Abstract
Background
Early detection of the disease obesity and support for patients living with obesity could improve the success of obesity treatment and management. The factors influencing the delay in obesity treatment, defined as the period between obesity onset and treatment start, are largely unknown. The aim of our study is to explore the help-seeking behavior of PwO towards obesity treatment.
Methods
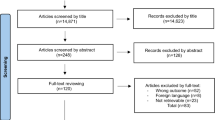
In this cross-sectional qualitative study, consecutive patients visiting the obesity clinic of the University Hospitals of Brussels between December 2023 and April 2024 were invited to participate. PwO were interviewed, and data were transcribed and analysed using thematic analysis.
Results
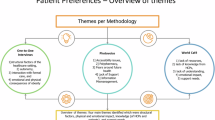
A total of 18 PwO (61% female, median age 37 years, (IQR: 23.5–57.5)) were interviewed. The journey of PwO towards obesity care seemed complex with multiple HCPs involved. Four themes were identified as triggers for seeking obesity care: Referral from primary care, family, friends and schools; Health complications; Financial burden of living with obesity; and Increased internal motivation. Three themes were identified as factors increasing treatment delay: Inefficient referral; Pressure from society to try lifestyle approaches first; and Challenges to overcome barriers for metabolic surgery. Inefficient referral from dietitians to multidisciplinary obesity treatment was identified as the main cause of treatment delay. PwO feel discouraged by the limited effectiveness of dietary guidance, leading to disengagement from the healthcare system.
Conclusion
Our findings identify several key barriers contributing to treatment delays for patients with obesity. People living with obesity emphasized the need for an obesity care pathway and improved communication among primary care providers, allied health professionals, and collaborating centres for obesity management (COMs) to reduce the time required to access appropriate obesity treatment. Additionally, societal perceptions framing obesity as a result of a lack of willpower were reported by patients with obesity as a barrier to seeking care.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
Information concerning data availability can be found in appendix 2.
References
Tim Lobstein HBaM, Neveux. World obesity atlas 2022. World Obesity Federation 2022.
Bowman-Busato J, Schreurs L, Halford JCG, Yumuk V, O’Malley G, Woodward E, et al. Providing a common language for obesity: the European Association for the Study of Obesity obesity taxonomy. Int J Obes (Lond) 2024.
Hildebrand S, Pfeifer A. The obesity pandemic and its impact on non-communicable disease burden. Pflugers Arch. 2025, https://doi.org/10.1007/s00424-025-03066-8.
Nyberg ST, Batty GD, Pentti J, Virtanen M, Alfredsson L, Fransson EI, et al. Obesity and loss of disease-free years owing to major non-communicable diseases: a multicohort study. Lancet Public Health. 2018;3:e490–e7.
Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377:13–27.
Tremmel M, Gerdtham UG, Nilsson PM, Saha S. Economic burden of obesity: a systematic literature review. Int J Environ Res Public Health. 2017;14. https://doi.org/10.3390/ijerph14040435.
Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, Halsey J, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373:1083–96.
Abdullah A, Stoelwinder J, Shortreed S, Wolfe R, Stevenson C, Walls H, et al. The duration of obesity and the risk of type 2 diabetes. Public Health Nutr. 2011;14:119–26.
Alpert MA, Lambert CR, Panayiotou H, Terry BE, Cohen MV, Massey CV, et al. Relation of duration of morbid obesity to left ventricular mass, systolic function, and diastolic filling, and effect of weight loss. Am J Cardiol. 1995;76:1194–7.
Fallah-Fini S, Adam A, Cheskin LJ, Bartsch SM, Lee BY. The additional costs and health effects of a patient having overweight or obesity: a computational model. Obes (Silver Spring). 2017;25:1809–15.
Rigas G, Williams K, Sumithran P, Brown WA, Swinbourne J, Purcell K, et al. Delays in healthcare consultations about obesity—Barriers and implications. Obes Res Clin Pract. 2020;14:487–90.
Caterson ID, Alfadda AA, Auerbach P, Coutinho W, Cuevas A, Dicker D, et al. Gaps to bridge: Misalignment between perception, reality and actions in obesity. Diab Obes Metab. 2019;21:1914–24.
Barry VB, Raiff BR. Weight management preferences in a non-treatment seeking sample. Health Promot Perspect. 2013;3:147–53.
Tol J, Swinkels IC, De Bakker DH, Veenhof C, Seidell JC. Overweight and obese adults have low intentions of seeking weight-related care: a cross-sectional survey. BMC Public Health. 2014;14:582.
Bunt SNW, Mérelle SYM, Steenhuis IHM, Kroeze W. Predictors of need for help with weight loss among overweight and obese men and women in the Netherlands: a cross-sectional study. BMC Health Serv Res. 2017;17:819.
Rubino F, Cummings DE, Eckel RH, Cohen RV, Wilding JPH, Brown WA, et al. Definition and diagnostic criteria of clinical obesity. Lancet Diab Endocrinol. 2025;13:221–62.
Busetto L, Dicker D, Frühbeck G, Halford JCG, Sbraccia P, Yumuk V, et al. A new framework for the diagnosis, staging and management of obesity in adults. Nat Med. 2024;30:2395–9.
Yumuk V, Frühbeck G, Oppert JM, Woodward E, Toplak H. An EASO position statement on multidisciplinary obesity management in adults. Obes Facts. 2014;7:96–101.
Yumuk V, Tsigos C, Fried M, Schindler K, Busetto L, Micic D, et al. European Guidelines for Obesity Management in Adults. Obes Facts. 2015;8:402–24.
McGowan BM. A practical guide to engaging individuals with obesity. Obes Facts. 2016;9:182–92.
Estrada-Restrepo A, Deossa-Restrepo GC, Benjumea-Rincón MV, Giraldo-Giraldo NA. [Sociodemographic and dietary factors and health conditions: determinants of malnutrition in the elderly in Colombia]. Cad Saude Publica. 2024;40:e00189423.
Dierckx de Casterlé B, Gastmans C, Bryon E, Denier Y. QUAGOL: a guide for qualitative data analysis. Int J Nurs Stud. 2012;49:360–71.
Aronne LJ, Hall KD, M Jakicic J, Leibel RL, Lowe MR, Rosenbaum M, et al. Describing the Weight-Reduced State: Physiology, Behavior, and Interventions. Obes (Silver Spring). 2021;29:S9–s24.
Bellicha A, van Baak MA, Battista F, Beaulieu K, Blundell JE, Busetto L, et al. Effect of exercise training on weight loss, body composition changes, and weight maintenance in adults with overweight or obesity: an overview of 12 systematic reviews and 149 studies. Obes Rev. 2021;22:e13256.
Dombrowski SU, Knittle K, Avenell A, Araújo-Soares V, Sniehotta FF. Long term maintenance of weight loss with non-surgical interventions in obese adults: systematic review and meta-analyses of randomised controlled trials. BMJ. 2014;348:g2646.
McPherson R. Genetic contributors to obesity. Can J Cardiol. 2007;23:23a–7a.
Velazquez A, Apovian CM. Updates on obesity pharmacotherapy. Ann N Y Acad Sci. 2018;1411:106–19.
Jackson Leach R, Powis J, Baur LA, Caterson ID, Dietz W, Logue J, et al. Clinical care for obesity: a preliminary survey of sixty-eight countries. Clin Obes. 2020;10:e12357.
Hassapidou M, Vlassopoulos A, Kalliostra M, Govers E, Mulrooney H, Ells L, et al. European Association for the Study of Obesity Position Statement on Medical Nutrition Therapy for the Management of Overweight and Obesity in Adults Developed in Collaboration with the European Federation of the Associations of Dietitians. Obes Facts. 2023;16:11–28.
Morgan-Bathke M, Raynor HA, Baxter SD, Halliday TM, Lynch A, Malik N, et al. Medical nutrition therapy interventions provided by dietitians for adult overweight and obesity management: an academy of nutrition and dietetics evidence-based practice guideline. J Acad Nutr Diet. 2023;123:520–45.e10.
Tsigos C, Hainer V, Basdevant A, Finer N, Mathus-Vliegen E, Micic D, et al. Criteria for EASO-collaborating centres for obesity management. Obes Facts. 2011;4:329–33.
Puhl RM, Heuer CA. Obesity stigma: important considerations for public health. Am J Public Health. 2010;100:1019–28.
Rubino, Puhl F, Cummings DE RM, Eckel RH, Ryan DH, Mechanick JI, et al. Joint international consensus statement for ending stigma of obesity. Nat Med. 2020;26:485–97.
Lim S, Oh B, Lee SH, Kim YH, Ha Y, Kang JH. Perceptions, attitudes, behaviors, and barriers to effective obesity care in South Korea: results from the ACTION-IO Study. J Obes Metab Syndr. 2020;29:133–42.
Janson A, Järvholm K, Sjögren L, Dahlgren J, Beamish AJ, Gronowitz E, et al. Metabolic and bariatric surgery in adolescents: for whom, when, and how?. Horm Res Paediatr. 2023;96:609–19.
Beamish AJ, Ryan Harper E, Järvholm K, Janson A, Olbers T. Long-term outcomes following adolescent metabolic and bariatric surgery. J Clin Endocrinol Metab. 2023;108:2184–92.
Eisenberg D, Shikora SA, Aarts E, Aminian A, Angrisani L, Cohen RV, et al. 2022 American Society of Metabolic and Bariatric Surgery (ASMBS) and International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) Indications for Metabolic and Bariatric Surgery. Obes Surg. 2023;33:3–14.
Casimiro Pérez JA, Fernández Quesada C, Del Val Groba Marco M, Arteaga González I, Cruz Benavides F, Ponce J, et al. Obesity Surgery Score (OSS) for Prioritization in the Bariatric Surgery Waiting List: a Need of Public Health Systems and a Literature Review. Obes Surg. 2018;28:1175–84.
Gregory DM, Temple Newhook J, Twells LK. Patients’ perceptions of waiting for bariatric surgery: a qualitative study. Int J Equity Health. 2013;12:86.
Arteaga-González IJ, Martín-Malagón AI, Ruiz de Adana JC, de la Cruz Vigo F, Torres-García AJ, Carrillo-Pallares AC. Bariatric Surgery Waiting Lists in Spain. Obes Surg. 2018;28:3992–6.
Behandeling obesitas Flowchart huisarts. Belgian Association for the study of Obesity; 2022.
Oppert JM, Bellicha A, van Baak MA, Battista F, Beaulieu K, Blundell JE, et al. Exercise training in the management of overweight and obesity in adults: synthesis of the evidence and recommendations from the European Association for the Study of Obesity Physical Activity Working Group. Obes Rev. 2021;22:e13273.
Kitzinger J. Qualitative research. Introducing focus groups. BMJ. 1995;311:299–302.
Acknowledgements
We extend our gratitude to all the patients who participated in the interviews.
Funding
We acknowledge financial support from Eli Lilly and Company. This funding source had no role in the design of this study and did not have any role during its execution, analyses, interpretation of the data, preparation of the manuscript or the decision to submit results for publication.
Author information
Authors and Affiliations
Contributions
LS: conceptualisation, formal analysis, funding acquisition, methodology, project administration, resources, validation, visualisation, writing original draft. CdeS: conceptualisation, investigation, project administration, resources, validation, visualisation, writing original draft. EG: conceptualisation, investigation, project administration, resources, validation, visualisation, writing original draft, writing review & editing. DU: conceptualisation, investigation, project administration, resources, validation, visualisation, writing original draft. MS: conceptualisation, investigation, project administration, resources, validation, visualisation, writing original draft. Nele Steenackers: conceptualisation, investigation, project administration, resources, validation, visualisation, writing original draft. SP: conceptualisation, investigation, project administration, resources, validation, visualisation, writing original draft. Inge Gies: conceptualisation, investigation, project administration, resources, validation, visualisation, writing original draft. BVderS: conceptualisation, investigation, project administration, resources, validation, visualisation, writing original draft. DDeC: conceptualisation, data curation, formal analysis, funding acquisition, investigation, project administration, methodology, resources, validation, visualisation, writing original draft, writing review & editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Schreurs, L., De Smedt, C., Goris, E. et al. “Just put in a little more effort”: the help-seeking experience of patients living with obesity. Int J Obes 49, 2062–2069 (2025). https://doi.org/10.1038/s41366-025-01867-6
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41366-025-01867-6