Abstract
Loeys–Dietz syndrome (LDS), an autosomal dominant connective tissue disorder, was initially considered “atypical” Marfan syndrome (MFS). MFS is caused by mutations in FBN1 encoding fibrillin 1, which binds to transforming growth factor β (TGF-β) to inhibit it from binding to TGF-β receptors. In contrast, LDS is caused by mutations in TGF-β-related genes, including TGFBR2. Some clinical symptoms of LDS, including cardiovascular and skeletal complications, are similar to those observed in MFS; however, arterial tortuosity and widespread aortic aneurysm, hypertelorism, and cleft palate or bifida uvula are specific to LDS. Therefore, the role and difference of the TGF-β signaling pathway in LDS remains unclear. To elucidate the pathological mechanisms of LDS and the phenotypical differences between MFS and LDS, an LDS zebrafish model was established by knocking down tgfbr2b using an antisense morpholino oligonucleotide (tgfbr2b morphant), and the phenotype and expression of genes and proteins related to the TGF-β signaling pathway were investigated. tgfbr2b morphants presented with a dysmorphic face, bent body, and cardiovascular abnormalities, some of which were similar to those observed in patients with LDS. The TGF-β1 gene and protein expression, as well as the genes related to the BMP signaling pathway, were upregulated, and the smad1/5/9 protein exhibited enhanced phosphorylation. These results suggest that dysregulation of BMP signaling during development plays an essential role in the craniofacial dysmorphism and cardiac abnormalities observed in the LDS zebrafish model. Our study clarified the differences of pathological mechanism between MFS and LDS.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Meester JAN, Verstraeten A, Schepers D, Alaerts M, Van Laer L, Loeys BL. Differences in manifestations of Marfan syndrome, Ehlers-Danlos syndrome, and Loeys-Dietz syndrome. Ann Cardiothorac Surg. 2017;6:582–94.
Godwin ARF, Dajani R, Zhang X, Thomson J, Holmes DF, Adamo CS, et al. Fibrillin microfibril structure identifies long-range effects of inherited pathogenic mutations affecting a key regulatory latent TGFβ-binding site. Nat Struct Mol Biol. 2023;30:608–18.
Loeys BL, Chen J, Neptune ER, Judge DP, Podowski M, Holm T, et al. A syndrome of altered cardiovascular, craniofacial, neurocognitive and skeletal development caused by mutations in TGFBR1 or TGFBR2. Nat Genet. 2005;37:275–81.
Regalado ES, Guo DC, Villamizar C, Avidan N, Gilchrist D, McGillivray B, et al. Exome sequencing identifies SMAD3 mutations as a cause of familial thoracic aortic aneurysm and dissection with intracranial and other arterial aneurysms. Circ Res. 2011;109:680–6.
Lindsay ME, Schepers D, Bolar NA, Doyle JJ, Gallo E, Fert-Bober J, et al. Loss-of-function mutations in TGFB2 cause a syndromic presentation of thoracic aortic aneurysm. Nat Genet. 2012;44:922–7.
Bertoli-Avella AM, Gillis E, Morisaki H, Verhagen JMA, de Graaf BM, van de Beek G, et al. Mutations in a TGF-β ligand, TGFB3, cause syndromic aortic aneurysms and dissections. J Am Coll Cardiol. 2015;65:1324–36.
Cannaerts E, Kempers M, Maugeri A, Marcelis C, Gardeitchik T, Richer J, et al. Novel pathogenic SMAD2 variants in five families with arterial aneurysm and dissection: further delineation of the phenotype. J Med Genet. 2019;56:220–7.
Camerota L, Ritelli M, Wischmeijer A, Majore S, Cinquina V, Fortugno P, et al. Genotypic categorization of Loeys-Dietz syndrome based on 24 novel families and literature data. Genes (Basel). 2019;10:764.
Loeys BL, Schwarze U, Holm T, Callewaert BL, Thomas GH, Pannu H, et al. Aneurysm syndromes caused by mutations in the TGF-beta receptor. N Engl J Med. 2006;355:788–98.
Huguenard AL, Johnson GW, Desai RR, Osbun JW, Dacey RG, Braverman AC. Relationship between phenotypic features in Loeys-Dietz syndrome and the presence of intracranial aneurysms. J Neurosurg. 2022;138:1385–92.
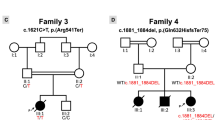
Liu X, Liu K, Hu L, Liu Z, Liu X, Wang J. A novel TGFBR2 mutation causes Loeys-Dietz syndrome in a Chinese infant: A case report. Heliyon. 2025;11:e42116.
Hanyu N, Morishima Y, Shimura M, Suda W, Suzuki S, Go S, et al. Early surgical intervention for Loeys-Dietz Syndrome in a 15-year-old Boy. J Jpn Pediatr Assoc. 2018;122:1198–202.
Miyazono K. Positive and negative regulation of TGF-beta signaling. J Cell Sci. 2000;113:1101–9.
Wu M, Wu S, Chen W, Li YP. The roles and regulatory mechanisms of TGF-β and BMP signaling in bone and cartilage development, homeostasis and disease. Cell Res. 2024;34:101–23.
Tsukamoto S, Mizuta T, Fujimoto M, Ohte S, Osawa K, Miyamoto A, et al. Smad9 is a new type of transcriptional regulator in bone morphogenetic protein signaling. Sci Rep. 2014;4:7596.
Ning J, Zhao Y, Ye Y, Yu J. Opposing roles and potential antagonistic mechanism between TGF-β and BMP pathways: Implications for cancer progression. EBioMedicine. 2019;41:702–10.
Suwanabol PA, Seedial SM, Shi X, Zhang F, Yamanouchi D, Roenneburg D, et al. Transforming growth factor-β increases vascular smooth muscle cell proliferation through the Smad3 and extracellular signal-regulated kinase mitogen-activated protein kinases pathways. J Vasc Surg. 2012;56:446–54.
You W, Hong Y, He H, Huang X, Tao W, Liang X, et al. TGF-β mediates aortic smooth muscle cell senescence in Marfan syndrome. Aging (Albany NY). 2019;11:3574–84.
Van Hemelrijk C, Renard M, Loeys B. The Loeys-Dietz syndrome: an update for the clinician. Curr Opin Cardiol. 2010;25:546–51.
Maleszewski JJ, Miller DV, Lu J, Dietz HC, Halushka MK. Histopathologic findings in ascending aortas from individuals with Loeys-Dietz syndrome (LDS). Am J Surg Pathol. 2009;33:194–201.
Deng Z, Fan T, Xiao C, Tian H, Zheng Y, Li C, et al. TGF-β signaling in health, disease, and therapeutics. Signal Transduct Target Ther. 2024;9:61.
Crosas-Molist E, Meirelles T, López-Luque J, Serra-Peinado C, Selva J, Caja L, et al. Vascular smooth muscle cell phenotypic changes in patients with Marfan syndrome. Arterioscler Thromb Vasc Biol. 2015;35:960–72.
Gallo EM, Loch DC, Habashi JP, Calderon JF, Chen Y, Bedja D, et al. Angiotensin II-dependent TGF-β signaling contributes to Loeys-Dietz syndrome vascular pathogenesis. J Clin Invest. 2014;124:448–60.
Luo, Deng X, Jiang S, Wang Y, Al-Raimi X, Wu AMA, et al. Identification of a pathogenic TGFBR2 variant in a patient with Loeys-Dietz syndrome. Front Genet. 2020;11:479.
Inamoto S, Kwartler CS, Lafont AL, Liang YY, Fadulu VT, Duraisamy S, et al. TGFBR2 mutations alter smooth muscle cell phenotype and predispose to thoracic aortic aneurysms and dissections. Cardiovasc Res. 2010;88:520–9.
Adhish M, Manjubala I. Effectiveness of zebrafish models in understanding human diseases-A review of models. Heliyon. 2023;9:e14557.
Choi J, Dong L, Ahn J, Dao D, Hammerschmidt M, Chen JN. FoxH1 negatively modulates flk1 gene expression and vascular formation in zebrafish. Dev Biol. 2007;304:735–44.
White RM, Sessa A, Burke C, Bowman T, LeBlanc J, Ceol C, et al. Transparent adult zebrafish as a tool for in vivo transplantation analysis. Cell Stem Cell. 2008;2:183–9.
Nusslein-Volhard C, Dahm R. Zebrafish: A Practical Approach. Oxford University Press; 2002.
Kimmel CB, Ballard WW, Kimmel SR, Ullmann B, Schilling TF. Stages of embryonic development of the zebrafish. Dev Dyn. 1995;203:253–310.
Michałowska A, Ponińska J, Chmielewski P, Michałowska I, Płoski R, Bilińska ZT. Intrafamilial variability of cardiovascular abnormalities associated with the p.R460H mutation of the TGFBR2 gene. Pol Arch Intern Med. 2020;130:676–8.
Gordon KJ, Kirkbride KC, How T, Blobe GC. Bone morphogenetic proteins induce pancreatic cancer cell invasiveness through a Smad1-dependent mechanism that involves matrix metalloproteinase-2. Carcinogenesis. 2009;30:238–48.
Wellbrock J, Sheikhzadeh S, Oliveira-Ferrer L, Stamm H, Hillebrand M, Keyser B, et al. Overexpression of Gremlin-1 in patients with Loeys–Dietz syndrome: implications on pathophysiology and early disease detection. PLoS One. 2014;9:e104742.
Kawazu Y, Inamura N, Kayatani F, Okamoto N, Morisaki H. Prenatal complex congenital heart disease with Loeys-Dietz syndrome. Cardiol Young—. 2012;22:116–9.
Muramatsu Y, Kosho T, Magota M, Yokotsuka T, Ito M, Yasuda A, et al. Progressive aortic root and pulmonary artery aneurysms in a neonate with Loeys-Dietz syndrome type 1B. Am J Med Genet A. 2010;152A:417–21.
Quarto N, Li S, Renda A, Longaker MT. Exogenous activation of BMP-2 signaling overcomes TGFβ-mediated inhibition of osteogenesis in Marfan embryonic stem cells and Marfan patient-specific induced pluripotent stem cells. Stem Cells. 2012;30:2709–19. https://doi.org/10.1002/stem.
Kruithof BP, Duim SN, Moerkamp AT, Goumans MJ. TGFβ and BMP signaling in cardiac cushion formation: lessons from mice and chicken. Differentiation. 2012;84:89–102.
Wu M, Chen G, Li YP. TGF-β and BMP signaling in osteoblast, skeletal development, and bone formation, homeostasis and disease. Bone Res. 2016;4:16009.
Yuan G, Zhan Y, Gou X, Chen Y, Yang G. TGF-β signaling inhibits canonical BMP signaling pathway during palate development. Cell Tissue Res. 2018;371:283–91.
Dituri F, Cossu C, Mancarella S, Giannelli G. The interactivity between TGFβ and BMP signaling in organogenesis, fibrosis, and cancer. Cells. 2019;8:1130.
Liu L, Li Q, Yang L, Li Q, Du X. SMAD4 feedback activates the canonical TGF-β family signaling pathways. Int J Mol Sci. 2021;22:10024.
Bonilla-Claudio M, Wang J, Bai Y, Klysik E, Selever J, Martin JF. Bmp signaling regulates a dose-dependent transcriptional program to control facial skeletal development. Development. 2012;139:709–1.
Chen JN, van Eeden FJ, Warren KS, Chin A, Nüsslein-Volhard C, Haffter P, et al. Left-right pattern of cardiac BMP4 may drive asymmetry of the heart in zebrafish. Development. 1997;124:4373–82.
Li B, Pu Z, Liao K, Du Y, Tan G, Nawy S, et al. Overexpression of Bmp4 induces microphthalmia by disrupting embryonic neural retina. Neurobiol Dis. 2024;201:106654.
Acknowledgements
We thank Editage for editing the manuscript. This study was supported by Grants-in-Aid for Scientific Research (C) from the Japanese Ministry of Education, Culture, Sports, Science and Technology (KAKENHI) (grant numbers JP23K06876 and 25K11090), an Intramural Research Grant for Neurological and Psychiatric Disorders of NCNP (grant No. 2-5, 5-6), and a Follow-up Grant from Tokyo Medical University.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chida, R., Kawahara, G., Nakayashiki, M. et al. Development of a zebrafish model of Loeys–Dietz syndrome through tgfbr2b knockdown. J Hum Genet (2026). https://doi.org/10.1038/s10038-026-01457-y
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s10038-026-01457-y