Abstract
Background/Objectives
The metabolic syndrome is a complex condition influenced by many factors including lifestyle. Recently, more and more studies explored the relationships between combined lifestyle factors (often measured as lifestyle scores/indices) and metabolic syndrome due to the co-occurrence of these factors. These scores/indices considered potential interactions among lifestyle factors, offering a more comprehensive understanding of their relationship with metabolic syndrome. However, no review/meta-analysis has been conducted to summarize existing evidence. Thus, this study aimed to synthesize the associations between lifestyle scores/indices and metabolic syndrome in cross-sectional and cohort studies.
Subjects/Methods
A literature search was performed in Embase and Medline. Multivariable-adjusted estimates were synthesized using random-effects models. In research where higher scores indicated better health, we used original estimates directly. In studies where higher scores denoted poorer health, we first calculated the coefficients and standard errors based on original estimates. Afterward, we reversed coefficients’ directions and recalculated new estimates. Thus, the pooled estimates compared the healthiest with the least-healthy lifestyles (the highest vs. lowest scores/indices). Subgroup analyses were conducted based on study design, region, baseline time, baseline age, sex, health status, metabolic syndrome diagnosis, and lifestyles’ number. Sensitivity analyses were performed by including only high-quality studies and employing leave-one-out analyses.
Results
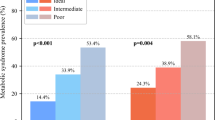
Nineteen studies from 16 publications were included. Physical activity, diet, and smoking were the top three included lifestyle factors. Compared to participants with the least-healthy lifestyles, those with the healthiest lifestyles had a 43% lower metabolic syndrome risk (95% confidence interval = 0.41–0.73). In subgroup analyses, healthy lifestyle scores/indices were inversely associated with both metabolic syndrome prevalence in cross-sectional studies (Odds ratio = 0.62; 95% confidence interval = 0.51–0.73) and metabolic syndrome incidence in cohort studies (Odds ratio = 0.40; 95% confidence interval = 0.11–0.68). The inverse association was consistent in other subgroup and sensitivity analyses.
Conclusions
Adherence to a healthy lifestyle pattern was beneficial to metabolic syndrome prevention.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
All data are available from the correspondence author on reasonable request.
References
Saklayen MG. The Global Epidemic of the Metabolic Syndrome. Curr Hypertens Rep. 2018;20:12.
Huang PL. A comprehensive definition for metabolic syndrome. Dis Model Mech. 2009;2:231–7.
Esposito K, Chiodini P, Colao A, Lenzi A, Giugliano D. Metabolic syndrome and risk of cancer: a systematic review and meta-analysis. Diabetes Care. 2012;35:2402–11.
Zhang D, Liu X, Liu Y, Sun X, Wang B, Ren Y, et al. Leisure-time physical activity and incident metabolic syndrome: a systematic review and dose-response meta-analysis of cohort studies. Metabolism. 2017;75:36–44.
Sun K, Liu J, Ning G. Active smoking and risk of metabolic syndrome: a meta-analysis of prospective studies. PLoS ONE. 2012;7:e47791.
Fabiani R, Naldini G, Chiavarini M. Dietary Patterns and Metabolic Syndrome in Adult Subjects: A Systematic Review and Meta-Analysis. Nutrients. 2019;11:2056.
Alkerwi A, Boutsen M, Vaillant M, Barre J, Lair ML, Albert A, et al. Alcohol consumption and the prevalence of metabolic syndrome: a meta-analysis of observational studies. Atherosclerosis. 2009;204:624–35.
Xie J, Li Y, Zhang Y, Vgontzas AN, Basta M, Chen B, et al. Sleep duration and metabolic syndrome: An updated systematic review and meta-analysis. Sleep Med Rev. 2021;59:101451.
Kuo WC, Bratzke LC, Oakley LD, Kuo F, Wang H, Brown RL. The association between psychological stress and metabolic syndrome: A systematic review and meta-analysis. Obes Rev. 2019;20:1651–64.
Sigit FS, Trompet S, Tahapary DL, Harbuwono DS, le Cessie S, Rosendaal FR, et al. Adherence to the healthy lifestyle guideline in relation to the metabolic syndrome: Analyses from the 2013 and 2018 Indonesian national health surveys. Prev Med Rep. 2022;27:101806.
Vajdi M, Karimi A, Farhangi MA, Ardekani AM. The association between healthy lifestyle score and risk of metabolic syndrome in Iranian adults: a cross-sectional study. BMC Endocr Disord. 2023;23:16.
Sotos-Prieto M, Ortola R, Ruiz-Canela M, Garcia-Esquinas E, Martinez-Gomez D, Lopez-Garcia E, et al. Association between the Mediterranean lifestyle, metabolic syndrome and mortality: a whole-country cohort in Spain. Cardiovasc. 2021;20:5.
Dehghani Firouzabadi F, Jayedi A, Asgari E, Akbarzadeh Z, Janbozorgi N, Djafarian K, et al. Association of Dietary and Lifestyle Inflammation Score With Metabolic Syndrome in a Sample of Iranian Adults. Front Nutr. 2021;8:735174.
Ra JS, Kim H. Combined Effects of Unhealthy Lifestyle Behaviors on Metabolic Syndrome among Postmenopausal Women. Healthcare. 2021;9:05.
Ye Y, Zhou Q, Dai W, Peng H, Zhou S, Tian H, et al. Gender differences in metabolic syndrome and its components in southern china using a healthy lifestyle index: a cross-sectional study. BMC Public Health. 2023;23:686.
Yoon J, Kim J, Son H. Gender Differences of Health Behaviors in the Risk of Metabolic Syndrome for Middle-Aged Adults: A National Cross-Sectional Study in South Korea. Int J Environ Res Public Health. 2021;18:01.
Kwasniewska M, Kaleta D, Dziankowska-Zaborszczyk E, Drygas W. Healthy behaviours, lifestyle patterns and sociodemographic determinants of the metabolic syndrome. Cent Eur J Public Health. 2009;17:14–9.
Sotos-Prieto M, Bhupathiraju SN, Falcon LM, Gao X, Tucker KL, Mattei J. A Healthy Lifestyle Score Is Associated with Cardiometabolic and Neuroendocrine Risk Factors among Puerto Rican Adults. J Nutr. 2015;145:1531–40.
Smith WA, Li C, Nottage KA, Mulrooney DA, Armstrong GT, Lanctot JQ, et al. Lifestyle and metabolic syndrome in adult survivors of childhood cancer: a report from the St. Jude Lifetime Cohort Study. Cancer. 2014;120:2742–50.
Lee JA, Cha YH, Kim SH, Park HS. Impact of combined lifestyle factors on metabolic syndrome in Korean men. J Public Health (Oxf). 2017;39:82–9.
Hershey MS, Sotos-Prieto M, Ruiz-Canela M, Christophi CA, Moffatt S, Martinez-Gonzalez MA, et al. The Mediterranean lifestyle (MEDLIFE) index and metabolic syndrome in a non-Mediterranean working population. Clin Nutr. 2021;40:2494–503.
Romero-Cabrera JL, Garcia-Rios A, Sotos-Prieto M, Quintana-Navarro G, Alcala-Diaz JF, Martin-Piedra L, et al. Adherence to a Mediterranean lifestyle improves metabolic status in coronary heart disease patients: A prospective analysis from the CORDIOPREV study. J Intern Med. 2023;293:574–88.
Farhadnejad H, Parastouei K, Rostami H, Mirmiran P, Azizi F. Dietary and lifestyle inflammatory scores are associated with increased risk of metabolic syndrome in Iranian adults. Diabetol Metab Syndr. 2021;13:30.
Mirmiran P, Farhadnejad H, Teymoori F, Parastouei K, Azizi F. The higher adherence to healthy lifestyle factors is associated with a decreased risk of metabolic syndrome in Iranian adults. Nutr Bull. 2022;47:57–67.
Garralda-Del-Villar M, Carlos-Chilleron S, Diaz-Gutierrez J, Ruiz-Canela M, Gea A, Martinez-Gonzalez MA, et al. Healthy lifestyle and incidence of metabolic syndrome in the SUN cohort. Nutrients. 2018;11:65.
Barbaresko J, Rienks J, Nothlings U. Lifestyle Indices and Cardiovascular Disease Risk: A Meta-analysis. Am J Prev Med. 2018;55:555–64.
Zhang Y, Pan XF, Chen J, Xia L, Cao A, Zhang Y, et al. Combined lifestyle factors and risk of incident type 2 diabetes and prognosis among individuals with type 2 diabetes: a systematic review and meta-analysis of prospective cohort studies. Diabetologia. 2020;63:21–33.
Zhang YB, Pan XF, Chen J, Cao A, Zhang YG, Xia L, et al. Combined lifestyle factors, incident cancer, and cancer mortality: a systematic review and meta-analysis of prospective cohort studies. Br J Cancer. 2020;122:1085–93.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Zeng X, Zhang Y, Kwong JS, Zhang C, Li S, Sun F, et al. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic review. J Evid Based Med. 2015;8:2–10.
Chen D, Zhi Q, Zhou Y, Tao Y, Wu L, Lin H. Association between Dental Caries and BMI in Children: A Systematic Review and Meta-Analysis. Caries Res. 2018;52:230–45.
Mamikutty R, Aly AS, Marhazlinda J. Selecting Risk of Bias Tools for Observational Studies for a Systematic Review of Anthropometric Measurements and Dental Caries among Children. Int J Environ Res Public Health. 2021;18:8623.
Krishnamoorthy Y, Rajaa S, Murali S, Sahoo J, Kar SS. Association between behavioural risk factors and metabolic syndrome among adult population in India: A systematic review and meta-analysis of observational studies. Nutr Metab Cardiovasc Dis. 2022;32:40–52.
Hu J, Zhu X, Yuan D, Ji D, Guo H, Li Y, et al. Association of sleep duration and sleep quality with the risk of metabolic syndrome in adults: a systematic review and meta-analysis. Endokrynol Pol. 2022;73:968–87.
Tenk J, Matrai P, Hegyi P, Rostas I, Garami A, Szabo I, et al. Perceived stress correlates with visceral obesity and lipid parameters of the metabolic syndrome: A systematic review and meta-analysis. Psychoneuroendocrinology. 2018;95:63–73.
Godos J, Zappala G, Bernardini S, Giambini I, Bes-Rastrollo M, Martinez-Gonzalez M. Adherence to the Mediterranean diet is inversely associated with metabolic syndrome occurrence: a meta-analysis of observational studies. Int J Food Sci Nutr. 2017;68:138–48.
Sun K, Ren M, Liu D, Wang C, Yang C, Yan L. Alcohol consumption and risk of metabolic syndrome: a meta-analysis of prospective studies. Clin Nutr. 2014;33:596–602.
Acknowledgements
We would like to express our gratitude to the Early Career Scheme, Research Grants Council of the University Grants Committee: HK (grant number: 25101418); General Research Fund, Research Grants Council of the University Grants Committee: HK (grant number: 15100822); and Central Research Grant of the Hong Kong Polytechnic University (grant number: P0009671). The funders had no role in study design, data collection, data analysis, data interpretation, or writing of the manuscript.
Author information
Authors and Affiliations
Contributions
YD: conceptualization, data curation, formal analysis, investigation, methodology, validation, visualization, writing – original draft, writing – review & editing; QY: formal analysis, validation, writing – review & editing; CH, HHW, TM, XC, FWN: investigation, supervision, validation, writing – review & editing; YJX: conceptualization, funding acquisition, project administration, supervision, validation, writing – review & editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Deng, Y., Yang, Q., Hao, C. et al. Combined lifestyle factors and metabolic syndrome risk: a systematic review and meta-analysis. Int J Obes 49, 226–236 (2025). https://doi.org/10.1038/s41366-024-01671-8
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41366-024-01671-8
This article is cited by
-
The role of insulin resistance in the longitudinal progression from NAFLD to cardiovascular-kidney-metabolic disease
Cardiovascular Diabetology (2025)
-
Association between the psychological frailty index and stroke: a cohort study from CHARLS
Scientific Reports (2025)
-
Triglycerides to high-density lipoprotein cholesterol ratio and its association with periodontitis—a systematic review
BDJ Open (2025)