Abstract
Background
Individuals who have chronic pain experience reductions in physical activity (PA), quality of life, and physical capabilities, creating a debilitating cycle where decreased PA and increased weight exacerbate pain. This study aimed to examine associations between weight status, PA, and time spent in pain using a nationally representative sample, accounting for demographic factors.
Methods
Using data from the 2011–2012 NHANES cycle, a comparison of pain groups with weight status and PA (total and type) and a mediation analysis using PA (total and type) as a mediator between weight status and time spent in pain were conducted.
Results
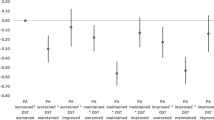
Total PA groups differed in pain levels with those engaging in vigorous activity having the lowest prevalence in the "pain always" category (5.4%), and those with obesity had a higher prevalence of “pain always” (49.6%) compared to those with normal weight (19.5%) and those with overweight (30.9%). Total PA mediated the relationship between people with obesity and the amount of time spent in pain (effect:1.141; CI:0.456–1.837), that is, compared to those who have normal weight, those who have obesity were less likely to meet the total PA guideline, and subsequently likely to spend more days in pain. Breaking down PA by types, travel PA (effect:0.071; CI:0.024–0.152), moderate recreational PA (effect:0.041; CI:0.018–0.079), and vigorous recreational PA (effect:0.135; CI:0.035–0.279) significantly mediated the relationships between people with obesity and days spent in pain.
Conclusion
Findings suggest that vigorous PA is linked to lower pain prevalence. Additionally, PA significantly mediates the relationship between people with obesity and days spent in pain. While people with overweight alone was not associated with the number of days spent in pain, engaging in vigorous recreational activities was linked to reductions in days spent in pain for individuals with overweight, highlighting the importance of staying active to manage pain.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study were extracted from the National Health and Nutrition Examination Study (NHANES) 2011-2012 repository, https://wwwn.cdc.gov/nchs/nhanes/search/datapage.aspx?Component=Demographics&Cycle=2011-2012. The specified extracted data and their applicable datasets, generated during and/or analyzed during the current study, are available from the corresponding author upon reasonable request.
References
Hardt J, Jacobsen C, Goldberg J, Nickel R, Buchwald D. Prevalence of chronic pain in a representative sample in the United States. Pain Med. 2008;9:803–12. https://doi.org/10.1111/j.1526-4637.2008.00425.x.
Nahin RL, Feinberg T, Kapos FP, Terman GW. Estimated rates of incident and persistent chronic pain among US adults, 2019-2020. JAMA Netw Open. 2023;6:2313563 https://doi.org/10.1001/jamanetworkopen.2023.13563.
Caudill-Slosberg MA, Schwartz LM, Woloshin S. Office visits and analgesic prescriptions for musculoskeletal pain in US: 1980 vs. 2000. Pain. 2004;109:514–9. https://doi.org/10.1016/j.pain.2004.03.006.
Heneweer H, Vanhees L, Picavet HSJ. Physical activity and low back pain: a U-shaped relation? Pain. 2009;143:21–5. https://doi.org/10.1016/j.pain.2008.12.033.
Landmark T, Romundstad P, Borchgrevink PC, Kaasa S, Dale O. Associations between recreational exercise and chronic pain in the general population: evidence from the HUNT 3 study. Pain. 2011;152:2241–7. https://doi.org/10.1016/j.pain.2011.04.029.
McBeth J, Nicholl BI, Cordingley L, Davies KA, MacFarlane GJ. Chronic widespread pain predicts physical inactivity: Results from the prospective EPIFUND study. Eur J Pain. 2010;14:972–9. https://doi.org/10.1016/j.ejpain.2010.03.005.
Smuck M, Kao MC, Brar N, Martinez-Ith A, Choi J. Tomkins-Lane CC Does physical activity influence the relationship between low back pain and obesity? Spine J 2014;14:209–16. https://doi.org/10.1016/j.spinee.2013.11.010.
Hashem LE, Roffey DM, Alfasi AM, Papineau GD, Wai DC, Phan P, et al. Exploration of the inter-relationships between obesity, physical inactivity, inflammation, and low back pain. Spine. 2018;43:1218–24. https://doi.org/10.1097/BRS.0000000000002582.
Fernandes IM, da C, Pinto RZ, Ferreira P, Lira FS. Low back pain, obesity, and inflammatory markers: exercise as potential treatment. J Exerc Rehabilit. 2018;14:168–74. https://doi.org/10.12965/jer.1836070.035.
Heuch I, Heuch I, Hagen K, Zwart J-A. Overweight and obesity as risk factors for chronic low back pain: a new follow-up in the HUNT Study. BMC Public Health. 2024;24:2618. https://doi.org/10.1186/s12889-024-20011-z.
Narouze S, Souzdalnitski D. Obesity and chronic pain: systematic review of prevalence and implications for pain practice. Regional Anesthesia. Pain Med. 2015;40:91–111. https://doi.org/10.1097/AAP.0000000000000218.
Lopez-Jimenez F, Almahmeed W, Bays H, Cuevas A, Di Angelantonio E, le Roux CW, et al. Obesity and cardiovascular disease: mechanistic insights and management strategies. A joint position paper by the World Heart Federation and World Obesity Federation. Eur J Prev Cardiol. 2022;29:2218–37. https://doi.org/10.1093/eurjpc/zwac187.
Scully T, Ettela A, LeRoith D, Gallagher EJ. Obesity, Type 2 Diabetes, and Cancer Risk. Front Oncol. 2021;10:10. https://doi.org/10.3389/fonc.2020.615375.
Marcus DA. Obesity and the impact of chronic pain. Clin J Pain. 2004;20:186–91. https://doi.org/10.1097/00002508-200405000-00009.
Booth J, Moseley GL, Schiltenwolf M, Cashin A, Davies M, Hübscher M. Exercise for chronic musculoskeletal pain: a biopsychosocial approach. Musculoskelet Care. 2017;15:413–21. https://doi.org/10.1002/msc.1191.
Seaman DR. Body mass index and musculoskeletal pain: is there a connection? Chiropr Man Therapies. 2013;21:15. https://doi.org/10.1186/2045-709X-21-15.
Dong HJ, Larsson B, Levin LÅ, Bernfort L, Gerdle B. Is excess weight a burden for older adults who suffer chronic pain. BMC Geriatr. 2018;18:270. https://doi.org/10.1186/s12877-018-0963-4.
Ray L, Lipton RB, Zimmerman ME, Katz MJ, Derby CA. Mechanisms of association between obesity and chronic pain in the elderly. Pain. 2011;152:53–59. https://doi.org/10.1016/j.pain.2010.08.043.
Umeda M, Kim Y. Gender differences in the prevalence of chronic pain and leisure time physical activity among US adults: a NHANES study. Int J Environ Res Public Health. 2019;16:988. https://doi.org/10.3390/ijerph16060988.
Meucci RD, Fassa AG, Xavier Faria NM. Prevalence of chronic low back pain: Systematic review. Rev de Saude Publ. 2015;49:49. https://doi.org/10.1590/S0034-8910.2015049005874.
McBeth J, Jones K. Epidemiology of chronic musculoskeletal pain. Best Pract Res Clin Rheumatol. 2007;21:403–25. https://doi.org/10.1016/j.berh.2007.03.003.
Strath LJ, Peterson JA, Meng L, Rani A, Huo Z, Foster TC, et al. Socioeconomic status, knee pain, and epigenetic aging in community-dwelling middle-to-older age adults. J Pain. 2024;25:293–301. https://doi.org/10.1016/j.jpain.2023.06.002.
Elagizi A, Kachur S, Carbone S, Lavie CJ, Blair SN. A review of obesity, physical activity, and cardiovascular disease. Curr Obes Rep.2020;9:571–81. https://doi.org/10.1007/s13679-020-00403-z.
Armstrong T, Bull F. Development of the World Health Organization Global Physical Activity Questionnaire (GPAQ). J Public Health. 2006;14:66–70. https://doi.org/10.1007/s10389-006-0024-x.
Riebe D, Ehrman JK, Liguori G, Magal M. American College of Sports Medicine: ACSM’s Guidelines for Exercise Testing and Prescription. Wolters Kluwer Health. 2018.
CDC/National Center for Health Statistics. Weighting in NHANES.
Mackinnon DP. Introduction to Statistical Mediation Analysis. Introduction Stat Mediation Anal. 2012. https://doi.org/10.4324/9780203809556.
Hayes AF. Beyond Baron and Kenny: statistical mediation analysis in the new millennium. Commun Monogr. 2009;76:408–20. https://doi.org/10.1080/03637750903310360.
Lai K. Estimating standardized SEM parameters given nonnormal data and incorrect model: methods and comparison. Structural Eq Model. 2018;25:600-20. https://doi.org/10.1080/10705511.2017.1392248.
Graham JW. Missing data: analysis and design. Missing data: Anal Des. 2012. https://doi.org/10.1007/978-1-4614-4018-5.
Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Eq Model. 1999;6:1–55. https://doi.org/10.1080/10705519909540118.
Hagströmer M, Oja P, Sjöström M. The International Physical Activity Questionnaire (IPAQ): a study of concurrent and construct validity. Public Health Nutr. 2006;9:755–62. https://doi.org/10.1079/phn2005898.
Cameron AJ, Magliano DJ, Dunstan DW, Zimmet PZ, Hesketh K, Peeters A, et al. A bi-directional relationship between obesity and health-related quality of life: Evidence from the longitudinal AusDiab study. Int J Obes. 2012;36:295–303. https://doi.org/10.1038/ijo.2011.103.
Bigand T, Wilson M, Bindler R, Daratha K. Examining risk for persistent pain among adults with overweight status. Pain Manag Nurs. 2018;19:549–56. https://doi.org/10.1016/j.pmn.2018.02.066.
Hitt HC, McMillen RC, Thornton-Neaves T, Koch K, Cosby AG. Comorbidity of Obesity and Pain in a General Population: Results from the Southern Pain Prevalence Study. J Pain. 2007;8:430–6. https://doi.org/10.1016/j.jpain.2006.12.003.
Majedi H, Amini MH, Yousefshahi F, Khazaeipour Z, Majedi M, Rahimi M, et al. Predicting factors of pain duration in patients with chronic pain: A large population-based study. Anesth Pain Med. 2020;10:e95776. https://doi.org/10.5812/aapm.95776.
Mccarthy LH, Bigal ME, Katz M, Derby C, Lipton RB. Chronic pain and obesity in elderly people: Results from the einstein aging study. J Am Geriatr Soc. 2009;57:115–9. https://doi.org/10.1111/j.1532-5415.2008.02089.x.
Andrzejewski W, Kassolik K, Brzozowski M, Cymer K. The influence of age and physical activity on the pressure sensitivity of soft tissues of the musculoskeletal system. J Bodyw Mov Ther. 2010;14:382–90. https://doi.org/10.1016/j.jbmt.2009.07.004.
Naugle KM, Riley JL. Self-reported physical activity predicts pain inhibitory and facilitatory function. Med Sci Sports Exerc. 2014;46:622–9. https://doi.org/10.1249/MSS.0b013e3182a69cf1.
Sluka KA, O’Donnell JM, Danielson J, Rasmussen LA. Regular physical activity prevents development of chronic pain and activation of central neurons. J Appl Physiol. 2013;114:725–33. https://doi.org/10.1152/japplphysiol.01317.2012.
Ellingson LD, Colbert LH, Cook DB. Physical activity is related to pain sensitivity in healthy women. Med Sci Sports Exerc. 2012;44:1401–6. https://doi.org/10.1249/MSS.0b013e318248f648.
Gyasi RM, Adjakloe YDA, Siaw LP, James PB, Amoah PA, Abass K, et al. The effect-modification of physical activity on the association of pain with impaired physical function in aging adults. Exp Gerontol. 2022;163:111791. https://doi.org/10.1016/j.exger.2022.111791.
Vaegter HB, Jones MD. Exercise-induced hypoalgesia after acute and regular exercise: Experimental and clinical manifestations and possible mechanisms in individuals with and without pain. Pain Rep. 2020;5:e823 https://doi.org/10.1097/PR9.0000000000000823.
Niwa Y, Shimo K, Ohga S, Tokiwa Y, Hattori T, Matsubara T. Effects of Exercise-Induced Hypoalgesia at Different Aerobic Exercise Intensities in Healthy Young Adults. J Pain Res. 2022;15:3615–24. https://doi.org/10.2147/JPR.S384306.
Peterson JA, Lohman C, Larson RD, Bemben MG, Black CD. Lean mass is associated with, but does not mediate sex differences in pressure pain sensitivity in healthy adults. J Pain Res. 2022;15:3981–94. https://doi.org/10.2147/JPR.S387635.
Peterson JA, Lohman C, Larson RD, Bemben MG, Black CD. Body composition does not influence conditioned pain modulation and exercise-induced hyperalgesia in healthy males and females. Eur J Pain. 2022;26:1800–10. https://doi.org/10.1002/ejp.2005.
Johnson AJ, Peterson JA, Vincent HK, Manini T, Cruz-Almeida Y. Body composition and body mass index are independently associated with widespread pain and experimental pain sensitivity in older adults: a pilot investigation. Front Pain Res. 2024;5:5. https://doi.org/10.3389/fpain.2024.1386573.
Paley CA, Johnson MI. Physical activity to reduce systemic inflammation associated with chronic pain and obesity a narrative review. Clin J Pain. 2016;32:365–70. https://doi.org/10.1097/AJP.0000000000000258.
Bartley EJ, Fillingim RB. Sex differences in pain: a brief review of clinical and experimental findings. Br J Anaesth. 2013;111:52–8. https://doi.org/10.1093/bja/aet127.
Mogil JS. Qualitative sex differences in pain processing: emerging evidence of a biased literature. Nat Rev Neurosci. 2020;21:353–65. https://doi.org/10.1038/s41583-020-0310-6.
Cimmino MA, Ferrone C, Cutolo M. Epidemiology of chronic musculoskeletal pain. Best Pr Res. 2011;25:173–83. https://doi.org/10.1016/j.berh.2010.01.012.
McDougall JJ. Arthritis and pain. Neurogenic origin of joint pain. Arthritis Res Ther. 2006;8:220. https://doi.org/10.1186/ar2069.
Calvo E, Córdova C, Shura R, Allel K, Alvaro CC, Keyes KM, et al. Global Pain and Aging: A Cross-Sectional Study on Age Differences in the Intensity of Chronic Pain Among Middle-Aged and Older Adults in 20 Countries. J Gerontol Ser B Psychological Sci Soc Sci. 2023;78:1098–108. https://doi.org/10.1093/geronb/gbac199.
Hastie BA, Riley JL, Fillingim RB. Ethnic differences in pain coping: Factor structure of the coping strategies questionnaire and coping strategies questionnaire-revised. J Pain. 2004;5:304–16. https://doi.org/10.1016/j.jpain.2004.05.004.
Booker SQ. African Americans’ perceptions of pain and pain management: a systematic review. J Transcultural Nurs. 2016;27:73–80. https://doi.org/10.1177/1043659614526250.
Jackson P, Spector AL, Strath LJ, Antoine LH, Li P, Goodin BR. et al. Epigenetic age acceleration mediates the relationship between neighborhood deprivation and pain severity in adults with or at risk for knee osteoarthritis pain. Soc Sci Med. 2023;331:116088. https://doi.org/10.1016/j.socscimed.2023.116088.
Prego-Domínguez J, Khazaeipour Z, Mallah N, Takkouche B. Socioeconomic status and occurrence of chronic pain: a meta-analysis. Rheumatology. 2021;60:1091–105. https://doi.org/10.1093/rheumatology/keaa758.
Arias O, Koenig G, Choi SD. Musculoskeletal acute and chronic pain surveyed among construction workers in Wisconsin, United States: a pilot study. Sustainability. 2022;14:13279. https://doi.org/10.3390/su142013279.
Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychol Methods. 2002;7:147–77. https://doi.org/10.1037/1082-989X.7.2.147.
Author information
Authors and Affiliations
Contributions
JP drafted the manuscript, performed data analysis, created tables and figures, and made revisions. AV contributed to the conceptualization of the study, assisted with drafting the manuscript, and participated in data collection. DL and YL served as primary data analysts and statisticians for the project. RL assisted in the study design and reviewed and approved the initial and subsequent manuscript drafts. CB designed the study, contributed to conceptualization, participated in data extraction, and provided overall project oversight and management. All authors made edits, reviewed, and approved the manuscript at various points of submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics statement
All methods were performed in accordance with the relevant guidelines and regulations.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Peterson, J.A., Venturini, A., Larson, D.J. et al. Physical activity mediates the relationship between weight status and pain impacting daily activities. Int J Obes 49, 1882–1890 (2025). https://doi.org/10.1038/s41366-025-01838-x
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41366-025-01838-x