Abstract
Background
Previous research has suggested that children who are exposed to chronic stress are at greater risk for childhood obesity, however little research has examined the mechanism of this association. This study aimed to investigate the association between family and household stress during the COVID-19 pandemic and children’s BMIz, and whether children’s hair cortisol concentration (HCC) mediates this association.
Methods
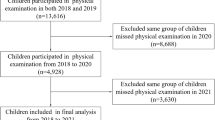
This study used baseline data from 228 children 2–6 years from the Family Stress Study, a prospective cohort study of families with children 2–6 years. Parents responded to an online survey which assessed family and household stressors including family functioning, home chaos, financial insecurity, food insecurity, parental depression, parenting stress, stressful life events, and COVID-19 stressors. A total family chronic stress index score was calculated from parents’ responses on these measures. Hair samples were collected from children to assess their HCC. The Hayes PROCESS mediation macro was used to assess the total, direct, and indirect effect of the family chronic stress index on child BMIz, adjusting for household income and child ethnicity/race.
Results
We found that the family chronic stress index was associated with higher child BMIz (b = 0.815, 95% CI = 0.181–1.449), but this association was not mediated by children’s HCC (b = 0.004, CI = −0.042–0.076).
Conclusions
Future research should continue to investigate hair cortisol as a measure of chronic stress among children younger than 6 years and explore other mechanisms of how chronic stress is associated with children’s weight outcomes, such as through parenting practices that influence children’s eating behaviour or physical activity, or children’s weight-related behaviours.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author, SD, upon reasonable request.
Code availability
The code that support the findings of this study are available from the corresponding author, SD, upon reasonable request.
References
Gundersen C, Mahatmya D, Garasky S, Lohman B. Linking psychosocial stressors and childhood obesity. Obes Rev. 2011;12:e54–63.
Pervanidou P, Chrousos GP. Stress and pediatric obesity: neurobiology and behavior. Fam Relat. 2016;65:85–93.
Lynch T, Azuero A, Lochman JE, Park N-J, Turner-Henson A, Rice M. The influence of psychological stress, depressive symptoms, and cortisol on body mass and central adiposity in 10- to-12-year-old children. J Pediatr Nurs. 2019;44:42–9.
Kappes C, Stein R, Körner A, Merkenschlager A, Kiess W. Stress, stress reduction and obesity in childhood and adolescence. Horm Res Paediatr. 2023;96:88–96.
Suglia SF, Duarte CS, Chambers EC, Boynton-Jarrett R. Cumulative social risk and obesity in early childhood. Pediatrics. 2012;129:e1173–e9.
Halliday JA, Palma CL, Mellor D, Green J, Renzaho AMN. The relationship between family functioning and child and adolescent overweight and obesity: a systematic review. Int J Obes. 2014;38:480–93.
East P, Delker E, Blanco E, Burrows R, Lozoff B, Gahagan S. Home and family environment related to development of obesity: a 21-year longitudinal study. Child Obes. 2019;15:156–66.
Shorer M, Leibovich L. Young children’s emotional stress reactions during the COVID-19 outbreak and their associations with parental emotion regulation and parental playfulness. Early Child Dev Care. 2022;192:861–71.
Schmidt SJ, Barblan LP, Lory I, Landolt MA. Age-related effects of the COVID-19 pandemic on mental health of children and adolescents. Eur J Psychotraumatol. 2021;12:1901407.
Adams EL, Smith D, Caccavale LJ, Bean MK. Parents are stressed! Patterns of parent stress across COVID-19. Front Psychiatry. 2021;12:626456.
Foley S, Badinlou F, Brocki KC, Frick MA, Ronchi L, Hughes C. Family function and child adjustment difficulties in the COVID-19 pandemic: an international study. Int J Environ Res Public Health. 2021;18:11136.
Feinberg ME, Mogle J, Lee JK, Tornello SL, Hostetler ML, Cifelli JA, et al. Impact of the COVID-19 pandemic on parent, child, and family functioning. Fam Process. 2022;61:361–74.
Han J-A, Chung Y-E, Chung I-H, Hong Y-H, Chung S. Impact of the COVID-19 pandemic on seasonal variations in childhood and adolescent growth: experience of pediatric endocrine clinics. Children. 2021;8:404.
Androutsos O, Perperidi M, Georgiou C, Chouliaras G. Lifestyle changes and determinants of children’s and adolescents’ body weight increase during the first COVID-19 lockdown in Greece: the COV-EAT study. Nutrients. 2021;13:930.
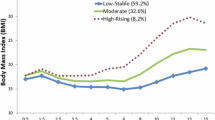
Vogel M, Geserick M, Gausche R, Beger C, Poulain T, Meigen C, et al. Age- and weight group-specific weight gain patterns in children and adolescents during the 15 years before and during the COVID-19 pandemic. Int J Obes. 2022;46:144–52.
Kiecolt-Glaser JK, Habash DL, Fagundes CP, Andridge R, Peng J, Malarkey WB, et al. Daily stressors, past depression, and metabolic responses to high-fat meals: a novel path to obesity. Biol Psychiatry. 2015;77:653–60.
Björntorp P. Do stress reactions cause abdominal obesity and comorbidities?. Obes Rev. 2001;2:73–86.
Incollingo Rodriguez AC, Epel ES, White ML, Standen EC, Seckl JR, Tomiyama AJ. Hypothalamic-pituitary-adrenal axis dysregulation and cortisol activity in obesity: a systematic review. Psychoneuroendocrinology. 2015;62:301–18.
Moss RH, Conner M, O’Connor DB. Exploring the effects of daily hassles and uplifts on eating behaviour in young adults: the role of daily cortisol levels. Psychoneuroendocrinology. 2021;129:105231.
O’Connor DB, Thayer JF, Vedhara K. Stress and health: a review of psychobiological processes. Annu Rev Psychol. 2021;72:663–88.
Miller AL, Clifford C, Sturza J, Rosenblum K, Vazquez DM, Kaciroti N, et al. Blunted cortisol response to stress is associated with higher body mass index in low-income preschool-aged children. Psychoneuroendocrinology. 2013;38:2611–7.
Kiess W, Meidert A, Dressendörfer RA, Schriever K, Kessler U, Köunig A, et al. Salivary cortisol levels throughout childhood and adolescence: relation with age, pubertal stage, and weight. Pediatr Res. 1995;37:502–6.
Miller AL, Kaciroti N, Sturza J, Retzloff L, Rosenblum K, Vazquez DM, et al. Associations between stress biology indicators and overweight across toddlerhood. Psychoneuroendocrinology. 2017;79:98–106.
Mendoza MM, Dmitrieva J, Perreira KM, Hurwich-Reiss E, Watamura SE. The effects of economic and sociocultural stressors on the well-being of children of Latino immigrants living in poverty. Cult Divers Ethn Minor Psychol. 2017;23:15–26.
Chu L, Shen K, Liu P, Ye K, Wang Y, Li C, et al. Increased cortisol and cortisone levels in overweight children. Med Sci Monit Basic Res. 2017;23:25–30.
Kunin-Batson AS, Crain AL, Gunnar MR, Kelly AS, Kharbanda EO, Haapala J, et al. Household income, cortisol, and obesity during early childhood: a prospective longitudinal study. J Pediatr. 2023;252:76–82.
Ling J, Kao TSA, Robbins LB. Body mass index, waist circumference and body fat are positively correlated with hair cortisol in children: a systematic review and meta-analysis. Obes Rev. 2020;21:e13050–n/a.
Ma L, Liu X, Yan N, Gan Y, Wu Y, Li Y, et al. Associations between different cortisol measures and adiposity in children: a systematic review and meta-analysis. Front Nutr. 2022;9:879256.
Spiga F, Walker JJ, Terry JR, Lightman SL. HPA axis-rhythms. Compr Physiol. 2014;4:1273–98.
Hellhammer J, Fries E, Schweisthal OW, Schlotz W, Stone AA, Hagemann D. Several daily measurements are necessary to reliably assess the cortisol rise after awakening: state- and trait components. Psychoneuroendocrinology. 2007;32:80–6.
Gibson EL, Checkley S, Papadopoulos A, Poon L, Daley S, Wardle J. Increased salivary cortisol reliably induced by a protein-rich midday meal. Psychosom Med. 1999;61:214–24.
Michels N, Sioen I, De Vriendt T, Huybrechts I, Vanaelst B, De Henauw S. Children’s morning and evening salivary cortisol: pattern, instruction compliance and sampling confounders. Horm Res Paediatr. 2012;77:27–35.
Russell E, Koren G, Rieder M, Van Uum S. Hair cortisol as a biological marker of chronic stress: current status, future directions and unanswered questions. Psychoneuroendocrinology. 2012;37:589–601.
Stalder T, Kirschbaum C. Analysis of cortisol in hair—state of the art and future directions. Brain Behav Immun. 2012;26:1019–29.
Miller AL, Gearhardt AN, Retzloff L, Sturza J, Kaciroti N, Lumeng JC. Early childhood stress and child age predict longitudinal increases in obesogenic eating among low-income children. Acad Pediatr. 2018;18:685–91.
Oh DL, Jerman P, Silvério Marques S, Koita K, Purewal Boparai SK, Burke Harris N, et al. Systematic review of pediatric health outcomes associated with childhood adversity. BMC Pediatr. 2018;18:83.
Huybrechts I, Beirlaen C, De Vriendt T, Slimani N, Pisa PT, Schouppe E, et al. Validity of instruction leaflets for parents to measure their child’s weight and height at home: results obtained from a randomised controlled trial. BMJ Open. 2014;4:e003768.
Huybrechts I, Himes JH, Ottevaere C, De Vriendt T, De Keyzer W, Cox B, et al. Validity of parent-reported weight and height of preschool children measured at home or estimated without home measurement: a validation study. BMC Pediatr. 2011;11:63.
Tenenbaum A, Shefer-Averbuch N, Lazar L, Yakobovitch-Gavan M, Phillip M, Oron T. Growth assessment of children during the COVID-19 pandemic—can we rely on parental measurements?. Acta Paediatr. 2021;110:3040–5.
Myatt M, Guevarra E. zscorer: Child Anthropometry z-Score Calculator. 2019. https://cran.r-project.org/web/packages/zscorer/index.html.
World Health Organization. Child growth standards. https://www.who.int/tools/child-growth-standards.
Sauve B, Koren G, Walsh G, Tokmakejian S, Van Uum SHM. Measurement of cortisol in human hair as a biomarker of systemic exposure. Clin Investig Med. 2007;30:E183–91.
Hayashi S, Miyamoto I, Takeda K. Measurement of human hair growth by optical microscopy and image analysis. Br J Dermatol. 1991;125:123–9.
Kirschbaum C, Tietze A, Skoluda N, Dettenborn L. Hair as a retrospective calendar of cortisol production—increased cortisol incorporation into hair in the third trimester of pregnancy. Psychoneuroendocrinology. 2009;34:32–7.
Hayes AF. Partial, conditional, and moderated moderated mediation: quantification, inference, and interpretation. Commun Monogr. 2018;85:4–40.
Moreno-Black G, Stockard J. Two worlds of obesity: ethnic differences in child overweight/obesity prevalence and trajectories. J Racial Ethn Health Disparities. 2016;3:331–9.
Isong IA, Richmond T, Avendaño M, Kawachi I. Racial/ethnic disparities: a longitudinal study of growth trajectories among US kindergarten children. J Racial Ethn Health Disparities. 2018;5:875–84.
Statistics Canada. Income statistics by economic family type and income source. 2024. https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1110019101.
Tate EB, Wood W, Liao Y, Dunton GF. Do stressed mothers have heavier children? A meta-analysis on the relationship between maternal stress and child body mass index. Obes Rev. 2015;16:351–61.
Vanaelst B, Michels N, Clays E, Herrmann D, Huybrechts I, Sioen I, et al. The association between childhood stress and body composition, and the role of stress-related lifestyle factors—cross-sectional findings from the baseline ChiBS survey. Int J Behav Med. 2014;21:292–301.
Lumeng JC, Miller A, Peterson KE, Kaciroti N, Sturza J, Rosenblum K, et al. Diurnal cortisol pattern, eating behaviors and overweight in low-income preschool-aged children. Appetite. 2014;73:65–72.
Christaki EV, Pervanidou P, Papassotiriou I, Bastaki D, Valavani E, Mantzou A, et al. Stress, inflammation and metabolic biomarkers are associated with body composition measures in lean, overweight, and obese children and adolescents. Children. 2022;9:291.
Christaki EV, Pervanidou P, Papassotiriou I, Mantzou A, Giannakakis G, Boschiero D, et al. Circulating FGF21 vs. stress markers in girls during childhood and adolescence, and in their caregivers: intriguing inter-relations between overweight/obesity, emotions, behavior, and the cared-caregiver relationship. Children. 2022;9:821.
Bryson HE, Mensah F, Goldfeld S, Price AMH. Using hair cortisol to examine the role of stress in children’s health inequalities at 3 years. Acad Pediatr. 2020;20:193–202.
Schloß S, Ruhl I, Müller V, Becker K, Skoluda N, Nater UM, et al. Low hair cortisol concentration and emerging attention-deficit/hyperactivity symptoms in preschool age. Dev Psychobiol. 2018;60:722–9.
Slopen N, Roberts AL, LeWinn KZ, Bush NR, Rovnaghi CR, Tylavsky F, et al. Maternal experiences of trauma and hair cortisol in early childhood in a prospective cohort. Psychoneuroendocrinology. 2018;98:168–76.
Larsen SC, Fahrenkrug J, Olsen NJ, Heitmann BL. Association between hair cortisol concentration and adiposity measures among children and parents from the “Healthy Start” study. PLoS ONE. 2016;11:e0163639.
Rovnaghi CR, Kala AF, Allen SL, Anand KJS. Interpretation of cortisol concentrations and reference intervals from the CALIPER database. Clin Chem. 2014;60:418–9.
Binz TM, Rietschel L, Streit F, Hofmann M, Gehrke J, Herdener M, et al. Endogenous cortisol in keratinized matrices: systematic determination of baseline cortisol levels in hair and the influence of sex, age and hair color. Forensic Sci Int. 2018;284:33–8.
Jansen E, Thapaliya G, Aghababian A, Sadler J, Smith K, Carnell S. Parental stress, food parenting practices and child snack intake during the COVID-19 pandemic. Appetite. 2021;161:105119.
Walton K, Simpson JR, Darlington G, Haines J. Parenting stress: a cross-sectional analysis of associations with childhood obesity, physical activity, and TV viewing. BMC Pediatr. 2014;14:244.
Parks EP, Kumanyika S, Moore RH, Stettler N, Wrotniak BH, Kazak A. Influence of stress in parents on child obesity and related behaviors. Pediatrics. 2012;130:e1096–104.
Webb HJ, Zimmer-Gembeck MJ, Scuffham PA, Scott R, Barber B. Family stress predicts poorer dietary quality in children: examining the role of the parent–child relationship. Infant Child Dev. 2018;27.
Sadeh A, Raviv A, Gruber R. Sleep patterns and sleep disruptions in school-age children. Dev Psychol. 2000;36:291–301.
Coto J, Garcia A, Hart KC, Graziano PA. Associations between disruptive behavior problems, parenting factors, and sleep problems among young children. J Dev Behav Pediatr. 2018;39:610–20.
Michels N, Sioen I, Boone L, Clays E, Vanaelst B, Huybrechts I, et al. Cross-lagged associations between children’s stress and adiposity: the Children’s Body Composition and Stress study. Psychosom Med. 2015;77:50–8.
Vismara L, Rollè L, Agostini F, Sechi C, Fenaroli V, Molgora S, et al. Perinatal parenting stress, anxiety, and depression outcomes in first-time mothers and fathers: a 3- to 6-months postpartum follow-up study. Front Psychol. 2016;7:938.
Widarsson M, Engström G, Rosenblad A, Kerstis B, Edlund B, Lundberg P. Parental stress in early parenthood among mothers and fathers in Sweden. Scand J Caring Sci. 2013;27:839–47.
Skreden M, Skari H, Malt UF, Pripp AH, BjÖRk MD, Faugli A, et al. Parenting stress and emotional wellbeing in mothers and fathers of preschool children. Scand J Public Health. 2012;40:596–604.
Vanderwall C, Randall Clark R, Eickhoff J, Carrel AL. BMI is a poor predictor of adiposity in young overweight and obese children. BMC Pediatr. 2017;17:135.
Acknowledgements
The authors would like to acknowledge and thank the families participating in the Family Stress Study. The Family Stress Study is supported by the Canadian Institutes of Health Research (419814) and the McMaster University COVID-19 Research Fund. The funding partners played no role in study design, methods, participant recruitment, data collection, analysis, or preparation of this paper.
Author information
Authors and Affiliations
Contributions
Conceptualization—JH, KM; methodology—AL, PT, AM, KM, JH; formal analysis—AL, PT; writing, original draft preparation—SD, JH; writing, review and editing—SD, AL, PT, AB, AM, SP, EG, AD, DM, LV, KM, JH; supervision—JH, KM. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41366_2025_1802_MOESM1_ESM.docx
Total, direct, and indirect effects of the family chronic stress index (including responses from two parents) on child BMIz
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Douglas, S., Laila, A., Tremblay, P.F. et al. Family stress and child BMIz during the COVID-19 pandemic: exploring the mediating effects of cortisol. Int J Obes 49, 1616–1622 (2025). https://doi.org/10.1038/s41366-025-01802-9
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41366-025-01802-9