Abstract
Background:
Mutations in canonical transient receptor potential channel 6 (TRPC6) have been identified as responsible for the development of focal segmental glomerulosclerosis, a proteinuric disease with steroid resistance and poor prognosis. This study explores the prevalence of TRPC6 variants in Chinese children with idiopathic nephrotic syndrome (INS), the genotype/phenotype correlation of TRPC6 variants, the therapeutic response, and the underlying molecular mechanism.
Methods:
Fifty-one children with sporadic INS were enrolled: 23 steroid-sensitive cases and 28 steroid-resistant cases Polymerase chain reaction was used to amplify 13 exons and the promoter sequences of TRPC6 before sequencing. The expression of TRPC6 in renal tissues was illustrated by immunohistochemistry staining. The transcriptional activity of variants in TRPC6 promoter was measured by the luciferase assay.
Results:
Three variants (-254C>G, rs3824934; +43C/T, rs3802829; and 240 G>A, rs17096918) were identified. The allele frequency of the -254C>G single-nucleotide polymorphism (SNP) in the steroid-resistant nephrotic syndrome (SRNS) patients (40.5%) was higher than that in the steroid-sensitive nephrotic syndrome subjects (27.1%; P = 0.046). The -254C>G SNP enhanced transcription from TRPC6 promoter in vitro and was associated with increased TRPC6 expression in renal tissues of SRNS patients.
Conclusion:
-254C>G, a SNP underlying enhanced TRPC6 transcription and expression, may be correlated with the development of steroid resistance in Chinese children with INS.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Khurana M, Traum AZ, Aivado M, et al. Urine proteomic profiling of pediatric nephrotic syndrome. Pediatr Nephrol 2006;21:1257–65.
Kitiyakara C, Kopp JB, Eggers P . Trends in the epidemiology of focal segmental glomerulosclerosis. Semin Nephrol 2003;23:172–82.
Collins AJ, Foley RN, Chavers B, et al. United States Renal Data System 2011 Annual Data Report: Atlas of chronic kidney disease & end-stage renal disease in the United States. Am J Kidney Dis 2012; 59:A7, e1–e420.
Kitiyakara C, Eggers P, Kopp JB . Twenty-one-year trend in ESRD due to focal segmental glomerulosclerosis in the United States. Am J Kidney Dis 2004;44:815–25.
Ulinski T, Aoun B . Pediatric idiopathic nephrotic syndrome: treatment strategies in steroid dependent and steroid resistant forms. Curr Med Chem 2010;17:847–53.
McBryde KD, Kershaw DB, Smoyer WE . Pediatric steroid-resistant nephrotic syndrome. Curr Probl Pediatr Adolesc Health Care 2001;31:280–307.
Ehrich JH, Geerlings C, Zivicnjak M, Franke D, Geerlings H, Gellermann J . Steroid-resistant idiopathic childhood nephrosis: overdiagnosed and undertreated. Nephrol Dial Transplant 2007;22:2183–93.
Winn MP, Conlon PJ, Lynn KL, et al. A mutation in the TRPC6 cation channel causes familial focal segmental glomerulosclerosis. Science 2005;308:1801–4.
Machuca E, Benoit G, Antignac C . Genetics of nephrotic syndrome: connecting molecular genetics to podocyte physiology. Hum Mol Genet 2009;18(R2):R185–94.
Mukerji N, Damodaran TV, Winn MP . TRPC6 and FSGS: the latest TRP channelopathy. Biochim Biophys Acta 2007;1772:859–68.
Benoit G, Machuca E, Nevo F, Gribouval O, Lepage D, Antignac C . Analysis of recessive CD2AP and ACTN4 mutations in steroid-resistant nephrotic syndrome. Pediatr Nephrol 2010;25:445–51.
Antignac C . Molecular basis of steroid-resistant nephrotic syndrome. Nefrologia 2005;25 Suppl 2:25–8.
Reusz G, Szabó A, Fekete A . [Nephrotic syndrome in childhood]. Orv Hetil 2006;147:2251–60.
Reiser J, Polu KR, Möller CC, et al. TRPC6 is a glomerular slit diaphragm-associated channel required for normal renal function. Nat Genet 2005;37:739–44.
Santín S, Ars E, Rossetti S, et al.; FSGS Study Group. TRPC6 mutational analysis in a large cohort of patients with focal segmental glomerulosclerosis. Nephrol Dial Transplant 2009;24:3089–96.
Heeringa SF, Möller CC, Du J, et al. A novel TRPC6 mutation that causes childhood FSGS. PLoS ONE 2009;4:e7771.
Zhu B, Chen N, Wang ZH, et al. Identification and functional analysis of a novel TRPC6 mutation associated with late onset familial focal segmental glomerulosclerosis in Chinese patients. Mutat Res 2009;664:84–90.
Gigante M, Caridi G, Montemurno E, et al. TRPC6 mutations in children with steroid-resistant nephrotic syndrome and atypical phenotype. Clin J Am Soc Nephrol 2011;6:1626–34.
Schlöndorff J, Del Camino D, Carrasquillo R, Lacey V, Pollak MR . TRPC6 mutations associated with focal segmental glomerulosclerosis cause constitutive activation of NFAT-dependent transcription. Am J Physiol, Cell Physiol 2009;296:C558–69.
Kuwahara K, Wang Y, McAnally J, et al. TRPC6 fulfills a calcineurin signaling circuit during pathologic cardiac remodeling. J Clin Invest 2006;116:3114–26.
Yu Y, Keller SH, Remillard CV, et al. A functional single-nucleotide polymorphism in the TRPC6 gene promoter associated with idiopathic pulmonary arterial hypertension. Circulation 2009;119:2313–22.
Clapham DE . TRP channels as cellular sensors. Nature 2003;426:517–24.
Okada T, Inoue R, Yamazaki K, et al. Molecular and functional characterization of a novel mouse transient receptor potential protein homologue TRP7. Ca(2+)-permeable cation channel that is constitutively activated and enhanced by stimulation of G protein-coupled receptor. J Biol Chem 1999;274:27359–70.
Hofmann T, Obukhov AG, Schaefer M, Harteneck C, Gudermann T, Schultz G . Direct activation of human TRPC6 and TRPC3 channels by diacylglycerol. Nature 1999;397:259–63.
Krall P, Canales CP, Kairath P, et al. Podocyte-specific overexpression of wild type or mutant trpc6 in mice is sufficient to cause glomerular disease. PLoS ONE 2010;5:e12859.
Mir S, Yavascan O, Berdeli A, Sozeri B . TRPC6 gene variants in Turkish children with steroid-resistant nephrotic syndrome. Nephrol Dial Transplant 2012;27:205–9.
Cho MH, Hong EH, Lee TH, Ko CW . Pathophysiology of minimal change nephrotic syndrome and focal segmental glomerulosclerosis. Nephrology (Carlton) 2007;12 Suppl 3:S11–4.
Shankland SJ, Pippin JW, Reiser J, Mundel P . Podocytes in culture: past, present, and future. Kidney Int 2007;72:26–36.
Acknowledgements
We thank all the children who participated in the study. We also thank Xiao-Xin Xu (Xin Hua Hospital Affiliated to Shanghai Jiao Tong University School of Medicine) and Nai-Qing Zhao (Department of Health Statistics, Public Health College of Fudan University) for their contributions and guidance in the statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Supplementary information
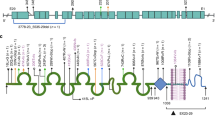
Supplementary Figure S1.
(TIFF 3447 kb)
Rights and permissions
About this article
Cite this article
Kuang, XY., Huang, WY., Xu, H. et al. 254C>G: a TRPC6 promoter variation associated with enhanced transcription and steroid-resistant nephrotic syndrome in Chinese children. Pediatr Res 74, 511–516 (2013). https://doi.org/10.1038/pr.2013.144
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/pr.2013.144
This article is cited by
-
Mutational landscape of TRPC6, WT1, LMX1B, APOL1, PTPRO, PMM2, LAMB2 and WT1 genes associated with Steroid resistant nephrotic syndrome
Molecular Biology Reports (2021)
-
TRPC6 and NPHS2 gene variants in adult patients with steroid-resistant nephrotic syndrome in North-West of Iran
Molecular Biology Reports (2019)