Abstract
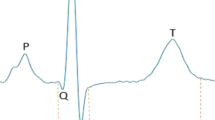
Psychotropic drugs can pose the risk of acquired long QT syndrome (LQTS). Unexpected autopsy-negative sudden death in patients taking psychotropic drugs may be associated with prolonged QT intervals and life-threatening arrhythmias. We analyzed genes that encode for cardiac ion channels and potentially associated with LQTS, examining specifically the potassium channel genes KCNQ1 and KCNH2 in 10 cases of sudden death involving patients administered psychotropic medication in which autopsy findings identified no clear cause of death. We amplified and sequenced all exons of KCNQ1 and KCNH2, identifying G643S, missense polymorphism in KCNQ1, in 6 of the 10 cases. A study analysis indicated that only 11% of 381 healthy Japanese individuals carry this polymorphism. Reports of previous functional analyses indicate that the G643S polymorphism in the KCNQ1 potassium channel protein causes mild IKs channel dysfunction. Our present study suggests that administering psychotropic drug therapy to individuals carrying the G643S polymorphism may heighten the risk of prolonged QT intervals and life-threatening arrhythmias. Thus, screening for the G643S polymorphism before prescribing psychotropic drugs may help reduce the risk of unexpected sudden death.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Accession codes
References
Harris, E. C. & Barraclough, B. Excess mortality of mental disorder. Br. J. Psychiatry 173, 11–53 (1998).
Raedler, T. J. Cardiovascular aspects of antipsychotics. Curr. Opin. Psychiatry 23, 574–581 (2010).
Timour, Q., Frassati, D., Descotes, J., Chevalier, P., Christé, G. & Chahine, M. Sudden death of cardiac origin and psychotropic drugs. Front. Pharmacol. 3, 1–9 (2012).
Haddad, P. M. & Anderson, I. M. Antipsychotic-related QTc prolongation, Torsade de pointes and sudden death. Drugs 62, 1649–1671 (2002).
Kongsamut, S., Kang, J., Chen, X. L., Roehr, J. & Rampe, D. A comparison of the receptor binding and HERG channel affinities for a series of antipsychotic drugs. Eur. J. Pharmacol. 450, 37–41 (2002).
Killeen, M. J. Antipsychotic-induced sudden cardiac death: examination of an atypical reaction. Expert Opin. Drug Saf. 8, 249–252 (2009).
Ray, W. A., Chung, C. P., Murray, K. T., Hall, K. & Stein, C. M. Atypical antipsychotic drugs and the risk of sudden cardiac death. N. Engl. J. Med. 360, 225–235 (2009).
Ramos-Ríos, R., Arrojo-Romero, M., Paz-Silva, E., Carballal-Calvo, F., Bouzón-Barreiro, J. L., Seoane-Prado, J. et al. QTc interval in a sample of long-term schizophrenia inpatients. Schizophr. Res. 116, 35–43 (2010).
Alvarez, P. A. & Pahissa, J. QT alterations in psychopharmacology: proven candidates and suspects. Curr. Drug Saf. 5, 97–104 (2010).
Lazarczyk, M. J., Bhuiyan, Z. A., Perrin, N. & Giannakopoulos, P. Selective acquired long QT syndrome (saLQTS) upon riperodone treatment. BMC Psychiatry 12, 220 (2012).
Raymond, L. A trusted partner providing reliable information on medicines http://www.azcert.org/ (25 May 2013).
Ozeki, Y., Fujii, K., Kurimoto, N., Yamada, N., Okawa, M., Aoki, T. et al. QTc prolongation and antipsychotic medications in sample of 1017 patients with schizophrenia. Prog. Neuropsychopharmacol. Biol. Psychiatry 34, 401–405 (2010).
Mahida, S., Hogarth, A. J., Cowan, C., Tayebjee, M. H., Graham, L. N. & Pepper, C. B. Genetics of congenital and drug-induced long QT syndromes: currents evidence and future research perspectives. J. Interv. Card. Electrophysiol. 37, 9–19 (2013).
Priori, S. G., Napolitano, C. & Schwartz, P. J. Low penetrance in the long-QT syndrome: clinical impact. Circulation 99, 529–533 (1999).
Brugada, R. Sudden death: managing the family, the role of genetics. Heart 97, 676–681 (2011).
Splawski, I., Shen, J., Timothy, K. W., Vincent, G. M., Lehmann, M. H. & Keating, M. T. Genomics structure of three long QT syndrome genes: KVLQT1, HERG, and KCNE1. Genomics 51, 86–97 (1998).
Jongbloed, R., Marcelis, C., Velter, C., Doevendans, P., Geraedts, J. & Smeets, H. DHPLC analysis of potassium ion channel genes in congenital long QT syndrome. Hum. Mutat. 20, 382–391 (2002).
Itoh, T., Tanaka, T., Nagai, R., Kamiya, T., Sawayama, T., Nakayama, T. et al. Genomic organization and mutational analysis of HERG, a gene responsible for familial long QT syndrome. Hum. Genet. 102, 435–439 (1998).
Hecker, K. H. & Roux, K. H. High and low annealing temperatures increase of both specificity and yield in touchdown and stepdown PCR. Biotechniques 20, 478–485 (1996).
Ozawa, T., Ito, M., Tamaki, S., Yao, T., Ashihara, T., Kita, Y. et al. Gender and age effects on ventricular repolarization abnormality in Japanese general carriers of a G643S common single nucleotide polymorphism for the KCNQ1 gene. Circ. J. 70, 645–650 (2006).
Bezzina, C. R., Verkerk, A. O, Busjahn, A., Jeron, A., Erdmann, J., Koopmann, T. T. et al. A common polymorphism in KCNH2(HERG) hastens cardiac repolarization. Cardiovasc. Res. 59, 27–36 (2003).
Hennessy, S., Bilker, W. B., Knauss, J. S., Margolis, D. J., Kimmel, S.E., Reynolds, R. F. et al. Cardiac arrest and ventricular arrhythmia in patients taking antipsychotic drugs: cohort study using administrative data. BMJ 325, 1070 (2002).
Ray, W. A., Meredith, S., Thapa, P. B., Meador, K.G., Hall, K. & Murray, K. T. Antipsychotics and the risk of sudden cardiac death. Arch. Gen. Psychiatry 58, 1161–1167 (2001).
Justo, D., Prokhorov, V., Heller, K. & Zeltser, D. Torsade de pointes induced by psychotropic drugs and the prevalence of its risk factors. Acta. Psychiatr. Scand. 111, 171–176 (2005).
Paulussen, A. D., Gilissen, R. A., Armstrong, M., Doevendans, P.A., Verhasselt, P., Smeets, H. J. et al. Genetic variations of KCNQ1, KCNH2, SCN5A, KCNE1, and KCNE2 in drug-induced long QT syndrome patients. J. Mol. Med. 82, 182–188 (2004).
Roden, D. M. & Viswanathan, P. C. Genetics of acquired long QT syndrome. J. Clin. Invest. 115, 2025–2032 (2005).
Michelsen, J.W. & Meyer, J.M. Cardiovascular effects of antipsychotics. Expert Rev. Neurother. 7, 829–839 (2007).
Sharma, D., Glatter, K. A., Timofeyev, V., Tuteja, D., Zhang, Z., Rodriguez, J. et al. Characterization of a KCNQ1/KVLQT1 polymorphism in Asia families with LQT2: implications for genetic testing. J. Mol. Cell. Cardiol. 37, 79–89 (2004).
Ackerman, M. J., Tester, D. J, Jones, G. S, Will, M. L., Burrow, C. R & Curran, M. E. Ethnic differences in cardiac potassium channel variants: implications for genetic susceptibility to sudden cardiac death and genetic testing for congenital long QT syndrome. Mayo Clin. Proc. 78, 1479–1487 (2003).
Kubota, T., Horie, M., Takano, M., Yoshida, H., Takenaka, K., Watanabe, E. et al. Evidence for a single nucleotide polymorphism in the KCNQ1 potassium channel that underlies susceptibility to life-threatening arrhythmias. J. Cardiovasc. Electrophysiol. 12, 1223–1229 (2001).
Pietilä, E., Fodstad, H., Niskasaari, E., Laitinen, P. PJ., Swan, H., Savolainen, M. et al. Association between HERG K897T polymorphism and QT interval in middle-age Finnish women. J. Am. Cell Cardiol. 40, 511–514 (2002).
Crotti, L., Lundquist, A. L., Insolia, R., Pedrazzini, M., Ferrandi, C., De Ferrari, G. M. et al. KCNH2-K897T is a genetic modifier of latent congenital long-QT syndrome. Circulation 112, 1251–1258 (2005).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kamei, S., Sato, N., Harayama, Y. et al. Molecular analysis of potassium ion channel genes in sudden death cases among patients administered psychotropic drug therapy: are polymorphisms in LQT genes a potential risk factor?. J Hum Genet 59, 95–99 (2014). https://doi.org/10.1038/jhg.2013.125
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/jhg.2013.125
Keywords
This article is cited by
-
Relationship between KCNQ1 (LQT1) and KCNH2 (LQT2) gene mutations and sudden death during illegal drug use
Scientific Reports (2018)
-
Drug-induced proarrhythmia: risk factors and electrophysiological mechanisms
Nature Reviews Cardiology (2016)
-
A variation in KCNQ1 gene is associated with repaglinide efficacy on insulin resistance in Chinese Type 2 Diabetes Mellitus Patients
Scientific Reports (2016)