Abstract
Background/Objective
Obesity is a devastating worldwide metabolic disease, with the highest prevalence in children and adolescents. Obesity impacts neuronal function but the fate of functional hyperemia, a vital mechanism making possible cerebral blood supply to active brain areas, is unknown in organisms fed a high-caloric Western Diet (WD) since adolescence.
Subjects/Methods
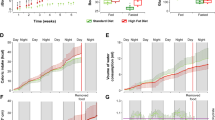
We mapped changes in cerebral blood volume (CBV) in the somatosensory cortex in response to whisker stimulation in adolescent, adult, and middle-aged mice fed a WD since adolescence. To this aim, we used non-invasive and high-resolution functional ultrasound imaging (fUS).
Results
We efficiently mimicked the metabolic syndrome of adolescents in young mice with early weight gain, dysfunctional glucose homeostasis, and insulinemia. Functional hyperemia is compromised as early as 3 weeks of WD and remains impaired after that in adolescent mice. These findings highlight the cerebrovascular vulnerability to WD during adolescence. In WD, ω-6:ω-3 polyunsaturated fatty acids (PUFAs) ratio is unbalanced towards proinflammatory ω-6. A balanced ω-6:ω-3 PUFAs ratio in WD achieved by docosahexaenoic acid supplementation efficiently restores glucose homeostasis and functional hyperemia in adults.
Conclusions
WD triggers a rapid impairment in cerebrovascular activity in adolescence, which is maintained at older ages, and can be rescued by a PUFA-based nutraceutical approach.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
All data generated or analysed during this study are included in this published article (and its Supplementary Information files). Detailed individual analysis will be made available upon request pending application and approval from the corresponding authors.
References
World Health Organization. Overweight and obesity. Updated March 1, 2024. Accessed January 30, 2025. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
Ogden CL, Carroll MD, Lawman HG, Fryar CD, Kruszon-Moran D, Kit BK, et al. Trends in obesity prevalence among children and adolescents in the United States, 1988-1994 through 2013-2014. JAMA. 2016;315:2292–9.
Kopelman PG. Obesity as a medical problem. Nature. 2000;404:635–43.
Goossens GH. The metabolic phenotype in obesity: fat mass, body fat distribution, and adipose tissue function. Obes Facts. 2017;10:207–15.
Sorop O, Dylan Olver T, van de Wouw J, Heinonen I, van Duin RW, Duncker DJ, et al. The microcirculation: a key player in obesity-associated cardiovascular disease. Cardiovasc Res. 2017;113:1035–45.
Soleimanzad H, Montaner M, Ternier G, Lemitre M, Silvestre JS, Kassis N, et al. Obesity in midlife hampers resting and sensory-evoked cerebral blood flow in mice. Obesity. 2021;29:150–8.
Coucha M, Abdelsaid M, Ward R, Abdul Y, Ergul A. Impact of metabolic diseases on cerebral circulation: structural and functional consequences. Compr Physiol. 2018;8:773–99.
Li Y, Dai Q, Jackson JC, Zhang J. Overweight is associated with decreased cognitive functioning among school-age children and adolescents. Obesity. 2008;16:1809–15.
Yau PL, Castro MG, Tagani A, Tsui WH, Convit A. Obesity and metabolic syndrome and functional and structural brain impairments in adolescence. Pediatrics. 2012;130:e856–64.
Garcia-Serrano AM, Duarte JMN. Brain metabolism alterations in type 2 diabetes: what did we learn from diet-induced diabetes models? Front Neurosci. 2020;14:229.
Campana M, Bellini L, Rouch C, Rachdi L, Coant N, Butin N, et al. Inhibition of central de novo ceramide synthesis restores insulin signaling in hypothalamus and enhances β-cell function of obese Zucker rats. Mol Metab. 2018;8:23–36.
Qiao YS, Tang X, Chai YH, Gong HG, Xu H, Patel I, et al. Cerebral blood flow alterations and obesity: a systematic review and meta-analysis. J Alzheimers Dis. 2012;90:15–31.
Iadecola C. The neurovascular unit coming of age: a journey through neurovascular coupling in health and disease. Neuron. 2017;96:17–42.
Schaeffer S, Iadecola C. Revisiting the neurovascular unit. Nat Neurosci. 2012;24:1198–209.
Duncombe J, Kitamura A, Hase Y, Ihara M, Kalaria RJ, Horsburgh K. Chronic cerebral hypoperfusion: a key mechanism leading to vascular cognitive impairment and dementia. Closing the translational gap between rodent models and human vascular cognitive impairment and dementia. Clin Sci. 2017;131:2451–68.
Claassen JAHR, Diaz-Arrastia R, Martin-Cook K, Levine BD, Zhang R. Altered cerebral hemodynamics in early Alzheimer disease: a pilot study using transcranial Doppler. J Alzheimers Dis. 2009;17:621–9.
Duarte JV, Pereira JMS, Quendera B, Raimundo M, Moreno C, Gomes L, et al. Early disrupted neurovascular coupling and changed event level hemodynamic response function in type 2 diabetes: an fMRI study. J Cereb Blood Flow Metab. 2015;35:1671–80.
Valcarcel-Ares VMN, Tucsek Z, Kiss T, Giles CB, Tarantini S, Yabluchanskiy A, et al. Obesity in aging exacerbates neuroinflammation, dysregulating synaptic function-related genes and altering eicosanoid synthesis in the mouse hippocampus: potential role in impaired synaptic plasticity and cognitive decline. J Gerontol A Biol Sci Med Sci. 2019;74:290–8.
Tucsek Z, Toth P, Tarantini S, Sosnowska D, Gautam T, Warrington JP, et al. Aging exacerbates obesity-induced cerebromicrovascular rarefaction, neurovascular uncoupling, and cognitive decline in mice. J Gerontol A Biol Sci Med Sci. 2014;69:1339–52.
Markicevic M, Savvateev I, Grimm C, Zerbi V. Emerging imaging methods to study whole-brain function in rodent models. Transl Psychiatry. 2021;11:457.
Moradi S, Ferdinando H, Zienkiewicz A, Särestöniemi M, Myllylä T. Measurement of cerebral circulation in human. In: Cerebral circulation—updates on models, diagnostics and treatments of related diseases. Ebook editors: Scerrati A., Ricciardi L., Dones F. Ferrara, Italy. (IntechOpen, 2022). https://doi.org/10.5772/intechopen.102383.
Tanter M, Fink M. Ultrafast imaging in biomedical ultrasound. IEEE Trans Ultrason Ferroelectr Freq Control. 2014;61:102–19.
Tanter M, Bercoff J, Sandrin L, Fink M. Ultrafast compound imaging for 2-D motion vector estimation: application to transient elastography. IEEE Trans Ultrason Ferroelectr Freq Control. 2002;49:1363–74.
Deffieux T, Demene C, Pernot M, Tanter M. Functional ultrasound neuroimaging: a review of the preclinical and clinical state of the art. Curr Opin Neurobiol. 2018;50:128–35.
Rahal L, Thibaut M, Rivals I, Claron J, Lenkei Z, Sitt JD, et al. Ultrafast ultrasound imaging pattern analysis reveals distinctive dynamic brain states and potent sub-network alterations in arthritic animals. Sci Rep. 2020;10:10485.
Bortolin RC, Vargas AR, Gasparotto J, Chaves PR, Schnorr CE, Martinello B, et al. A new animal diet based on human Western diet is a robust diet-induced obesity model: comparison to high-fat and cafeteria diets in term of metabolic and gut microbiota disruption. Int J Obes. 2018;42:525–34.
Satterthwaite TD, Shinohara RT, Wolf DH, Hopson RD, Elliott MA, Vandekar SN, et al. Impact of puberty on the evolution of cerebral perfusion during adolescence. Proc Natl Acad Sci USA. 2014;111:8643–8.
Ronan L, Alexander-Bloch AF, Wagstyl K, Farooqi S, Brayne C, Tyler LK, et al. Obesity associated with increased brain age from midlife. Neurobiol Aging. 2016;47:63–70.
Boitard C, Etchamendy N, Sauvant J, Aubert A, Tronel S, Marighetto A, et al. Juvenile, but not adult exposure to high-fat diet impairs relational memory and hippocampal neurogenesis in mice. Hippocampus. 2012;22:2095–100.
Murray S, Chen EY. Examining adolescence as a sensitive period for high-fat, high-sugar diet exposure: a systematic review of the animal literature. Front Neurosci. 2019;13:1108.
Simopoulos AP. Evolutionary aspects of diet: the omega-6/omega-3 ratio and the brain. Mol Neurobiol. 2011;44:203–15.
Bernasconi AA, Wiest MM, Lavie CJ, Milani RV, Laukkanen JA. Effect of omega-3 dosage on cardiovascular outcomes: an updated meta-analysis and meta-regression of interventional trials. Mayo Clin Proc. 2021;96:304–13.
Yamagata K. Dietary docosahexaenoic acid inhibits neurodegeneration and prevents stroke. J Neurosci Res. 2021;99:561–72.
Abbott KA, Burrows TL, Acharya S, Thota RN, Garg ML. DHA-enriched fish oil reduces insulin resistance in overweight and obese adults. Prostaglandins Leukot Essent Fat Acids. 2020;159:102154.
Yamagata K. Docosahexaenoic acid regulates vascular endothelial cell function and prevents cardiovascular disease. Lipids Health Dis. 2017;16:118.
Kansra AR, Lakkunarajah S, Jay MS. Childhood and adolescent obesity: a review. Front Pediatr. 2020;8:581461.
Pulgaron ER, Delamater AM. Obesity and type 2 diabetes in children: epidemiology and treatment. Curr Diab Rep. 2014;14:508.
George MM, Copeland KC. Current treatment options for type 2 diabetes mellitus in youth: today’s realities and lessons from the TODAY study. Curr Diab Rep. 2013;13:72–80.
Cruciani-Guglielmacci C, Vincent-Lamon M, Rouch C, Orosco M, Ktorza A, Magnan C. Early changes in insulin secretion and action induced by high-fat diet are related to a decreased sympathetic tone. Am J Physiol Endocrinol Metab. 2005;288:E148–54.
Khazen T, Hatoum OA, Ferreira G, Maroun M. Acute exposure to a high-fat diet in juvenile male rats disrupts hippocampal-dependent memory and plasticity through glucocorticoids. Sci Rep. 2019;9:12270.
Selim M, Jones R, Novak P, Zhao P, Novak V. The effects of body mass index on cerebral blood flow velocity. Clin Auton Res. 2008;18:331–8.
Peng SL, Chen CM. The influence of obesity on cerebral blood flow in young adults using arterial spin labeling MRI. NMR Biomed. 2020;33:e4375.
Tagi VM, Chiarelli F. Obesity and insulin resistance in children. Curr Opin Pediatr. 2020;32:582–8.
Redel JM, DiFrancesco M, Lee GR, Ziv A, Dolan LM, Brady CC. Cerebral blood flow is lower in youth with type 2 diabetes compared to obese controls: a pilot study. Pediatr Diab. 2022;23:291–300.
Li W, Prakash R, Chawla D, Du W, Didion SP, Filosa JA, et al. Early effects of high-fat diet on neurovascular function and focal ischemic brain injury. Am J Physiol Regul Integr Comp Physiol. 2013;304:R1001–8.
Haley MJ, Krishnan S, Burrows D, de Hoog L, Thakrar J, Schiessl I, et al. Acute high-fat feeding leads to disruptions in glucose homeostasis and worsens stroke outcome. J Cereb Blood Flow Metab. 2019;39:1026–37.
Naneix F, Bakoyiannis I, Santoyo-Zedillo M, Bosch-Bouju C, Pacheco-Lopez G, Coutureau E, et al. Chemogenetic silencing of hippocampus and amygdala reveals a double dissociation in periadolescent obesogenic diet-induced memory alterations. Neurobiol Learn Mem. 2021;178:107354.
Stone EA, Quartermain D. Greater behavioral effects of stress in immature as compared to mature male mice. Physiol Behav. 1997;63:143–5.
Andersen SL. Trajectories of brain development: point of vulnerability or window of opportunity? Neurosci Biobehav Rev. 2003;27:3–18.
Zou P, Scoggins MA, Li Y, Jones M, Helton KJ, Ogg RJ. Developmental patterns of CBF and BOLD responses to visual stimulus. J Cereb Blood Flow Metab. 2021;41:630–40.
Baller EB, Valcarcel AM, Adebimpe A, Alexander-Bloch A, Cui Z, Gur RC, et al. Developmental coupling of cerebral blood flow and fMRI fluctuations in youth. Cell Rep. 2022;38:110576.
Chen JJ, Rosas HD, Salat DH. Age-associated reductions in cerebral blood flow are independent from regional atrophy. NeuroImage. 2011;55:468–78.
Ryder JR, Northrop E, Rudser KD, Kelly AS, Gao Z, Khoury PR, et al. Accelerated early vascular aging among adolescents with obesity and/or type 2 diabetes mellitus. J Am Heart Assoc. 2020;9:e014891.
Williams WKA, Magnuson M, Majeed W, LaConte SM, Peltier SJ, Huet XP, et al. Comparison of alpha-chloralose, medetomidine and isoflurane anesthesia for functional connectivity mapping in the rat. Magn Reson Imaging. 2010;28:995–1003.
Mace E, Montaldo G, Osmanski BF, Cohen I, Fink M, Tanter M. Functional ultrasound imaging of the brain. Nat Methods. 2011;8:662–4.
Boido D, Rungta RL, Osmanski BF, Roche M, Tsurugizawa T, Le Bihan D, et al. Mesoscopic and microscopic imaging of sensory responses in the same animal. Nat Commun. 2019;10:1110.
Bertolo A, et al. High sensitivity mapping of brain-wide functional networks in awake mice using simultaneous multi-slice fUS imaging. Imaging Neurosci. 2023;1:1–18.
Ferrier J, Tiran E, Deffieux T, Tanter M, Lenkei Z. Functional imaging evidence for task-induced deactivation and disconnection of a major default mode network hub in the mouse brain. Proc Natl Acad Sci USA. 2020;117:15270–80.
Gobato AO, Vasques AC, Zambon MP, Barros Filho Ade A, Hessel G. Metabolic syndrome and insulin resistance in obese adolescents. Rev Paul Pediatr. 2014;32:55–62.
Frosch OH, Yau PL, Osorio RS, Rusinek H, Storey P, Convit A. Insulin resistance among obese middle-aged is associated with decreased cerebrovascular reactivity. Neurology. 2017;89:249–55.
Thaler JP, Yi CX, Schur EA, Guyenet SJ, Hwang BH, Dietrich MO, et al. Obesity is associated with hypothalamic injury in rodents and humans. J Clin Invest. 2012;122:153–62.
Erdös B, Snipes JA, Miller AW, Busija DW. Cerebrovascular dysfunction in Zucker obese rats is mediated by oxidative stress and protein kinase C. Diabetes. 2004;53:1352–9.
Gurzell EA, Teague H, Harris M, Clinthorne J, Shaikh SR, Fenton JI. DHA-enriched fish oil targets B cell lipid microdomains and enhances ex vivo and in vivo B cell function. J Leukoc Biol. 2013;93:463–70.
Lin Y, Bai M, Wang S, Chen L, Li Z, Li C, et al. Lactate is a key mediator that links obesity to insulin resistance via modulating cytokine production from adipose tissue. Diabetes. 2022;71:637–52.
Rahman MdH, Bhusal A, Kim JH, Jha MK, Song GJ, Go Y, et al. Astrocytic pyruvate dehydrogenase kinase-2 is involved in hypothalamic inflammation in mouse models of diabetes. Nat Commun. 2020;11:5906.
Zhao X, An X, Yang C, Sun W, Ji H, Lian F. The crucial role and mechanism of insulin resistance in metabolic disease. Front Endocrinol. 2023;14:1149239.
Maschari D, Saxena G, Law TD, Walsh E, Campbell MC, Consitt LA. Lactate-induced lactylation in skeletal muscle is associated with insulin resistance in humans. Front Physiol. 2022;13:951390.
Gunawan F, Matson BC, Coppoli A, Jiang L, Ding Y, Perry R, et al. Deficits in brain glucose transport among younger adults with obesity. Obesity. 2024;32:1329–38.
Rebelos E, Bucci M, Karjalainen T, Oikonen V, Bertoldo A, Hannukainen JC, et al. Insulin resistance is associated with enhanced brain glucose uptake during euglycemic hyperinsulinemia: a large-scale PET cohort. Diab Care. 2021;44:788–94.
Cadario F. Vitamin D and ω-3 polyunsaturated fatty acids towards a personalized nutrition of youth diabetes: a narrative lecture. Nutrients. 2022;14:4887.
Munro IA, Garg ML. Dietary supplementation with long chain omega-3 polyunsaturated fatty acids and weight loss in obese adults. Obes Res Clin Pract. 2013;7:e173–81.
Martínez-Fernández L, Laiglesia LM, Huerta AE, Martínez JA, Moreno-Aliaga MJ. Omega-3 fatty acids and adipose tissue function in obesity and metabolic syndrome. Prostaglandins Other Lipid Mediat. 2015;121:24–41.
Dangardt F, Osika W, Chen Y, Nilsson U, Gan LM, Gronowitz E, et al. Omega-3 fatty acid supplementation improves vascular function and reduces inflammation in obese adolescents. Atherosclerosis. 2010;212:580–5.
Sun GY, Simonyi A, Fritsche KL, Chuang DL, Hannink M, Gu Z, et al. Docosahexaenoic acid (DHA): an essential nutrient and a nutraceutical for brain health and diseases. Prostaglandins Leukot Essent Fat Acids. 2018;136:3–13.
Innes JK, Calder PC. Omega-6 fatty acids and inflammation. Prostaglandins Leukot Essent Fat Acids. 2018;132:41–48.
Simopoulos AP. An increase in the omega-6/omega-3 fatty acid ratio increases the risk for obesity. Nutrients. 2016;8:128.
Joris PJ, Mensink RP, Adam TC, Liu TT. Cerebral blood flow measurements in adults: a review on the effects of dietary factors and exercise. Nutrients. 2018;10:530.
de Wilde MC, Farkas E, Gerrits M, Kiliaan AJ, Luiten PGM. The effect of n-3 polyunsaturated fatty acid-rich diets on cognitive and cerebrovascular parameters in chronic cerebral hypoperfusion. Brain Res. 2002;947:166–73.
Arnoldussen IAC, Zerbi V, Wiesmann M, Noordman RHJ, Bolijn S, Mutsaers MPC, et al. Early intake of long-chain polyunsaturated fatty acids preserves brain structure and function in diet-induced obesity. J Nutr Biochem. 2016;30:177–88.
Charrière K, Ghzaiel I, Lizard G, Vejux A. Involvement of microglia in neurodegenerative diseases: beneficial effects of docosahexahenoic acid (DHA) supplied by food or combined with nanoparticles. Int J Mol Sci. 2021;22:10639.
Balbi M, Ghosh M, Longden TA, Vega MJ, Gesierich B, Hellal F, et al. Dysfunction of mouse cerebral arteries during early aging. J Cereb Blood Flow Metab. 2015;35:1445–53.
Zaletel M, Strucl M, Pretnar-Oblak J, Zvan B. Age-related changes in the relationship between visual evoked potentials and visually evoked cerebral blood flow velocity response. Funct Neurol 2005;20:115–20.
Spear LP. The adolescent brain and age-related behavioral manifestations. Neurosci Biobehav Rev. 2000;24:417–63.
Deffieux T, Demené C, Tanter M. Functional ultrasound imaging: a new imaging modality for neuroscience. Neuroscience. 2021;474:110–21.
Friston KJ, Holmes AP, Poline JB, Grasby PJ, Williams SC, Frackowiak RS, et al. Analysis of fMRI time-series revisited. NeuroImage. 1995;2:45–53.
Paxinos G, Franklin KBG. Paxinos and Franklin’s the Mouse Brain in Stereotaxic Coordinates - 5th Edition. 2019. Academic Press. San Diego, USA. https://www.elsevier.com/books/paxinos-and-franklins-the-mouse-brain-in-stereotaxic-coordinates/paxinos/978-0-12-816157-9.
Acknowledgements
We thank the animal core facility “Buffon” of the University of Paris Cité/Jacques Monod Institute for Animal Care.
Funding
HS had a postdoctoral fellowship award from NIH and AXA. MM had a doctoral fellowship award from Idex Université Paris Cité. This work was supported by the AXA Research Fund (MT).
Author information
Authors and Affiliations
Contributions
HS and CM equally contributed to the work. They designed the experiments, acquired and analyzed the imaging data along with MM for metabolic phenotyping. FP and CM edited the article. MT and HG equally contributed to the work. They designed the experiments and wrote the article together with HS, CM, MM, FP, and CM, MT and HG supervised the project.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
All animal experiments were approved by the committee for animal care of Université Paris Cité and by the French Ministry of Research (agreement #17629) under the European directive 2010/63/UE.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Soleimanzad, H., Morisset, C., Montaner, M. et al. Western diet since adolescence impairs brain functional hyperemia at adulthood in mice: rescue by a balanced ω-3:ω-6 polyunsaturated fatty acids ratio. Int J Obes 49, 844–854 (2025). https://doi.org/10.1038/s41366-025-01711-x
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41366-025-01711-x