Abstract
Background
Magnet-assisted bariatric surgery (MABS) represents a novel advancement in minimally invasive surgical techniques. It addresses challenges associated with obesity-related anatomical complexities, such as hepatomegaly and fatty liver disease, by enhancing surgical exposure and site visualization.
Objectives
This systematic review aimed to: (1) compare the efficacy of MABS and conventional bariatric surgery for weight loss and postoperative outcomes; (2) assess their safety profiles; and (3) evaluate perioperative recovery, hospital stay, and patient-reported outcomes like quality of life and satisfaction.
Methods
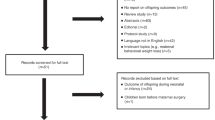
A comprehensive literature search was conducted across PubMed, Web of science, Google scholar and Cochrane databases. Data were extracted and synthesized to provide quantitative assessment of MABS’s performance.
Results
A total of 12 articles comprising 1305 participants were included. The findings confirmed MABS’s feasibility and safety, with significant advantages across varying BMI ranges. Notable benefits included improved surgical exposure, shorter or comparable operative times, reduced postoperative pain, shorter hospital stays, low complication rates and no procedure-related mortality.
Conclusion
MABS demonstrated strong potential as an innovative tool in minimally invasive bariatric surgery, offering significant benefits for both patients and surgical teams. Its ability to address obesity-related challenges and enhance surgical outcomes supports its continued use and refinement. Future research should focus on stratified analyses, long-term outcomes, and economic evaluations to establish standardized criteria for patient selection and expand its applicability to other minimally invasive procedures.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Das S, Debnath M, Das S, Sarkar S, Rumana AS. Association of overweight and obesity with hypertension, diabetes and comorbidity among adults in Bangladesh: evidence from nationwide Demographic and Health Survey 2017–2018 data. BMJ Open. 2022;12:e052822.
Alterki A, Abu-Farha M, Al Shawaf E, Al-Mulla F, Abubaker J. Investigating the Relationship between Obstructive Sleep Apnoea, Inflammation and Cardio-Metabolic Diseases. Int J Mol Sci. 2023;24:6807.
World Health Organization (WHO). Obesity and overweight. World Health Organization; 2025. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
Courcoulas AP, Daigle CR, Arterburn DE. Long term outcomes of metabolic/bariatric surgery in adults. BMJ. 2023;383:e071027.
Davis M, Davalos G, Ortega C, Chen S, Schimpke S, Jain-Spangler K, et al. Magnetic Liver Retraction: an Incision-Less Approach for Less Invasive Bariatric Surgery. Obes Surg. 2019;29:1068–73.
Cadière G-B, Poras M, Maréchal M-T, Pau L, Muteganya R, Gossum MV, et al. Sleeve gastrectomy with duodenoileal bipartition using linear magnets: feasibility and safety at 1-year follow-up. J Gastrointest Surg. 2024;28:640–50.
Gagner M, Abuladze D, Koiava L, Buchwald JN, Van Sante N, Krinke T. First-in-Human Side-to-Side Magnetic Compression Duodeno-ileostomy with the Magnet Anastomosis System. Obes Surg. 2023;33:2282–92.
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73:712–6.
FDA. De novo classification request for levita magnetic surgical system. FDA; 2015. https://www.accessdata.fda.gov/cdrh_docs/reviews/DEN150007.pdf.
Haskins IN, Strong AT, Allemang MT, Bencsath KP, Rodriguez JH, Kroh MD. Magnetic surgery: first U.S. experience with a novel device. Surg Endosc. 2018;32:895–9.
C J. Medical-Grade Magnets for Implantable and Wearable Devices: Design, Safety, and Applications. Magnetstek. https://magnetstek.com/medical-grade-magnets-for-implantable-and-wearable-devices-design-safety-and-applications/#:~:text=,the%20lifespan%20of%20the%20device.
Luengas R, Galindo J, Castro M, Marambio A, Watkins G, Rodriguez del Rey M, et al. First prospective clinical trial of reduced incision bariatric procedures using magnetic liver retraction. Surg Obes Relat Dis. 2021;17:147–52.
Borjas G, Sánchez N, Urdaneta A, Maldonado A, Ramos E, Ferrigni C, et al. Magnetic device in reduced port and single port bariatric surgery: First 170 cases experience. Cir Esp. 2022;100:614–21.
Borjas G, Sánchez N, Urdaneta A, Maldonado A, Ramos E. Magnetic-Assisted Reduced-Port Sleeve Gastrectomy Versus Laparoscopic Sleeve Gastrectomy: a Comparative Study. Obes Surg. 2023;33:2261–5.
Romero-Velez G, Robles I, Jiménez J, Cabrera C, Luengas R, Portenier D, et al. Robotic Magnetic Surgery: Results From the First Prospective Clinical Trial. Ann Surg Open. 2022;3:e225.
Borjas G, Urdaneta A, Ramos E, Maldonado A. Magnetic liver retraction in bariatric surgery: Is it possible?. Cir Esp. 2024;102:331–4.
Gagner M, Almutlaq L, Cadiere G-B, Torres AJ, Sanchez-Pernaute A, Buchwald JN, et al. Side-to-side magnetic duodeno-ileostomy in adults with severe obesity with or without type 2 diabetes: early outcomes with prior or concurrent sleeve gastrectomy. Surg Obes Relat Dis. 2024;20:341–52.
Gagner M, Fried M, Michalsky D, Dolezalova K, Sramkova P, Brezina J, et al. First-in-Human Linear Magnetic Jejuno-Ileal Bipartition: Preliminary Results with Incisionless, Sutureless, Swallowable Technique. Obes Surg. 2025;35:2067–80.
Gagner M, Almutlaq L, Gnanhoue G, Buchwald JN. First-in-human side-to-side linear magnetic compression gastroileostomy: feasibility and early outcomes in adults with obesity. J Gastrointest Surg. 2025;29:102067.
Bhandari M, Neto MG, Brunaldi VO, Bhandari M, Mathor W, Reddy M, et al. Immediately-Patent Magnetic Duodeno-Ileal Anastomosis (IMPA-DI): The First-in-Human Study. Obes Surg. 2025;35:2053–8.
Liu R, Guo Y, Yin G, Tuo H, Zhu Y, Yang W, et al. Magnetic anchoring device assisted-laparoscopic sleeve gastrectomy versus conventional laparoscopic sleeve gastrectomy: A retrospective cohort study. Heliyon. 2024;10:e26875.
Welsh LK, Davalos G, Diaz R, Narvaez A, Perez JE, Castro M, et al. Magnetic Liver Retraction Decreases Postoperative Pain and Length of Stay in Bariatric Surgery Compared to Nathanson Device. J Laparoendoscopic Adv Surg Tech. 2021;31:194–202.
Hiramatsu K, Aoba T, Kamiya T, Mohri K, Kato T. Novel use of the Nathanson liver retractor to prevent postoperative transient liver dysfunction during laparoscopic gastrectomy. Asian J Endosc Surg. 2020;13:293–300.
Romero-Velez G, Portenier D, Roberts J, Oviedo RJ, Rodriguez-Navarro A, Kroh MD. Magnetic-assisted surgery: the road from laparoscopy to robotics. Mini Invasive Surg. 2022;6:56.
Nigicser I, Oldfield M, Haidegger T. Magnetic Anchoring Considerations for Retractors Supporting Manual and Robot-Assisted Minimally Invasive Surgery. Machines. 2022;10:745.
Bernier GV, Sanchez JE. Surgical simulation: the value of individualization. Surg Endosc. 2016;30:3191–7.
Tian B, Zhang M, Ren Y, Zhang Y, Lyu Y, Yan X. Clinical application of magnetic anchor technique in laparoscopic cholecystectomy: the first retrospective study in China. Front Surg. 2024;10:1335805.
Fulla J, Small A, Kaplan-Marans E, Palese M. Magnetic-Assisted Robotic and Laparoscopic Renal Surgery: Initial Clinical Experience with the Levita Magnetic Surgical System. J Endourol. 2020;34:1242–6.
Diaz R, Davalos G, Welsh LK, Portenier D, Guerron AD. Use of magnets in gastrointestinal surgery. Surg Endosc. 2019;33:1721–30.
Acknowledgements
I would like to extend my deepest gratitude to all the authors who supported and contributed to this research.
Funding
Zhiyong Dong was supported by “Guangzhou Science and Technology Plan Project (2024A03J1037)”. The funding bodies had no role in the study design, data collection, data analysis, data interpretation, the writing of the manuscript and the decision to submit the paper for publication. The corresponding authors had full access to all the data in the study and take responsibility for the decision to submit for publication.
Author information
Authors and Affiliations
Contributions
YC, SD, and YL conceptualized the study and drafted the initial manuscript. XZ, BW, and XZ were responsible for literature search and synthesis of findings. WC and ZD reviewed the results, and revised the initial draft. All authors critically reviewed and approved the final submitted version. WC and ZD are the guarantors of the work. The corresponding author confirms that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, Y., Shiliang, D., Liu, Y. et al. Current evidence and future perspectives on magnet-assisted bariatric surgery (MABS): a systematic review. Int J Obes (2025). https://doi.org/10.1038/s41366-025-01966-4
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41366-025-01966-4