Abstract
Background/Objectives
To examine the relationship between early childhood adiposity, adolescent lifestyles, gut microbiota and steatotic liver disease (SLD) development in adolescents using data from a prospective, longitudinal cohort study.
Methods
We included 69 adolescents (14–17 years old) with SLD and 69 adolescents without SLD, matched for BMI-z scores, sex, and age, from the 13-year longitudinal cohort the “Growth and Obesity Cohort Study”. Anthropometric data between the ages of 4 and 17 and lifestyle parameters (including diet and physical activity) at 14–17 years old were evaluated. Fecal samples were collected and microbiome composition and function were assessed using 16S ribosomal RNA amplicon sequencing.
Results
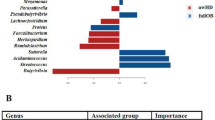
Principal component analysis demonstrated dietary intake factors and childhood adiposity factors expanding the distribution variation between case and control groups, respectively. Lower odds of developing SLD during adolescence was associated with higher levels of daily fiber intake during adolescence (adjusted odds ratio = 0.91) and lower childhood adiposity (triceps skinfold at 5 years of age, suprailiac skinfold at 8 and 11 years of age, and waist-to-hip ratio at age 5–9 years). SLD was associated with a lower abundance of specific microbial species, such as Bacteroides vulgatus, which was higher in the control group compared to the case group (control/case abundance ratio = 18.71). B. vulgatus abundance also positively correlated with dietary fiber intake and inversely correlated with childhood adiposity.
Conclusions
Adiposity in early childhood and a low dietary fiber intake may contribute to the pathogenesis of SLD during adolescence, possibly through alterations to the intestinal microbiome; these findings could inform early disease markers and targets for intervention.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others

Data availability
All data generated or analyzed during this study are included in this published article (and its supplementary information files).
References
Panera N, Barbaro B, Della Corte C, Mosca A, Nobili V, Alisi A. A review of the pathogenic and therapeutic role of nutrition in pediatric nonalcoholic fatty liver disease. Nutr Res. 2018;58:1–16.
Trico D, Caprio S, Rosaria Umano G, Pierpont B, Nouws J, Galderisi A, et al. Metabolic Features of Nonalcoholic Fatty Liver (NAFL) in Obese Adolescents: Findings From a Multiethnic Cohort. Hepatology. 2018;68:1376–90.
Anderson EL, Howe LD, Jones HE, Higgins JP, Lawlor DA, Fraser A. The Prevalence of Non-Alcoholic Fatty Liver Disease in Children and Adolescents: A Systematic Review and Meta-Analysis. PLoS One. 2015;10:e0140908.
Schwimmer JB, Deutsch R, Kahen T, Lavine JE, Stanley C, Behling C. Prevalence of fatty liver in children and adolescents. Pediatrics. 2006;118:1388–93.
Holmer M, Ekstedt M, Nasr P, Zenlander R, Wester A, Tavaglione F, et al. Effect of common genetic variants on the risk of cirrhosis in non-alcoholic fatty liver disease during 20 years of follow-up. Liver Int. 2022;42:2769–80.
Brunt EM, Wong VW, Nobili V, Day CP, Sookoian S, Maher JJ, et al. Nonalcoholic fatty liver disease. Nat Rev Dis Primers. 2015;1:15080.
Sookoian S, Pirola CJ. The genetic epidemiology of nonalcoholic fatty liver disease: toward a personalized medicine. Clin Liver Dis. 2012;16:467–85.
Rinella ME, Lazarus JV, Ratziu V, Francque SM, Sanyal AJ, Kanwal F, et al. A multisociety Delphi consensus statement on new fatty liver disease nomenclature. Hepatology. 2023;78:1966–86.
Jung JH, Jung MK, Kim KE, Kwon AR, Chae HW, Yoon CS, et al. Ultrasound measurement of pediatric visceral fat thickness: correlations with metabolic and liver profiles. Ann Pediatr Endocrinol Metab. 2016;21:75–80.
European Society for Pediatric Gastroenterology Hepatology and Nutrition, European Association for the Study of the Liver, North American Society for Pediatric Gastroenterology Hepatology and Nutrition, Nutrition, Latin-American Society for Pediatric Gastroenterology Hepatology and Nutrition, et al. Paediatric steatotic liver disease has unique characteristics: A multisociety statement endorsing the new nomenclature. J Pediatr Gastroenterol Nutr. 2024;78(5):1190–6.
Silveira LS, Monteiro PA, Antunes BdMM, Seraphim PM, Fernandes RA, Christofaro DGD, et al. Intra-abdominal fat is related to metabolic syndrome and non-alcoholic fat liver disease in obese youth. BMC Pediatrics. 2013;13:1–6.
Alberti G, Faune M, Santos JL, De Barbieri F, Garcia C, Pereira A, et al. Relation between Body Composition Trajectories from Childhood to Adolescence and Nonalcoholic Fatty Liver Disease Risk. Nutrients. 2024;16:785.
Musso G, Gambino R, De Michieli F, Cassader M, Rizzetto M, Durazzo M, et al. Dietary habits and their relations to insulin resistance and postprandial lipemia in nonalcoholic steatohepatitis. Hepatology. 2003;37:909–16.
Cortez-Pinto H, Jesus L, Barros H, Lopes C, Moura MC, Camilo ME. How different is the dietary pattern in non-alcoholic steatohepatitis patients? Clin Nutr. 2006;25:816–23.
Papandreou D, Karabouta Z, Pantoleon A, Rousso I. Investigation of anthropometric, biochemical and dietary parameters of obese children with and without non-alcoholic fatty liver disease. Appetite. 2012;59:939–44.
Hoyles L, Fernandez-Real JM, Federici M, Serino M, Abbott J, Charpentier J, et al. Publisher Correction: Molecular phenomics and metagenomics of hepatic steatosis in non-diabetic obese women. Nat Med. 2018;24:1628.
Wang B, Jiang X, Cao M, Ge J, Bao Q, Tang L, et al. Altered Fecal Microbiota Correlates with Liver Biochemistry in Nonobese Patients with Non-alcoholic Fatty Liver Disease. Sci Rep. 2016;6:32002.
Aron-Wisnewsky J, Vigliotti C, Witjes J, Le P, Holleboom AG, Verheij J, et al. Gut microbiota and human NAFLD: disentangling microbial signatures from metabolic disorders. Nat Rev Gastroenterol Hepatol. 2020;17:279–97.
Zhu L, Baker SS, Gill C, Liu W, Alkhouri R, Baker RD, et al. Characterization of gut microbiomes in nonalcoholic steatohepatitis (NASH) patients: a connection between endogenous alcohol and NASH. Hepatology. 2013;57:601–9.
Nier A, Engstler AJ, Maier IB, Bergheim I. Markers of intestinal permeability are already altered in early stages of non-alcoholic fatty liver disease: Studies in children. PLoS One. 2017;12:e0183282.
Michail S, Lin M, Frey MR, Fanter R, Paliy O, Hilbush B, et al. Altered gut microbial energy and metabolism in children with non-alcoholic fatty liver disease. FEMS Microbiol Ecol. 2015;91:1–9.
Del Chierico F, Nobili V, Vernocchi P, Russo A, De Stefanis C, Gnani D, et al. Gut microbiota profiling of pediatric nonalcoholic fatty liver disease and obese patients unveiled by an integrated meta-omics-based approach. Hepatology. 2017;65:451–64.
Schwimmer JB, Johnson JS, Angeles JE, Behling C, Belt PH, Borecki I, et al. Microbiome Signatures Associated With Steatohepatitis and Moderate to Severe Fibrosis in Children With Nonalcoholic Fatty Liver Disease. Gastroenterology. 2019;157:1109–22.
Testerman T, Li Z, Galuppo B, Graf J, Santoro N. Insights from shotgun metagenomics into bacterial species and metabolic pathways associated with NAFLD in obese youth. Hepatol Commun. 2022;6:1962–74.
Zhong H, Penders J, Shi Z, Ren H, Cai K, Fang C, et al. Impact of early events and lifestyle on the gut microbiota and metabolic phenotypes in young school-age children. Microbiome. 2019;7:1–14.
Corvalan C, Uauy R, Stein AD, Kain J, Martorell R. Effect of growth on cardiometabolic status at 4 y of age. Am J Clin Nutr. 2009;90:547–55.
CDC. About Underage Drinking. Available from: https://www.cdc.gov/alcohol/underage-drinking/?CDC_AAref_Val=https://www.cdc.gov/alcohol/fact-sheets/underage-drinking.htm.
Vajro P, Lenta S, Socha P, Dhawan A, McKiernan P, Baumann U, et al. Diagnosis of nonalcoholic fatty liver disease in children and adolescents: position paper of the ESPGHAN Hepatology Committee. J Pediatr Gastroenterol Nutr. 2012;54:700–13.
Strauss S, Gavish E, Gottlieb P, Katsnelson L. Interobserver and intraobserver variability in the sonographic assessment of fatty liver. AJR Am J Roentgenol. 2007;189:W320–3.
de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85:660–7.
Fernandez JR, Redden DT, Pietrobelli A, Allison DB. Waist circumference percentiles in nationally representative samples of African-American, European-American, and Mexican-American children and adolescents. J Pediatr. 2004;145:439–44.
Cediel G, Corvalan C, Lopez de Romana D, Mericq V, Uauy R. Prepubertal Adiposity, Vitamin D Status, and Insulin Resistance. Pediatrics. 2016;138:e20160076.
USDA ARS. Automated Multiple-Pass Method. 2024. Available from: https://www.ars.usda.gov/northeast-area/beltsville-md-bhnrc/beltsville-human-nutrition-research-center/food-surveys-research-group/docs/ampm-usda-automated-multiple-pass-method/.
USDA ARS. National Nutrient Database for Standard Reference Release 28. 2020. Available from: https://www.ars.usda.gov/northeast-area/beltsville-md-bhnrc/beltsville-human-nutrition-research-center/methods-and-application-of-food-composition-laboratory/mafcl-site-pages/sr11-sr28/.
Chile MoHo. Chilean National Food Survey. In Annex: Tables of Weight Equivalences of the Photographic Atlas of Chilean Foods and Chilean Food Preparations. Santiago, Chile; Ministerio de Salud Chile, 2010.
Rebolledo N, Reyes M, Corvalan C, Popkin BM, Smith Taillie L. Dietary Intake by Food Source and Eating Location in Low- and Middle-Income Chilean Preschool Children and Adolescents from Southeast Santiago. Nutrients. 2019;11:1695.
Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–95.
Bolyen E, Rideout JR, Dillon MR, Bokulich NA, Abnet CC, Al-Ghalith GA, et al. Reproducible, interactive, scalable and extensible microbiome data science using QIIME 2. Nat Biotechnol. 2019;37:852–7.
Callahan BJ, McMurdie PJ, Rosen MJ, Han AW, Johnson AJ, Holmes SP. DADA2: High-resolution sample inference from Illumina amplicon data. Nat Methods. 2016;13:581–3.
Wang Q, Garrity GM, Tiedje JM, Cole JR. Naive Bayesian classifier for rapid assignment of rRNA sequences into the new bacterial taxonomy. Appl Environ Microbiol. 2007;73:5261–7.
Oksanen J, Simpson GL, Blanchet FG, Kindt R, Legendre P, Minchin PR et al. Vegan: Community Ecology Package. 2023. Available from: http://CRAN.R-project.org/package=vegan.
Paradis E, Claude J, Strimmer K. APE: analyses of phylogenetics and evolution in R language. Bioinformatics. 2004;20:289–90.
Vos MB, Lavine JE. Dietary fructose in nonalcoholic fatty liver disease. Hepatology. 2013;57:2525–31.
Lirio LM, Forechi L, Zanardo TC, Batista HM, Meira EF, Nogueira BV, et al. Chronic fructose intake accelerates non-alcoholic fatty liver disease in the presence of essential hypertension. J Diabetes Complications. 2016;30:85–92.
Jensen T, Abdelmalek MF, Sullivan S, Nadeau KJ, Green M, Roncal C, et al. Fructose and sugar: A major mediator of non-alcoholic fatty liver disease. J Hepatol. 2018;68:1063–75.
Ouyang X, Cirillo P, Sautin Y, McCall S, Bruchette JL, Diehl AM, et al. Fructose consumption as a risk factor for non-alcoholic fatty liver disease. J Hepatol. 2008;48:993–9.
Schwarz JM, Noworolski SM, Erkin-Cakmak A, Korn NJ, Wen MJ, Tai VW, et al. Effects of Dietary Fructose Restriction on Liver Fat, De Novo Lipogenesis, and Insulin Kinetics in Children With Obesity. Gastroenterology. 2017;153:743–52.
Wang R, Yan R, Jiao J, Li F, Zhang H, Chang Z, et al. Fruit and vegetable intake and the risk of non-alcoholic fatty liver disease: a meta-analysis of observational studies. Front Nutr. 2024;11:1398184.
Du LJ, He ZY, Gu X, Hu X, Zhang XX, Yang LJ, et al. Inverse Association of Fruit and Vegetable Consumption with Nonalcoholic Fatty Liver Disease in Chinese Patients with Type 2 Diabetes Mellitus. Nutrients. 2022;14:4559.
Kanerva N, Sandboge S, Kaartinen NE, Mannisto S, Eriksson JG. Higher fructose intake is inversely associated with risk of nonalcoholic fatty liver disease in older Finnish adults. Am J Clin Nutr. 2014;100:1133–8.
Vasdev S, Gill V, Parai S, Longerich L, Gadag V. Dietary vitamin E and C supplementation prevents fructose induced hypertension in rats. Mol Cell Biochem. 2002;241:107–14.
Jiang X, Zheng J, Zhang S, Wang B, Wu C, Guo X. Advances in the Involvement of Gut Microbiota in Pathophysiology of NAFLD. Front Med. 2020;7:361.
Yoshida N, Emoto T, Yamashita T, Watanabe H, Hayashi T, Tabata T, et al. Bacteroides vulgatus and Bacteroides dorei Reduce Gut Microbial Lipopolysaccharide Production and Inhibit Atherosclerosis. Circulation. 2018;138:2486–98.
You HJ, Si J, Kim J, Yoon S, Cha KH, Yoon HS, et al. Bacteroides vulgatus SNUG 40005 Restores Akkermansia Depletion by Metabolite Modulation. Gastroenterology. 2023;164:103–16.
Zhang B, Chen T, Cao M, Yuan C, Reiter RJ, Zhao Z, et al. Gut Microbiota Dysbiosis Induced by Decreasing Endogenous Melatonin Mediates the Pathogenesis of Alzheimer’s Disease and Obesity. Front Immunol. 2022;13:900132.
Raman M, Ahmed I, Gillevet PM, Probert CS, Ratcliffe NM, Smith S, et al. Fecal microbiome and volatile organic compound metabolome in obese humans with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2013;11:868–75 e1-3.
Loomba R, Seguritan V, Li W, Long T, Klitgord N, Bhatt A, et al. Gut Microbiome-Based Metagenomic Signature for Non-invasive Detection of Advanced Fibrosis in Human Nonalcoholic Fatty Liver Disease. Cell Metab. 2017;25:1054–62 e5.
Hrncir T, Hrncirova L, Kverka M, Hromadka R, Machova V, Trckova E, et al. Gut Microbiota and NAFLD: Pathogenetic Mechanisms, Microbiota Signatures, and Therapeutic Interventions. Microorganisms. 2021;9:957.
Xia Y, Zhang S, Zhang Q, Liu L, Meng G, Wu H, et al. Insoluble dietary fibre intake is associated with lower prevalence of newly-diagnosed non-alcoholic fatty liver disease in Chinese men: a large population-based cross-sectional study. Nutr Metab. 2020;17:4.
Zhao H, Yang A, Mao L, Quan Y, Cui J, Sun Y. Association Between Dietary Fiber Intake and Non-alcoholic Fatty Liver Disease in Adults. Front Nutr. 2020;7:593735.
Alferink LJ, Kiefte-de Jong JC, Erler NS, Veldt BJ, Schoufour JD, de Knegt RJ, et al. Association of dietary macronutrient composition and non-alcoholic fatty liver disease in an ageing population: the Rotterdam Study. Gut. 2019;68:1088–98.
Koh A, De Vadder F, Kovatcheva-Datchary P, Backhed F. From Dietary Fiber to Host Physiology: Short-Chain Fatty Acids as Key Bacterial Metabolites. Cell. 2016;165:1332–45.
Perez-Montes de Oca A, Julian MT, Ramos A, Puig-Domingo M, Alonso N. Microbiota, Fiber, and NAFLD: Is There Any Connection? Nutrients. 2020;12:3100.
Patnode ML, Beller ZW, Han ND, Cheng J, Peters SL, Terrapon N, et al. Interspecies Competition Impacts Targeted Manipulation of Human Gut Bacteria by Fiber-Derived Glycans. Cell. 2019;179:59–73.e13.
Wan F, Pan F, Ayonrinde OT, Adams LA, Mori TA, Beilin LJ, et al. Validation of fatty liver disease scoring systems for ultrasound diagnosed non-alcoholic fatty liver disease in adolescents. Dig Liver Dis. 2021;53:746–52.
Cuzmar V, Alberti G, Uauy R, Pereira A, Garcia C, De Barbieri F, et al. Early Obesity: Risk Factor for Fatty Liver Disease. J Pediatr Gastroenterol Nutr. 2020;70:93–8.
Bjorntorp P. Portal” adipose tissue as a generator of risk factors for cardiovascular disease and diabetes. Arteriosclerosis. 1990;10:493–6.
Ibrahim MM. Subcutaneous and visceral adipose tissue: structural and functional differences. Obes Rev. 2010;11:11–8.
McCann JR, Bihlmeyer NA, Roche K, Catherine C, Jawahar J, Kwee LC, et al. The Pediatric Obesity Microbiome and Metabolism Study (POMMS): Methods, Baseline Data, and Early Insights. Obesity. 2021;29:569–78.
Feldstein AE, Charatcharoenwitthaya P, Treeprasertsuk S, Benson JT, Enders FB, Angulo P. The natural history of non-alcoholic fatty liver disease in children: a follow-up study for up to 20 years. Gut. 2009;58:1538–44.
Funding
This project is funded by FONDECYT 1161456 and 1200839. CC is funded by Young Scientists Fund of the National Natural Science Foundation of China (82103953) and Fundamental Research Funds for the Central Universities (20720220060). ZZ is funded by the Natural Science Foundation of Fujian Province (2022J01332).
Author information
Authors and Affiliations
Contributions
EW and JCG designed the study. AP, GA and JCG performed clinical studies. CC and ZZ analyzed and interpreted data. CC drafted the manuscript. ZZ, EW, and JCG critical revision of the manuscript for important intellectual content. FDB and CG performed and analyzed clinical data. GA analyzed nutricional data. All authors revised and approved the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cai, C., Zhang, Z., Alberti, G. et al. Early childhood adiposity, lifestyle and gut microbiome are linked to steatotic liver disease development in adolescents. Int J Obes 49, 1056–1065 (2025). https://doi.org/10.1038/s41366-025-01737-1
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41366-025-01737-1