Abstract
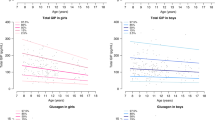
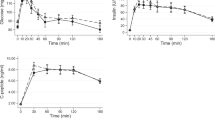
Most studies of insulin sensitivity in puberty have been cross-sectional and have not been able to longitudinally address changes that might occur. In addition, these studies were unable to separate out glucose's ability to stimulate its own disposal (glucose effectiveness, SG) from insulin sensitivity (SI) or to separate the hepatic and peripheral effects of insulin. To address these problems, we used the frequently sampled i.v. glucose tolerance test with [6,6]D2 glucose to study SG* and SI* in 24 children (Tanner stage 1–3) at 6-mo intervals over an 18-mo period. Mean overnight GH and fasting GH binding protein (GHBP), IGF-1, and leptin levels were also measured. SG* did not differ between the sexes or Tanner stages. SI* did not differ between Tanner stages for either sex and was higher in boys than in girls. Hepatic insulin resistance did not differ between sexes or Tanner stages. SG* was not related to any of the other variables measured. SI* was negatively related to BMI, GHBP, IGF1, and leptin. These results demonstrate that insulin sensitivity is greater in prepubertal and early pubertal boys than in girls and is primarily determined by body mass effects.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Abbreviations
- BMI:
-
body mass index
- GHBP:
-
GH binding protein
- IGF1:
-
insulin-like growth factor 1
- SG:
-
glucose effectiveness
- SG * :
-
glucose effectiveness determined from labeled glucose and one compartment minimal model
- SI:
-
insulin sensitivity
- SI * :
-
insulin sensitivity determined from labeled glucose and one compartment minimal model
References
Amiel SA, Sherwin RS, Simonson DC, Lauritano AA, Tamborlane WV 1986 Impaired insulin action in puberty: a contributing factor to poor glycemic control in adolescents with diabetes. N Engl J Med 315: 215–219.
Bloch CA, Clemons P, Sperling MA 1987 Puberty decreases insulin sensitivity. J Pediatr 110: 481–487.
Caprio S, Plewe G, Diamond MP, Simonson DC, Boulware S, Sherwin RS, Tamborlane WV 1989 Increased insulin secretion in puberty: a compensatory response to reductions in insulin sensitivity. J Pediatr 114: 963–967.
Cutfield WS, Bergman RN, Menon RK, Sperling MA 1990 The modified minimal model: application to measurement of insulin sensitivity in children. J Clin Endocrinol Metab 70: 1644–1650.
Amiel SA, Caprio Sherwin RS, Plewe G, Haymond MW, Tamborlane WV 1991 Insulin resistance of puberty: a defect restricted to peripheral glucose metabolism. J Clin Endocrinol Metab 72: 277–282.
Cook JS, Hoffman RP, Stene MA, Hansen JR 1993 Effects of maturational stage on insulin sensitivity during puberty. J Clin Endocrinol Metab 77: 725–730.
Travers SH, Jeffers BW, Bloch CA, Hill JO, Eckel RH 1995 Gender and Tanner stage differences in body composition and insulin sensitivity in early pubertal children. J Clin Endocrinol Metab 80: 172–178.
Arslanian S, Suprasongsin C 1996 Insulin sensitivity, lipids and body composition in childhood: is “Syndrome X” present?. J Clin Endocrinol Metab 81: 1058
Hoffman RP, Armstrong PT 1996 Glucose effectiveness, peripheral and hepatic insulin sensitivity, in obese and lean prepubertal children. Int J Obes 20: 521–525.
Ader M, Pacini G, Yang YJ, Bergman RN 1985 Importance of glucose per se to intravenous glucose tolerance: comparison of the minimal-model prediction with direct measurements. Diabetes 34: 1092–1103.
Avogaro A, Bristow JD, Bier DM, Cobelli C, Toffolo G 1989 Stable-label intravenous glucose tolerance test minimal model. Diabetes 38: 1048–1055.
Martha P, Rogol A, Blizzard R, Shaw M, Baumann G 1991 Growth hormone binding protein is inversely related to 24 hour growth hormone release in normal boys. J Clin Endocrinol Metab 73: 175–181.
Ahmed M, Ong KKL, Morell DJ, Cox L, Drayer N, Perry L, Preece MA, Dunger DB 1999 Longitudinal study of leptin concentrations during puberty: sex differences and relationship to changes in body composition. J Clin Endocrinol Metab 84: 899–905.
Steele R 1959 Use of C14-glucose to measure hepatic glucose production following an I. Metabolism 8: 512–519.
Arslanian SA, Heil BV, Becker DJ, Drash AL 1991 Sexual dimorphism in insulin sensitivity in adolescents with insulin dependent diabetes mellitus. J Clin Endocrinol Metab 72: 920–926.
Acknowledgements
The authors thank the nurses of the CRC for their assistance in care for the subjects, Dennis Charkowski, and Yalan Li for measurement of [6,6]D2 glucose and especially Nandhini Subbiah for her measurement of plasma glucose levels, computer data entry, and organizational abilities. We also thank Drs. Eva Tsalikian and Patricia Donohoue who helped by Tanner staging the female subjects.
Author information
Authors and Affiliations
Additional information
This study was funded by a grant from the Genentech Foundation for Growth and Development and by the General Clinical Research Center of the University of Iowa (RR59).
Rights and permissions
About this article
Cite this article
Hoffman, R., Vicini, P., Sivitz, W. et al. Pubertal Adolescent Male-Female Differences in Insulin Sensitivity and Glucose Effectiveness Determined by the One Compartment Minimal Model. Pediatr Res 48, 384–388 (2000). https://doi.org/10.1203/00006450-200009000-00022
Received:
Accepted:
Issue date:
DOI: https://doi.org/10.1203/00006450-200009000-00022
This article is cited by
-
Do sex differences in paediatric type 1 diabetes care exist? A systematic review
Diabetologia (2023)
-
Glycemic control, depression, diabetes distress among adolescents with type 1 diabetes: effects of sex, race, insurance, and obesity
Acta Diabetologica (2021)
-
Nutritional Status of Pediatric Patients with Type 1 Diabetes Mellitus from Northeast Poland: A Case-Control Study
Diabetes Therapy (2021)
-
Insulin Resistance of Puberty
Current Diabetes Reports (2016)
-
Adiponectin/resistin levels and insulin resistance in children: a four country comparison study
International Journal of Pediatric Endocrinology (2015)