Abstract
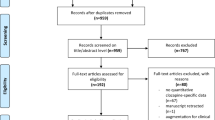
Memantine, an uncompetitive antagonist of glutamate receptors of the N-methyl-D-aspartate type is approved for the treatment of moderate to severe Alzheimer's disease. A growing body of evidence supports a link between the glutamatergic neurotransmission and schizophrenia. The purpose of this study (MEM-MD-29) was to examine the efficacy and safety of memantine as an adjunctive treatment to atypical antipsychotics in patients with persistent residual psychopathology of schizophrenia. In this double-blind, placebo-controlled study, participants were assigned to receive 20 mg/day memantine (n=70) or placebo (n=68), in addition to continuing treatment with atypical antipsychotics, for 8 weeks. The primary efficacy measure was the total score on the Positive and Negative Symptom Scale (PANSS). Secondary measures were positive and negative PANSS scores, PANSS responders, Calgary Depression Scale for Schizophrenia (CDSS), Clinical Global Impression of Severity (CGI-S), Clinical Global Impression of Improvement (CGI-I), and Brief Assessment of Cognition in Schizophrenia (BACS). Missing data were imputed using the last observation carried forward (LOCF) approach. Safety was assessed by means of physical examination, clinical laboratory evaluation, recording of adverse events (AEs), and measures of extrapyramidal symptoms. At end point, total PANSS scores did not differ between the memantine and the placebo group (p=0.570, LOCF). A similar outcome was observed for all secondary measures. The frequency of serious AEs in the memantine vs placebo group was 8.7 vs 6.0%; treatment discontinuations because of AEs occurred in 11.6 and 3.0% of patients in these groups, respectively. Memantine showed no efficacy as an adjunctive therapy in schizophrenia patients with residual psychopathology and was associated with a higher incidence of AEs than placebo.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Addington D, Addington J, Atkinson M (1996). A psychometric comparison of the Calgary Depression Scale for Schizophrenia and the Hamilton Depression Rating Scale. Schizophr Res 19: 205–212.
APA (2000). DSM-IV-TR: Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Press: Washington, DC.
Bell MD, Lysaker PH, Milstein RM, Beam-Goulet JL (1994). Concurrent validity of the cognitive component of schizophrenia: relationship of PANSS scores to neuropsychological assessments. Psychiatry Res 54: 51–58.
Bressan RA, Pilowsky LS (2000). Imaging the glutamatergic system in vivo—relevance to schizophrenia. Eur J Nucl Med 27: 1723–1731.
Buchanan RW, Javitt DC, Marder SR, Schooler NR, Gold JM, McMahon RP et al (2007). The Cognitive and Negative Symptoms in Schizophrenia Trial (CONSIST): the efficacy of glutamatergic agents for negative symptoms and cognitive impairments. Am J Psychiatry 164: 1593–1602.
Buckley PF, Shendarkar N (2005). Treatment-refractory schizophrenia. Curr Opin Psychiatry 18: 165–173.
Carlsson A, Waters N, Waters S, Carlsson ML (2000). Network interactions in schizophrenia—therapeutic implications. Brain Res Brain Res Rev 31: 342–349.
Carpenter WT, Buchanan RW, Javitt DC, Marder SR, Schooler NR, Heresco-Levy U et al (2005). Testing two efficacy hypotheses for the treatment of negative symptoms. Schizophr Bull 20th International Congress on Schizophrenia Research, Savannah, GA.
Casey DE, Daniel DG, Wassef AA, Tracy KA, Wozniak P, Sommerville KW (2003). Effect of divalproex combined with olanzapine or risperidone in patients with an acute exacerbation of schizophrenia. Neuropsychopharmacology 28: 182–192.
Chakos MH, Glick ID, Miller AL, Hamner MB, Miller del D, Patel JK et al (2006). Baseline use of concomitant psychotropic medications to treat schizophrenia in the CATIE trial. Psychiatr Serv 57: 1094–1101.
Coyle JT, Tsai G, Goff DC (2002). Ionotropic glutamate receptors as therapeutic targets in schizophrenia. Curr Drug Targets CNS Neurol Disord 1: 183–189.
Deakin JF, Simpson MD (1997). A two-process theory of schizophrenia: evidence from studies in post-mortem brain. J Psychiatr Res 31: 277–295.
Egerton A, Reid L, McKerchar CE, Morris BJ, Pratt JA (2005). Impairment in perceptual attentional set-shifting following PCP administration: a rodent model of set-shifting deficits in schizophrenia. Psychopharmacology (Berl) 179: 77–84.
Ferguson JM, Shingleton RN (2007). An open-label, flexible-dose study of memantine in major depressive disorder. Clin Neuropharmacol 30: 136–144.
Goff DC, Keefe RS, Volavka J, Krystal JH, Davy K, Thompson TR et al (2006). Lamotrigine added to atypical antipsychotics for treatment of schizophrenia: results of two double-blind randomized clinical trials. Am Psychiatr Assoc 159th Annual Meeting, Toronto, ON.
Guy W (1976). ECDEU Assessment Manual for Psychopharmacology. In: Superintendent of Documents, U.S. Government Printing Office, U.S. Department of Health, Education, and Welfare Publication No. 76-338: Washington, DC.
Heresco-Levy U, Javitt DC, Ebstein R, Vass A, Lichtenberg P, Bar G et al (2005). D-Serine efficacy as add-on pharmacotherapy to risperidone and olanzapine for treatment-refractory schizophrenia. Biol Psychiatry 57: 577–585.
Homayoun H, Moghaddam B (2007). NMDA receptor hypofunction produces opposite effects on prefrontal cortex interneurons and pyramidal neurons. J Neurosci 27: 11496–11500.
Honer WG, Thornton AE, Chen EY, Chan RC, Wong JO, Bergmann A et al (2006). Clozapine alone versus clozapine and risperidone with refractory schizophrenia. N Engl J Med 354: 472–482.
Javitt DC, Zukin SR (1991). Recent advances in the phencyclidine model of schizophrenia. Am J Psychiatry 148: 1301–1308.
Jones RW, Bayer A, Inglis F, Barker A, Phul R (2007). Safety and tolerability of once-daily versus twice-daily memantine: a randomised, double-blind study in moderate to severe Alzheimer's disease. Int J Geriatr Psychiatry 22: 258–262.
Kay SR, Fiszbein A, Opler LA (1987). The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull 13: 261–276.
Keefe RS, Goldberg TE, Harvey PD, Gold JM, Poe MP, Coughenour L (2004). The Brief Assessment of Cognition in Schizophrenia: reliability, sensitivity, and comparison with a standard neurocognitive battery. Schizophr Res 68: 283–297.
Keefe RS, Poe M, Walker TM, Harvey PD (2006). The relationship of the Brief Assessment of Cognition in Schizophrenia (BACS) to functional capacity and real-world functional outcome. J Clin Exp Neuropsychol 28: 260–269.
Kraus MS, Keefe RS (2007). Cognition as an outcome measure in schizophrenia. Br J Psychiatry Suppl 50: s46–s51.
Kreyenbuhl J, Valenstein M, McCarthy JF, Ganoczy D, Blow FC (2006). Long-term combination antipsychotic treatment in VA patients with schizophrenia. Schizophr Res 84: 90–99.
Krystal JH, Belger A, Abi-Saab W, Moghaddam B, Charney DS, Anand A et al (2000). Glutamatergic contributions to cogntive disfunction in schizophrenia. In: Harvey PD, Sharma T (eds). Cognition in Schizophrenia: Impairments, Importance and Treatment Strategies. Oxford University Press: London. pp 126–155.
Kurtz MM (2005). Neurocognitive impairment across the lifespan in schizophrenia: an update. Schizophr Res 74: 15–26.
Lane HY, Chang YC, Liu YC, Chiu CC, Tsai GE (2005). Sarcosine or D-serine add-on treatment for acute exacerbation of schizophrenia: a randomized, double-blind, placebo-controlled study. Arch Gen Psychiatry 62: 1196–1204.
Maccaferri G, Dingledine R (2002). Control of feedforward dendritic inhibition by NMDA receptor-dependent spike timing in hippocampal interneurons. J Neurosci 22: 5462–5472.
McShane R, Areosa Sastre A, Minakaran N (2006). Memantine for dementia. Cochrane Database Syst Rev: CD003154.
Messer T, Tiltscher C, Schmauss M (2006). [Polypharmacy in the treatment of schizophrenia]. Fortschr Neurol Psychiatr 74: 377–391.
Moghaddam B, Adams B, Verma A, Daly D (1997). Activation of glutamatergic neurotransmission by ketamine: a novel step in the pathway from NMDA receptor blockade to dopaminergic and cognitive disruptions associated with the prefrontal cortex. J Neurosci 17: 2921–2927.
Parsons CG, Stoffler A, Danysz W (2007). Memantine: a NMDA receptor antagonist that improves memory by restoration of homeostasis in the glutamatergic system—too little activation is bad, too much is even worse. Neuropharmacology 53: 699–723.
Patil ST, Zhang L, Martenyi F, Lowe SL, Jackson KA, Andreev BV et al (2007). Activation of mGlu2/3 receptors as a new approach to treat schizophrenia: a randomized Phase 2 clinical trial. Nat Med 13: 1102–1107.
Peskind ER, Potkin SG, Pomara N, Ott BR, Graham SM, Olin JT et al (2006). Memantine treatment in mild to moderate Alzheimer disease: A 24-week, randomized, controlled trial. Am J Geriatr Psychiatry 14: 704–715.
Rammsayer TH (2001). Effects of pharmacologically induced changes in NMDA-receptor activity on long-term memory in humans. Learn Mem 8: 20–25.
Reisberg B, Doody R, Stoffler A, Schmitt F, Ferris S, Mobius HJ (2003). Memantine in moderate-to-severe Alzheimer's disease. N Engl J Med 348: 1333–1341.
Riedel M, Strassnig M, Schwarz MJ, Muller N (2005). COX-2 inhibitors as adjunctive therapy in schizophrenia: rationale for use and evidence to date. CNS Drugs 19: 805–819.
Stahl SM, Grady MM (2004). A critical review of atypical antipsychotic utilization: comparing monotherapy with polypharmacy and augmentation. Curr Med Chem 11: 313–327.
Tariot PN, Farlow MR, Grossberg GT, Graham SM, McDonald S, Gergel I (2004). Memantine treatment in patients with moderate to severe Alzheimer disease already receiving donepezil: a randomized controlled trial. JAMA 291: 317–324.
Tsai G, Coyle JT (2002). Glutamatergic mechanisms in schizophrenia. Annu Rev Pharmacol Toxicol 42: 165–179.
Tuominen H, Tiihonen J, Wahlbeck K (2006). Glutamatergic drugs for schizophrenia. Cochrane Database Syst Rev: CD003730.
Waheed W, Hussain MZ, Hussain S (2006). Memantine in the treatment of schizophrenic cognitive impairment. Am Psychiatr Assoc 159th Annual Meeting, Toronto, Canada.
Winblad B, Poritis N (1999). Memantine in severe dementia: results of the 9M-Best Study (Benefit and efficacy in severely demented patients during treatment with memantine). Int J Geriatr Psychiatry 14: 135–146.
Yang CR, Chen L (2005). Targeting prefrontal cortical dopamine D1 and N-methyl-D-aspartate receptor interactions in schizophrenia treatment. Neuroscientist 11: 452–470.
Zink M, Henn FA, Thome J (2004). Combination of amisulpride and olanzapine in treatment-resistant schizophrenic psychoses. Eur Psychiatry 19: 56–58.
Acknowledgements
Forest Laboratories Inc. provided funding and statistical support for this study. We acknowledge Vojislav Pejovic, PhD and Michael L. Miller, PhD from Prescott Medical Communications Group for medical writing and editorial support.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Previous presentation: None.
Location of work: This trial has been conducted in the following US sites: Dartmouth Hitchcock Medical Center, Department of Psychiatry, Lebanon, NH; Metropolitan Psychiatric Center, St Louis, MO; VA San Diego Healthcare System, San Diego, CA; Duke University, John Umstead Hospital, Butner, NC; Medication Research Clinic, San Antonio, TX; University of Iowa, Psychiatric Research, Iowa City, IA; University of Cincinnati, Cincinnati, OH; UNC Chapel Hill, Clinical Research Unit, Raleigh, NC; University of Miami, Jackson Memorial Hospital, Mental Health Hospital Center, Miami, FL; Nathan Kline Institute, Psychiatric Research Department, Orangeburg, NY; Synergy Clinical Research, National City, CA; University Hills Clinical Research, Irving, TX; CBH Health, LLC, Rockville, MD.
Members of the MEM-MD-29 study group included
Alan Green, MD, Dartmouth Hitchcock Medical School, Lebanon, NH; John Csernansky, MD, Metropolitan Psychiatric Center, St. Louis, MO; Hua Jin, MD, VA San Diego Healthcare System, San Diego, CA; Joseph McEvoy, MD, Duke University, John Umstead Hospital, Butner, NC; Alexander Miller, MD, Medication Research Clinic, San Antonio, TX; Del Miller, MD, University of Iowa, Iowa City, IA; Henry Nasrallah, MD, MA, University of Cincinnati, Cincinnati, OH; Olgierd Pucilowski, MD, PhD, University of North Carolina—Chapel Hill, Raleigh, NC; Richard Steinbook, MD, University of Miami, Jackson Memorial Hospital, Miami, FL; Jan Volavka, MD, Nathan Kline Institute, Orangeburg, NY; Mohammed A. Bari, MD, Synergy Clinical Research, National City, CA; Mary Ann Knesevich, MD, University Hills Clinical Research, Irving, TX; Robert E. Litman, MD, CBH Health, LLC, Rockville, MD.
DISCLOSURE/CONFLICT OF INTEREST
Jeffrey Lieberman serves as a consultant and/or advisor for Astra Zeneca, Eli Lilly, Forest Laboratories, GlaxoSmithKline, Pfizer and Wyeth; and as a member of the Data Safety Management Board (DSMB) for Solvay and Wyeth. He does not receive financial compensation or salary support for his participation as a consultant or as a member of a board. He receives grant support from AstraZeneca, Bristol-Myers Squibb, GlaxoSmithKline, Janssen, Merck, Pfizer and Wyeth; and he holds a patent from Repligen.
Allyson Gage, Kelly Papadakis, and Xinwei Daniel Jia are employees of Forest Laboratories Inc.
John Csernansky has received research grants from the NIMH, NIA, and the Schizophrenia Trials Network (University of North Carolina). In addition, he has been a consultant for Sanofi-Aventis, Eli Lilly, Solvay, and Wyeth Pharmaceuticals, and has received honoraria for lectures from Eli Lilly and Janssen Pharmaceuticals.
Robert Litman has been a consultant for Dainippon-Sumitomo, and an Independent Contractor (Principal Investigator) for clinical trial contracts through CBH Health, LLC, with the following sponsors: AstraZeneca, Sanofi-Aventis, Johnson & Johnson Pharmaceutical Research and Development LLC, Forest Research Institute, Wyeth, Vanda Pharmaceuticals, Mutual Pharmaceuticals.
Jan Volavka has received travel funds from Eli Lilly & Company.
This study was designed, financed, and analyzed by Forest Laboratories Inc.
Rights and permissions
About this article
Cite this article
Lieberman, J., Papadakis, K., Csernansky, J. et al. A Randomized, Placebo-Controlled Study of Memantine as Adjunctive Treatment in Patients with Schizophrenia. Neuropsychopharmacol 34, 1322–1329 (2009). https://doi.org/10.1038/npp.2008.200
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/npp.2008.200
Keywords
This article is cited by
-
Cognitive impairment in schizophrenia: aetiology, pathophysiology, and treatment
Molecular Psychiatry (2023)
-
Schizophrenia, Curcumin and Minimizing Side Effects of Antipsychotic Drugs: Possible Mechanisms
Neurochemical Research (2023)
-
Glutamatergic dysfunction in Schizophrenia
Translational Psychiatry (2022)
-
Non-invasive brain stimulation modulates GABAergic activity in neurofibromatosis 1
Scientific Reports (2022)
-
Memantine in neurological disorders – schizophrenia and depression
Journal of Molecular Medicine (2021)