Abstract
Objective:
The objective of this study was to evaluate the effectiveness of rescue oral acetaminophen in improving echocardiography (echo) indices of patent ductus arteriosus (PDA) shunt volume and avoiding surgical ligation in extremely low gestational age (GA) neonates (ELGANs, <28 weeks) with persistent PDA.
Study Design:
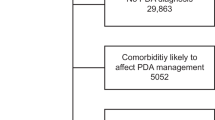
Retrospective cohort study of ELGANs with moderate or severe PDA at risk for ligation after a practice change introducing oral acetaminophen (60 mg kg−1 day−1 for 3 to 7 days) to facilitate ductal constriction after indomethacin failure.
Results:
Twenty-six infants (median GA 24.4 weeks at birth) with persistent PDA under consideration for surgical ligation were treated with oral acetaminophen at a mean of 27 days of life. Echo indices of shunt volume improved in 12 (46%) infants (3 closed and 9 reduced to mild shunt), all of whom avoided ligation. There was no echo improvement in 14 (54%) infants, of which 8/14 underwent ligation, and ligation was deferred in 6/14 infants, mostly owing to improvement in respiratory stability. Fewer responders than non-responders underwent ligation (0% vs 57%, P<0.01), though there were no differences in other neonatal outcomes.
Conclusions:
In ELGANs with persistent significant PDA, rescue therapy with oral acetaminophen was associated with improvement in echo indices of shunt volume and avoidance of ligation in nearly half of infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Kabra NS, Schmidt B, Roberts RS, Doyle LW, Papile L, Fanaroff A et al. Neurosensory impairment after surgical closure of patent ductus arteriosus in extremely low birth weight infants: results from the Trial of Indomethacin Prophylaxis in Preterms. J Pediatr 2007; 150 (3): 229–234, e221.
Madan JC, Kendrick D, Hagadorn JI, Frantz IID . Patent ductus arteriosus therapy: Impact on neonatal and 18-month outcome. Pediatrics 2009; 123 (2): 674–681.
Weisz DE, More K, McNamara PJ, Shah PS . PDA ligation and health outcomes: a meta-analysis. Pediatrics 2014; 133 (4): e1024–e1046.
Morriss FH Jr, Saha S, Bell EF, Colaizy TT, Stoll BJ, Hintz SR et al. Surgery and neurodevelopmental outcome of very low-birth-weight infants. JAMA Pediatr 2014; 168 (8): 746–754.
Wickremasinghe AC, Rogers EE, Piecuch RE, Johnson BC, Golden S, Moon-Grady AJ et al. Neurodevelopmental outcomes following two different treatment approaches (early ligation and selective ligation) for patent ductus arteriosus. J Pediatr 2012; 161 (6): 1065–1072.
Shah P, Mirea L, Weisz D, Barrington K, Lee K, Sorokan T et al. Trends in patent ductus arteriosus management and association with neonatal mortality and morbidities among very preterm infants in Canada. E-PAS 2014; 2850: 8.
Bose CL, Laughon MM . Patent ductus arteriosus: lack of evidence for common treatments. Arch Dis Child Fetal Neonatal Ed 2007; 92 (6): F498–F502.
Noori S, McCoy M, Friedlich P, Bright B, Gottipati V, Seri I et al. Failure of ductus arteriosus closure is associated with increased mortality in preterm infants. Pediatrics 2009; 123 (1): e138–e144.
Kaempf JW, Wu YX, Kaempf AJ, Kaempf AM, Wang L, Grunkemeier G . What happens when the patent ductus arteriosus is treated less aggressively in very low birth weight infants? J Perinatol 2012; 32 (5): 344–348.
Schena F, Francescato G, Cappelleri A, Picciolli I, Mayer A, Mosca F et al. Association between hemodynamically significant patent ductus arteriosus and bronchopulmonary dysplasia. J Pediatr 2015; 166 (6): 1488–1492.
Dang D, Wang D, Zhang C, Zhou W, Zhou Q, Wu H . Comparison of oral paracetamol versus ibuprofen in premature infants with patent ductus arteriosus: a randomized controlled trial. PLoS One 2013; 8 (11): e77888.
Oncel MY, Yurttutan S, Erdeve O, Uras N, Altug N, Oguz SS et al. Oral paracetamol versus oral ibuprofen in the management of patent ductus arteriosus in preterm infants: a randomized controlled trial. J Pediatr 2014; 164 (3): 510–514 e511.
Roofthooft DW, van Beynum IM, Helbing WA, Reiss IK, Simons SH . Paracetamol for ductus arteriosus closure: not always a success story. Neonatology 2013; 104 (3): 170.
Ozdemir OM, Dogan M, Kucuktasci K, Ergin H, Sahin O . Paracetamol therapy for patent ductus arteriosus in premature infants: a chance before surgical ligation. Pediatr Cardiol 2014; 35 (2): 276–279.
El-Khuffash A, Jain A, Corcoran D, Shah PS, Hooper CW, Brown N et al. Efficacy of paracetamol on patent ductus arteriosus closure may be dose dependent: evidence from human and murine studies. Pediatr Res 2014; 76 (3): 238–244.
Fajardo MF, Claure N, Swaminathan S, Sattar S, Vasquez A, D'Ugard C et al. Effect of positive end-expiratory pressure on ductal shunting and systemic blood flow in preterm infants with patent ductus arteriosus. Neonatology 2014; 105 (1): 9–13.
De Buyst J, Rakza T, Pennaforte T, Johansson AB, Storme L . Hemodynamic effects of fluid restriction in preterm infants with significant patent ductus arteriosus. J Pediatr 2012; 161 (3): 404–408.
El-Khuffash AF, Jain A, McNamara PJ . Ligation of the patent ductus arteriosus in preterm infants: Understanding the physiology. J Pediatr 2013; 162 (6): 1100–1106.
Hammerman C, Bin-Nun A, Markovitch E, Schimmel MS, Kaplan M, Fink D . Ductal closure with paracetamol: a surprising new approach to patent ductus arteriosus treatment. Pediatrics 2011; 128 (6): e1618–e1621.
Oncel MY, Yurttutan S, Uras N, Altug N, Ozdemir R, Ekmen S et al. An alternative drug (paracetamol) in the management of patent ductus arteriosus in ibuprofen-resistant or contraindicated preterm infants. Arch Dis Child Fetal Neonatal Ed 2013; 98 (1): F94.
Kessel I, Waisman D, Lavie-Nevo K, Golzman M, Lorber A, Rotschild A . Paracetamol effectiveness, safety and blood level monitoring during patent ductus arteriosus closure: a case series. J Matern Fetal Neonatal Med 2014; 27 (16): 1719–1721.
Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg 1978; 187 (1): 1–7.
Smith A, Maguire M, Livingstone V, Dempsey EM . Peak systolic to end diastolic flow velocity ratio is associated with ductal patency in infants below 32 weeks of gestation. Arch Dis Child Fetal Neonatal Ed 2015; 100 (2): F132–F136.
Jasani B, Kabra N, Nanavati RN . Oral paracetamol in treatment of closure of patent ductus arteriosus in preterm neonates. J Postgrad Med 2013; 59 (4): 312–314.
El-Khuffash A, James AT, Cleary A, Semberova J, Franklin O, Miletin J . Late medical therapy of patent ductus arteriosus using intravenous paracetamol. Arch Dis Child Fetal Neonatal Ed 2015; 100 (3): F253–F256.
Allegaert K, Anderson B, Simons S, van Overmeire B . Paracetamol to induce ductus arteriosus closure: is it valid? Arch Dis Child 2013; 98 (6): 462–466.
Anderson BJ . Paracetamol (Acetaminophen): mechanisms of action. Paediatr Anaesth 2008; 18 (10): 915–921.
Rolland A, Shankar-Aguilera S, Diomande D, Zupan-Simunek V, Boileau P . Natural evolution of patent ductus arteriosus in the extremely preterm infant. Arch Dis Child Fetal Neonatal Ed 2015; 100 (1): F55–F58.
El-Khuffash A, James AT, Corcoran JD, Dicker P, Franklin O, Elsayed YN et al. A patent ductus arteriosus severity score predicts chronic lung disease or death before discharge. J Pediatr 2015; 167: 1354–1361.e2.
Sehgal A, Paul E, Menahem S . Functional echocardiography in staging for ductal disease severity: role in predicting outcomes. Eur J Pediatr 2013; 172 (2): 179–184.
El-Khuffash AF, Slevin M, McNamara PJ, Molloy EJ . Troponin T, N-terminal pro natriuretic peptide and a patent ductus arteriosus scoring system predict death before discharge or neurodevelopmental outcome at 2 years in preterm infants. Arch Dis Child Fetal Neonatal Ed 2011; 96 (2): F133–F137.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Weisz, D., Martins, F., Nield, L. et al. Acetaminophen to avoid surgical ligation in extremely low gestational age neonates with persistent hemodynamically significant patent ductus arteriosus. J Perinatol 36, 649–653 (2016). https://doi.org/10.1038/jp.2016.60
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/jp.2016.60
This article is cited by
-
Clinical and echocardiography predictors of response to first-line acetaminophen treatment in preterm infants with hemodynamically significant patent ductus arteriosus
Journal of Perinatology (2024)
-
Is late treatment with acetaminophen safe and effective in avoiding surgical ligation among extremely preterm neonates with persistent patent ductus arteriosus?
Journal of Perinatology (2021)
-
Oral Paracetamol for Patent Ductus Arteriosus Rescue Closure
Pediatric Cardiology (2018)