Abstract
Background
Animal studies provide evidence of a link between exosome profile, obesity and insulin resistance (IR). Although it is known that exosomes mediate cell-cell communication via their macromolecular cargo, the genetic factors regulating exosomes in humans are largely unknown.
Methods
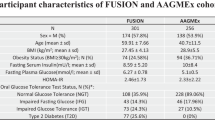
Leveraging genome-wide expression and genotype data from the African American Genetics of expression and Metabolism (AAGMEx) cohort, we focused on 262 genes in “Exosome pathway”, curated by us, to examine the relationship of the expression of these genes with IR and obesity and tested the role of single nucleotide polymorphisms (SNPs) in determining the variability in the expression of these genes in adipose and muscle tissue. Publicly available gene expression data on European ancestry individuals, genome-wide association studies (GWAS), and bioinformatic approaches were used to validate the role of obesity-associated genetic variants in regulating exosome pathway genes.
Results
Transcript levels of 96 and 15 exosome pathway genes were associated with gluco-metabolic traits (BMI and insulin sensitivity) in adipose and muscle tissue, respectively. Data also suggest transancestral replication of association. The cis-expression quantitative trait (cis-eQTL) analysis of exosome pathway genes identified 45 and 65 cis-eGenes in adipose and muscle tissue, respectively. Expression of a subset of 26 cis-eGenes in adipose was also associated with gluco-metabolic traits. Based on combined SNP-to-gene-linking analysis 35 and 82 adipose expressed exosomal genes (e.g. AHNAK, RAP2A) were identified as target genes for gluco-metabolic trait-associated SNPs in GWAS catalogue and UKBB GWAS datasets, respectively.
Conclusions
The expression of exosome pathway genes in adipose and muscle tissue are associated with obesity and IR, and expression of a subset of these genes are determined by SNPs. Furthermore, analysis of target genes of GWAS identified gluco-metabolic trait-associated SNPs suggests that a subset of these SNPs is potentially involved in causing obesity and related gluco-metabolic diseases, likely by modulating exosome biogenesis.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request. Other information on data availability in public databases is included in the “Methods” section.
References
Xourafa G, Korbmacher M, Roden M. Inter-organ crosstalk during development and progression of type 2 diabetes mellitus. Nat Rev Endocrinol. 2024;20:27–49.
Hu S, Hu Y, Yan W. Extracellular vesicle-mediated interorgan communication in metabolic diseases. Trends Endocrinol Metab. 2023;34:571–82.
Raposo G, Stahl PD. Extracellular vesicles, genetic programmers. Nat Cell Biol. 2024;26:22–3.
Valadi H, Ekström K, Bossios A, Sjöstrand M, Lee JJ, Lötvall JO. Exosome-mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells. Nat Cell Biol. 2007;9:654–9.
Whitham M, Parker BL, Friedrichsen M, Hingst JR, Hjorth M, Hughes WE, et al. Extracellular vesicles provide a means for tissue crosstalk during exercise. Cell Metab. 2018;27:237–51.e4.
Jeppesen DK, Fenix AM, Franklin JL, Higginbotham JN, Zhang Q, Zimmerman LJ, et al. Reassessment of exosome composition. Cell. 2019;177:428–45.e18.
Welsh JA, Goberdhan DCI, O’Driscoll L, Buzas EI, Blenkiron C, Bussolati B, et al. Minimal information for studies of extracellular vesicles (MISEV2023): from basic to advanced approaches. J Extracell Vesicles. 2024;13:e12404.
van der Pol E, Boing AN, Harrison P, Sturk A, Nieuwland R. Classification, functions, and clinical relevance of extracellular vesicles. Pharmacol Rev. 2012;64:676–705.
Eissa S, Matboli M, Aboushahba R, Bekhet MM, Soliman Y. Urinary exosomal microRNA panel unravels novel biomarkers for diagnosis of type 2 diabetic kidney disease. J Diab Complications. 2016;30:1585–92.
Schlaepfer IR, Nambiar DK, Ramteke A, Kumar R, Dhar D, Agarwal C, et al. Hypoxia induces triglycerides accumulation in prostate cancer cells and extracellular vesicles supporting growth and invasiveness following reoxygenation. Oncotarget. 2015;6:22836–56.
Ramteke A, Ting H, Agarwal C, Mateen S, Somasagara R, Hussain A, et al. Exosomes secreted under hypoxia enhance invasiveness and stemness of prostate cancer cells by targeting adherens junction molecules. Mol Carcinog. 2015;54:554–65.
de Jong OG, Verhaar MC, Chen Y, Vader P, Gremmels H, Posthuma G. et al. Cellular stress conditions are reflected in the protein and RNA content of endothelial cell-derived exosomes. J Extracell Vesicles. 2012;1:18396.
Isaac R, Reis FCG, Ying W, Olefsky JM. Exosomes as mediators of intercellular crosstalk in metabolism. Cell Metab. 2021;33:1744–62.
Kulaj K, Harger A, Bauer M, Caliskan ÖS, Gupta TK, Chiang DM, et al. Adipocyte-derived extracellular vesicles increase insulin secretion through transport of insulinotropic protein cargo. Nat Commun. 2023;14:709.
Blandin A, Amosse J, Froger J, Hilairet G, Durcin M, Fizanne L, et al. Extracellular vesicles are carriers of adiponectin with insulin-sensitizing and anti-inflammatory properties. Cell Rep. 2023;42:112866.
Wang J, Li L, Zhang Z, Zhang X, Zhu Y, Zhang C, et al. Extracellular vesicles mediate the communication of adipose tissue with brain and promote cognitive impairment associated with insulin resistance. Cell Metab. 2022;34:1264–79.e8.
Jafari N, Kolla M, Meshulam T, Shafran JS, Qiu Y, Casey AN, et al. Adipocyte-derived exosomes may promote breast cancer progression in type 2 diabetes. Sci Signal. 2021;14:eabj2807.
Ying W, Gao H, Dos Reis FCG, Bandyopadhyay G, Ofrecio JM, Luo Z, et al. MiR-690, an exosomal-derived miRNA from M2-polarized macrophages, improves insulin sensitivity in obese mice. Cell Metab. 2021;33:781–90.e5.
Crewe C, Joffin N, Rutkowski JM, Kim M, Zhang F, Towler DA, et al. An endothelial-to-adipocyte extracellular vesicle axis governed by metabolic state. Cell. 2018;175:695–708.e13.
Mishra S, Kumar A, Kim S, Su Y, Singh S, Sharma M, et al. A liquid biopsy-based approach to isolate and characterize adipose tissue-derived extracellular vesicles from blood. ACS Nano. 2023;17:10252–68.
Connolly KD, Wadey RM, Mathew D, Johnson E, Rees DA, James PE. Evidence for adipocyte-derived extracellular vesicles in the human circulation. Endocrinology. 2018;159:3259–67.
Guescini M, Canonico B, Lucertini F, Maggio S, Annibalini G, Barbieri E, et al. Muscle releases alpha-sarcoglycan positive extracellular vesicles carrying miRNAs in the bloodstream. PLoS ONE. 2015;10:e0125094.
Rigamonti AE, Bollati V, Pergoli L, Iodice S, De Col A, Tamini S, et al. Effects of an acute bout of exercise on circulating extracellular vesicles: tissue-, sex-, and BMI-related differences. Int J Obes. 2020;44:1108–18.
Arya SB, Collie SP, Parent CA. The ins-and-outs of exosome biogenesis, secretion, and internalization. Trends Cell Biol. 2024;34:90–108.
Gurung S, Perocheau D, Touramanidou L, Baruteau J. The exosome journey: from biogenesis to uptake and intracellular signalling. Cell Commun Signal. 2021;19:47.
Kalluri R, LeBleu VS. The biology, function, and biomedical applications of exosomes. Science. 2020;367:eaau6977.
Krylova SV, Feng D. The machinery of exosomes: biogenesis, release, and uptake. Int J Mol Sci. 2023;24:1337.
Lee YJ, Shin KJ, Chae YC. Regulation of cargo selection in exosome biogenesis and its biomedical applications in cancer. Exp Mol Med. 2024;56:877–89.
Mathieu M, Martin-Jaular L, Lavieu G, Théry C. Specificities of secretion and uptake of exosomes and other extracellular vesicles for cell-to-cell communication. Nat Cell Biol. 2019;21:9–17.
Guo BB, Bellingham SA, Hill AF. The neutral sphingomyelinase pathway regulates packaging of the prion protein into exosomes. J Biol Chem. 2015;290:3455–67.
Hessvik NP, Llorente A. Current knowledge on exosome biogenesis and release. Cell Mol Life Sci. 2018;75:193–208.
Lark DS, LaRocca TJ. Expression of exosome biogenesis genes is differentially altered by aging in the mouse and in the human brain during Alzheimer’s disease. J Gerontol A Biol Sci Med Sci. 2022;77:659–63.
Orrù V, Virdis F, Marongiu M, Serra V, Schlessinger D, Devoto M. et al. Effect of genetic factors, age and sex on levels of circulating extracellular vesicles and platelets. Int J Mol Sci. 2023;24:7183.
Riva P, Battaglia C, Venturin M. Emerging role of genetic alterations affecting exosome biology in neurodegenerative diseases. Int J Mol Sci. 2019;20:4113.
Wang J, Barr MM, Wehman AM. Extracellular vesicles. Genetics. 2024;227:iyae088.
Sajuthi SP, Sharma NK, Chou JW, Palmer ND, McWilliams DR, Beal J, et al. Mapping adipose and muscle tissue expression quantitative trait loci in African Americans to identify genes for type 2 diabetes and obesity. Hum Genet. 2016;135:869–80.
Sharma NK, Sajuthi SP, Chou JW, Calles-Escandon J, Demons J, Rogers S, et al. Tissue-specific and genetic regulation of insulin sensitivity-associated transcripts in African Americans. J Clin Endocrinol Metab. 2016;101:1455–68.
Boston RC, Stefanovski D, Moate PJ, Sumner AE, Watanabe RM, Bergman RN. MINMOD Millennium: a computer program to calculate glucose effectiveness and insulin sensitivity from the frequently sampled intravenous glucose tolerance test. Diab Technol Ther. 2003;5:1003–15.
Alexander DH, Novembre J, Lange K. Fast model-based estimation of ancestry in unrelated individuals. Genome Res. 2009;19:1655–64.
Sharma NK, Chuang Key CC, Civelek M, Wabitsch M, Comeau ME, Langefeld CD, et al. Genetic regulation of enoyl-CoA hydratase domain-containing 3 in adipose tissue determines insulin sensitivity in African Americans and Europeans. Diabetes. 2019;68:1508–22.
Brotman SM, El-Sayed Moustafa JS, Guan L, Broadaway KA, Wang D, Jackson AU, et al. Adipose tissue eQTL meta-analysis highlights the contribution of allelic heterogeneity to gene expression regulation and cardiometabolic traits. Nat Genet. 2025;57:180–92.
Civelek M, Wu Y, Pan C, Raulerson CK, Ko A, He A, et al. Genetic regulation of adipose gene expression and cardio-metabolic traits. Am J Hum Genet. 2017;100:428–43.
Taylor DL, Jackson AU, Narisu N, Hemani G, Erdos MR, Chines PS, et al. Integrative analysis of gene expression, DNA methylation, physiological traits, and genetic variation in human skeletal muscle. Proc Natl Acad Sci USA. 2019;116:10883–8.
Ghosh S, Bouchard C. Considerations on efforts needed to improve our understanding of the genetics of obesity. Int J Obes. 2025;49:206–10.
Gazal S, Weissbrod O, Hormozdiari F, Dey KK, Nasser J, Jagadeesh KA, et al. Combining SNP-to-gene linking strategies to identify disease genes and assess disease omnigenicity. Nat Genet. 2022;54:827–36.
Weeks EM, Ulirsch JC, Cheng NY, Trippe BL, Fine RS, Miao J, et al. Leveraging polygenic enrichments of gene features to predict genes underlying complex traits and diseases. Nat Genet. 2023;55:1267–76.
Zhai R, Pan L, Yang Z, Li T, Ning Z, Pawitan Y, et al. Genetic and phenotypic links between obesity and extracellular vesicles. Hum Mol Genet. 2022;31:3643–51.
Bouchard C. Genetics of obesity: what we have learned over decades of research. Obesity. 2021;29:802–20.
Loos RJF, Yeo GSH. The genetics of obesity: from discovery to biology. Nat Rev Genet. 2022;23:120–33.
Sinha S, Hoshino D, Hong NH, Kirkbride KC, Grega-Larson NE, Seiki M, et al. Cortactin promotes exosome secretion by controlling branched actin dynamics. J Cell Biol. 2016;214:197–213.
Ostrowski M, Carmo NB, Krumeich S, Fanget I, Raposo G, Savina A, et al. Rab27a and Rab27b control different steps of the exosome secretion pathway. Nat Cell Biol. 2010;12:19–30.
Valentine JM, Ahmadian M, Keinan O, Abu-Odeh M, Zhao P, Zhou X. et al. β3-Adrenergic receptor downregulation leads to adipocyte catecholamine resistance in obesity. J Clin Invest. 2022;132:e153357.
Dong SS, Duan YY, Zhu RJ, Jia YY, Chen JX, Huang XT, et al. Systematic functional characterization of non-coding regulatory SNPs associated with central obesity. Am J Hum Genet. 2025;112:116–34.
Kim YN, Shin JH, Kyeong DS, Cho SY, Kim MY, Lim HJ, et al. Ahnak deficiency attenuates high-fat diet-induced fatty liver in mice through FGF21 induction. Exp Mol Med. 2021;53:468–82.
Woo JK, Shin JH, Lee SH, Park HM, Cho SY, Sung YM, et al. Essential role of Ahnak in adipocyte differentiation leading to the transcriptional regulation of Bmpr1α expression. Cell Death Dis. 2018;9:864.
Silva TA, Smuczek B, Valadão IC, Dzik LM, Iglesia RP, Cruz MC, et al. AHNAK enables mammary carcinoma cells to produce extracellular vesicles that increase neighboring fibroblast cell motility. Oncotarget. 2016;7:49998–50016.
Acknowledgements
We thank the investigators, staff, and participants of the AAGMEx cohort for their valuable contributions. Computations were performed using the Wake Forest University (WFU) High Performance Computing Facility (DEAC HPC). Clinical and genomic studies in the AAGMEx cohort were supported by National Institutes of Health NIH/NIDDK grant R01 DK090111 and R01 DK118243 (PI: SKD). The authors also thank the METSIM, FUSION, and other study investigators for publicly sharing their data.
Author information
Authors and Affiliations
Contributions
SKD conceptualized and designed the study; SKD collected data; MEC and CDL analyzed the data; SKD, GD, and CDL interpreted results; SKD wrote and finalized the manuscript; all authors read, edited, and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
GD is the founder of LiBiCo LLC, which has no influence or contribution to the work presented in this manuscript. Other authors have no conflict of interest.
Ethics approval and consent to participate
All participants in the AAGMEx cohort provided written informed consent under protocols approved by the Institutional Review Board (IRB) at Wake Forest University Health Sciences (Human Protocol: IRB00015775). The IRB reviewed all research involving humans to ensure that studies are conducted in accordance with the ethical standards put forward by the Belmont Report, and federal, state, and local regulations, and policies governing human research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Das, S.K., Deep, G., Comeau, M.E. et al. Genetic regulation of exosome biogenesis pathway in human adipose and muscle tissue and association with obesity and insulin resistance. Int J Obes (2025). https://doi.org/10.1038/s41366-025-01933-z
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41366-025-01933-z