Abstract
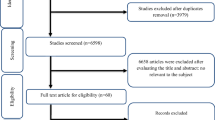
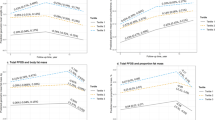
The effect of fluoxetine administration on body weight (BW), waist circumference (WC), and body mass index (BMI) remains inconclusive, as many studies have reported contradicting results. We conducted a meta-analysis of randomized controlled trials (RCTs) to assess the impact of fluoxetine prescription on these anthropometric indices. A comprehensive systematic review was conducted in PubMed/MEDLINE, SCOPUS, Web of Science, and EMBASE for manuscripts indexed before Jun 28st, 2025. The results were computed using the DerSimonian and Laird random effects model and reported as weighted mean differences (WMD) with 95% confidence intervals (CI). The current meta-analysis included 22 RCT arms (2348 individuals: placebo = 1166; fluoxetine = 1182) on BW, 2 RCT arms (77 individuals: placebo = 39; fluoxetine = 38) on WC, and 4 RCT arms (215 individuals: placebo = 105; fluoxetine = 110) on BMI. The present meta-analysis included 22 RCT arms (2348 individuals: placebo = 1166; fluoxetine = 1182) on BW. Fluoxetine treatment significantly reduced BW (WMD: −2.095 kg, p < 0.001), with significant heterogeneity noted among the RCTs (I² = 84.7%, P < 0.001). Fluoxetine supplementation decreased BW more substantially when the dose was ≥60 mg/day (WMD: −2.759 kg, p < 0.001) compared to <60 mg/day (WMD: −1.017 kg, p = 0.001), in trials lasting ≤12 weeks (WMD: −3.000 kg, p < 0.001) versus >12 weeks (WMD: −1.114 kg, p = 0.047), and when administered to individuals living with obesity (WMD: −2.246 kg, p < 0.001) compared to those living with overweight (WMD: −1.972 kg, p < 0.001). Fluoxetine did not impact WC or BMI values. Fluoxetine administration is associated with a reduction in BW, particularly when prescribed at doses ≥60 mg/day, during short-term interventions (≤3 months), and in individuals living with obesity.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this published article, and you can find these data in references.
Change history
29 October 2025
In this article a wrong version of supplementary file 3 was uploaded
References
Selman A, Dai J, Driskill J, Reddy AP, Reddy PH. Depression and obesity: focus on factors and mechanistic links. Biochim Biophys Acta Mol Basis Dis. 2025;1871:167561.
Goodwin RD, Dierker LC, Wu M, Galea S, Hoven CW, Weinberger AH. Trends in U.S. depression prevalence from 2015 to 2020: the widening treatment gap. Am J Prev Med. 2022;63:726–33.
Malhi GS, Bell E, Singh AB, Bassett D, Berk M, Boyce P, et al. The 2020 Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for mood disorders: major depression summary. Bipolar Disord. 2020;22:788–804.
Ampuero E, Luarte A, Flores FS, Soto AI, Pino C, Silva V, et al. The multifaceted effects of fluoxetine treatment on cognitive functions. Front Pharmacol. 2024;15:1412420.
Edinoff AN, Akuly HA, Hanna TA, Ochoa CO, Patti SJ, Ghaffar YA, et al. Selective serotonin reuptake inhibitors and adverse effects: a narrative review. Neurol Int. 2021;13:387–401.
Liu D, Guo T, Peng Q, Velu P, Prabahar K, Safargar M, et al. The effect of Fluoxetine on lipid profiles in overweight or obese Individuals: a systematic review and meta-analysis of randomized controlled trials. Diabetes Res Clin Pract. 2025;222:112040.
Ádám D, Arany J, Tóth KF, Póliska S, Váradi J, Kolozsi P, et al. Fluoxetine exerts anti-proliferative effect in human epidermal keratinocytes. Arch Dermatol Res. 2025;317:277.
Bougea A, Angelopoulou E, Vasilopoulos E, Gourzis P, Papageorgiou S. Emerging therapeutic potential of fluoxetine on cognitive decline in Alzheimer’s disease: systematic review. Int J Mol Sci. 2024;25:6542.
Fleetwood KJ, Guthrie B, Jackson CA, Kelly PAT, Mercer SW, Morales DR, et al. Depression and physical multimorbidity: a cohort study of physical health condition accrual in UK Biobank. PLoS Med. 2025;22:e1004532.
Walrave R, Beerten SG, Mamouris P, Coteur K, Van Nuland M, Van Pottelbergh G, et al. Trends in the epidemiology of depression and comorbidities from 2000 to 2019 in Belgium. BMC Prim Care. 2022;23:163.
Li Y, Du X, Shi S, Chen M, Wang S, Huang Y, et al. Trends in prevalence and multimorbidity of metabolic, cardiovascular, and chronic kidney diseases among US adults with depression from 2005 to 2020. J Affect Disord. 2025;372:262–8.
Patist CM, Stapelberg NJC, Du Toit EF, Headrick JP. The brain-adipocyte-gut network: linking obesity and depression subtypes. Cogn Affect Behav Neurosci. 2018;18:1121–44.
Milaneschi Y, Simmons WK, van Rossum EFC, Penninx BW. Depression and obesity: evidence of shared biological mechanisms. Mol Psychiatry. 2019;24:18–33.
Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW, et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67:220–9.
Mouawad M, Nabipur L, Agrawal DK. Impact of antidepressants on weight gain: underlying mechanisms and mitigation strategies. Arch Clin Biomed Res. 2025;9:183–95.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Reprint—Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Phys Ther. 2009;89:873–80.
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Borenstein M, Hedges LV, Higgins JP, Rothstein HR. Introduction to meta-analysis. Chichester, UK: John Wiley & Sons; 2011.
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13.
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34.
Zhang J. The bidirectional relationship between body weight and depression across gender: a simultaneous equation approach. Int J Environ Res Public Health. 2021;18:7673.
Carter A, Hoang N, Gilbert P, Kirby JN. Body weight perception outweighs body weight when predicting shame, criticism, depression and anxiety for lower BMI range and higher BMI range adults. J Health Psychol. 2022;27:2276–90.
Paulitsch RG, Demenech LM, Dumith SC. Association of depression and obesity is mediated by weight perception. J Health Psychol. 2021;26:2020–30.
Fuller NR, Burns J, Sainsbury A, Horsfield S, da Luz F, Zhang S, et al. Examining the association between depression and obesity during a weight management programme. Clin Obes. 2017;7:354–9.
Cao J, Chen Z, Wang Y, Ma Y, Yang Z, Cai J, et al. Overweight and glucose/lipid metabolism abnormality associated with SSRIs: a pharmacovigilance study based on the FDA adverse event reporting system. Front Pharmacol. 2024;15:1517546.
Serralde-Zuñiga AE, González-Garay AG, Rodríguez-Carmona Y, Meléndez-Mier G. Use of fluoxetine to reduce weight in adults with overweight or obesity: abridged republication of the cochrane systematic review. Obes Facts. 2022;15:473–86.
Choi YJ, Choi CY, Kim CU, Shin S. A nationwide pharmacovigilance investigation on trends and seriousness of adverse events induced by anti-obesity medication. J Glob Health. 2023;13:04095.
Garin P, Favre L, Vionnet N, Frantz J, Eap CB, Vandenberghe F. The influence of a Roux-en-Y gastric bypass on plasma concentrations of antidepressants. Obes Surg. 2023;33:1422–30.
Sun BK, Kim JH, Choi JS, Hwang SJ, Sung JH. Fluoxetine decreases the proliferation and adipogenic differentiation of human adipose-derived stem cells. Int J Mol Sci. 2015;16:16655–68.
Petimar J, Young JG, Yu H, Rifas-Shiman SL, Daley MF, Heerman WJ, et al. Medication-induced weight change across common antidepressant treatments: a target trial emulation study. Ann Intern Med. 2024;177:993–1003.
Sohel AJ, Shutter MC, Patel P, Molla M. Fluoxetine, in StatPearls. Treasure Island (FL): StatPearls Publishing; 2024.
FLUOXETINE oral | MSF medical guidelines. Médecins Sans Frontières; 2025. Available from: https://medicalguidelines.msf.org/en/viewport/EssDr/english/fluoxetine-oral-16683693.html.
Author information
Authors and Affiliations
Contributions
The authors’ contributions were as follows: FC, MS, JD and HK-V carried out the research, data analysis, and statistical assessment. FC, FD, ZY, JD and M-AG were involved in writing and structuring the manuscript. JD and HK-V took part in designing the research. FC, FD, ZY and JD were responsible for revising the manuscript. All authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cui, F., Dong, F., Yang, Z. et al. The effects of fluoxetine on body weight, waist circumference, and body mass index in individuals who are overweight or have obesity: a meta-analysis of randomized controlled trials. Int J Obes 49, 2446–2452 (2025). https://doi.org/10.1038/s41366-025-01891-6
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41366-025-01891-6