Abstract
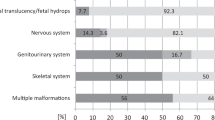
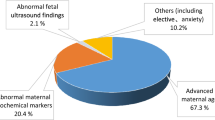
Genetic defects are a major cause of pregnancy loss, leading to fetal death or elective abortion due to congenital anomalies. This study evaluates the effectiveness of trio exome sequencing (ES) in identifying genetic causes of pregnancy loss. Trio ES was used as a first-tier genetic test on 193 cases of pregnancy loss to detect both chromosomal abnormalities and small variants potentially linked to fetal death and anomalies. The pathogenicity of identified variants was assessed, and the diagnostic yield was analyzed. Trio ES provided an overall diagnostic yield of 24% (47/193) across this cohort, with a similar positive rate observed in fetal death (26%, 12/45) and elective abortion (23%, 35/148) groups. Among diagnosed cases, 45% (21/47) were attributed to chromosomal abnormalities, while 55% (26/47) were caused by small variants. This suggests that ES more than doubled the positive rates compared to traditional methods such as karyotyping and chromosomal microarray analysis. Notably, chromosomal abnormalities were the primary cause of fetal death (75%, 9/12), whereas small variants were more prevalent in elective abortion cases (68%, 24/35), particularly those with central nervous and skeletal anomalies. Additional candidate variants were identified in 35 inconclusive cases (18%), potentially further increasing the detection rate. This study highlights the value of trio ES in diagnosing genetic causes of pregnancy loss. Implementing it as a first-tier test can significantly enhance our understanding of fetal death and anomalies, therefore facilitating informed future pregnancy management.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Heaney S, Tomlinson M, Aventin A. Termination of pregnancy for fetal anomaly: a systematic review of the healthcare experiences and needs of parents. BMC Pregnancy Childbirth. 2022;22:441.
Schubert C, Milverton J, Goodall S, Merlin T. A systematic review to assess the utility of genomic autopsy using exome or genome sequencing in cases of congenital anomalies and perinatal death. Genet Med. 2024;26:101159.
Blue NR, Page JM, Silver RM. Genetic abnormalities and pregnancy loss. Semin Perinatol. 2019;43:66–73.
Melo P, Dhillon-Smith R, Islam MA, Devall A, Coomarasamy A. Genetic causes of sporadic and recurrent miscarriage. Fertil Steril. 2023;120:940–4.
Reddy UM, Page GP, Saade GR, Silver RM, Thorsten VR, Parker CB, et al. Karyotype versus microarray testing for genetic abnormalities after stillbirth. N Engl J Med. 2012;367:2185–93.
Zhou Q, Wu SY, Amato K, DiAdamo A, Li P. Spectrum of cytogenomic abnormalities revealed by array comparative genomic hybridization on products of conception culture failure and normal karyotype samples. J Genet Genom. 2016;43:121–31.
Zhao C, Chai H, Zhou Q, Wen J, Reddy UM, Kastury R, et al. Exome sequencing analysis on products of conception: a cohort study to evaluate clinical utility and genetic etiology for pregnancy loss. Genet Med. 2021;23:435–42.
Fu F, Li R, Yu Q, Wang D, Deng Q, Li L, et al. Application of exome sequencing for prenatal diagnosis of fetal structural anomalies: clinical experience and lessons learned from a cohort of 1618 fetuses. Genome Med. 2022;14:123.
Byrne AB, Arts P, Ha TT, Kassahn KS, Pais LS, O’Donnell-Luria A, et al. Genomic autopsy to identify underlying causes of pregnancy loss and perinatal death. Nat Med. 2023;29:180–9.
Talevich E, Shain AH, Botton T, Bastian BC. CNVkit: genome-wide copy number detection and visualization from targeted DNA sequencing. PLoS Comput Biol. 2016;12:e1004873.
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17:405–24.
Riggs ER, Andersen EF, Cherry AM, Kantarci S, Kearney H, Patel A, et al. Technical standards for the interpretation and reporting of constitutional copy-number variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics (ACMG) and the Clinical Genome Resource (ClinGen). Genet Med. 2020;22:245–57.
Lord J, McMullan DJ, Eberhardt RY, Rinck G, Hamilton SJ, Quinlan-Jones E, et al. Prenatal exome sequencing analysis in fetal structural anomalies detected by ultrasonography (PAGE): a cohort study. Lancet. 2019;393:747–57.
Petrovski S, Aggarwal V, Giordano JL, Stosic M, Wou K, Bier L, et al. Whole-exome sequencing in the evaluation of fetal structural anomalies: a prospective cohort study. Lancet. 2019;393:758–67.
Daum H, Meiner V, Elpeleg O, Harel T. collaborating a. Fetal exome sequencing: yield and limitations in a tertiary referral center. Ultrasound Obstet Gynecol. 2019;53:80–86.
Essers R, Lebedev IN, Kurg A, Fonova EA, Stevens SJC, Koeck RM, et al. Prevalence of chromosomal alterations in first-trimester spontaneous pregnancy loss. Nat Med. 2023;29:3233–42.
Bunnell ME, Wilkins-Haug L, Reiss R. Should embryos with autosomal monosomy by preimplantation genetic testing for aneuploidy be transferred?: Implications for embryo selection from a systematic literature review of autosomal monosomy survivors. Prenat Diagn. 2017;37:1273–80.
Viana MM, Vianna GS, Carvalho ERF, da Costa H, de Aguiar MJB. High-level mosaic monosomy 21 in a 13-year-old girl: case report and review of the literature. Am J Med Genet A. 2022;188:953–8.
Ghidini A, Fallet S, Robinowitz J, Lockwood CJ, Dische R, Willner J. Prenatal detection of monosomy 21 mosaicism. Prenat Diagn. 1993;13:163–9.
Scelsa B, Bedeschi FM, Guerneri S, Lalatta F, Introvini P. Partial trisomy of 7q: case report and literature review. J Child Neurol. 2008;23:572–9.
Colley E, Hamilton S, Smith P, Morgan NV, Coomarasamy A, Allen S. Potential genetic causes of miscarriage in euploid pregnancies: a systematic review. Hum Reprod Update. 2019;25:452–72.
Robbins SM, Thimm MA, Valle D, Jelin AC. Genetic diagnosis in first or second trimester pregnancy loss using exome sequencing: a systematic review of human essential genes. J Assist Reprod Genet. 2019;36:1539–48.
Mellis R, Oprych K, Scotchman E, Hill M, Chitty LS. Diagnostic yield of exome sequencing for prenatal diagnosis of fetal structural anomalies: A systematic review and meta-analysis. Prenat Diagn. 2022;42:662–85.
Maksiutenko EM, Barbitoff YA, Nasykhova YA, Pachuliia OV, Lazareva TE, Bespalova ON, et al. The landscape of point mutations in human protein coding genes leading to pregnancy loss. Int J Mol Sci. 2023;24:17572.
Moreno-Leon L, Quezada-Ramirez MA, Bilsbury E, Kiss C, Guerin A, Khanna H. Prenatal phenotype analysis and mutation identification of a fetus with meckel gruber syndrome. Front Genet. 2022;13:982127.
Pang J, Kong F, Tang W, Xi H, Ma N, Sheng X, et al. Two novel TMEM67 variations in a Chinese family with recurrent pregnancy loss: a case report. BMC Med Genomics. 2024;17:156.
Stembalska A, Rydzanicz M, Pollak A, Kostrzewa G, Stawinski P, Biela M, et al. Prenatal versus postnatal diagnosis of Meckel-Gruber and Joubert syndrome in patients with TMEM67 mutations. Genes. 2021;12:1078.
Malloy CA, Polinski C, Alkan S, Manera R, Challapalli M. Hemophagocytic lymphohistiocytosis presenting with nonimmune hydrops fetalis. J Perinatol. 2004;24:458–60.
Vermeulen MJ, de Haas V, Mulder MF, Flohil C, Fetter WP, van de Kamp JM. Hydrops fetalis and early neonatal multiple organ failure in familial hemophagocytic lymphohistiocytosis. Eur J Med Genet. 2009;52:417–20.
Iwatani S, Uemura K, Mizobuchi M, Yoshimoto S, Kawasaki K, Kosaka Y, et al. Familial hemophagocytic lymphohistiocytosis presenting as hydrops fetalis. AJP Rep. 2015;5:e22–24.
Chenhan Z, Jun S, Yang D, Linliang Y, Xiaowen G, Chunya J, et al. A case of Aicardi-Goutieres syndrome caused by TREX1 gene mutation. BMC Pregnancy Childbirth. 2023;23:124.
Lefebvre M, Bruel AL, Tisserant E, Bourgon N, Duffourd Y, Collardeau-Frachon S, et al. Genotype-first in a cohort of 95 fetuses with multiple congenital abnormalities: when exome sequencing reveals unexpected fetal phenotype-genotype correlations. J Med Genet. 2021;58:400–13.
Bakrania P, Ugur Iseri SA, Wyatt AW, Bunyan DJ, Lam WW, Salt A, et al. Sonic hedgehog mutations are an uncommon cause of developmental eye anomalies. Am J Med Genet A. 2010;152A:1310–3.
So PL, Luk HM, Cheung KW, Hui W, Chung MY, Mak ASL, et al. Prenatal phenotype of Kabuki syndrome: a case series and literature review. Prenat Diagn. 2021;41:1089–1100.
Zhang L, Li YL, Zhen L, Li R, Li DZ. Prenatal phenotype of Kabuki syndrome: seven case series. Fetal Diagn Ther. 2022;49:371–6.
Jaganathan K, Kyriazopoulou Panagiotopoulou S, McRae JF, Darbandi SF, Knowles D, Li YI, et al. Predicting splicing from primary sequence with deep learning. Cell. 2019;176:535–548 e524.
Haghshenas S, Bhai P, Aref-Eshghi E, Sadikovic B. Diagnostic utility of genome-wide DNA methylation analysis in Mendelian neurodevelopmental disorders. Int J Mol Sci. 2020;21:9303.
Valencia M, Lapunzina P, Lim D, Zannolli R, Bartholdi D, Wollnik B, et al. Widening the mutation spectrum of EVC and EVC2: ectopic expression of Weyer variants in NIH 3T3 fibroblasts disrupts Hedgehog signaling. Hum Mutat. 2009;30:1667–75.
Bertolacini CD, Ribeiro-Bicudo LA, Petrin A, Richieri-Costa A, Murray JC. Clinical findings in patients with GLI2 mutations-phenotypic variability. Clin Genet. 2012;81:70–75.
Acknowledgements
This study was partly supported by a grant from the Science and Technology Program of Guangzhou, China (2024A03J0755). The authors are sincerely grateful to the patients and their families for participating in this study.
Author information
Authors and Affiliations
Contributions
Conceptualization: XC, LX, PF; Data Curation: LX, AD, XD, XC; Formal Analysis: LX, AD, QZ, JZ, ST, PF, XC; Methodology: XC, JZ, WM, QZ, JZ, ST; Writing-original draft: XC, LX, JZ, ST, PF; Writing-review and editing: all authors. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The research protocol was reviewed and approved by the Institutional Review Board of KingMed Diagnostics (No. 2024099). The study was conducted in accordance with the Declaration of Helsinki. A waiver of informed consent was granted by the Institutional Review Board in the study on the grounds that all data were fully deidentified and anonymized prior to analysis, the study posed no more than minimal risk to participants, and the exemption would not adversely affect the rights or welfare of the individuals involved.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xiang, L., Deng, A., Zhou, J. et al. Diagnostic yield of trio exome sequencing as a first-tier test for identifying genetic causes of pregnancy loss. J Hum Genet 70, 517–527 (2025). https://doi.org/10.1038/s10038-025-01373-7
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s10038-025-01373-7