and their responses to conditions of heat and cold. In: CM Tipton, CA Tate and RL Terjung (eds). ACSM's Advanced Exercise Physiology. Lippincott, Williams & Wilkins: Baltimore, MD, 2005, pp 535–563.
Cheuvront SN, Montain SJ, Sawka MN . Fluid replacement and performance during the marathon. Sports Med 2007; 37: 353–357.
Armstrong LE . Assessing hydration status: the elusive gold standard. J Am Coll Nutr 2007; 26: 575S–584S.
Acknowledgements
We recognize the excellent help of the organization of the International Nijmegen 4 Day Marches, Siemens Medical Solutions Diagnostics BV (Breda, The Netherlands), Noortje van Duijnhoven, Ralph Scholten, Madelijn Sander, Bregina Kersten and Linda Pardoel. Dr Thijssen is financially supported by the Dutch Heart Foundation (E. Dekker-stipend).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Eijsvogels, T., Veltmeijer, M., Schreuder, T. et al. The impact of obesity on physiological responses during prolonged exercise. Int J Obes 35, 1404–1412 (2011). https://doi.org/10.1038/ijo.2010.277
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/ijo.2010.277
Keywords
This article is cited by
-
Interindividual- and blood-correlated sweat phenylalanine multimodal analytical biochips for tracking exercise metabolism
Nature Communications (2024)
-
Thermoregulation and fluid balance during a 30-km march in 60- versus 80-year-old subjects
AGE (2014)
-
Association between bisphenol A exposure and body mass index in Chinese school children: a cross-sectional study
Environmental Health (2012)