Abstract
Objective
To evaluate the efficacy of a comprehensive cognitive intervention as an add-on to a standard behavioral weight-loss intervention (BWLI) in improving anthropometric measures in individuals with excess weight.
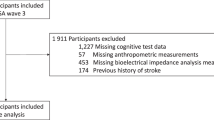
Participants
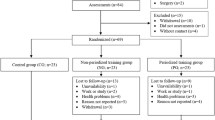
This randomized controlled trial included 148 participants (126 women; mean BMI = 31.62 kg/m²); 86.5% participants (n = 128) completed the study.
Methods
Participants were randomized into three groups: (1) Cognitive group (received four cognitive trainings: inhibitory control, approach-avoidance bias modification, implementation intentions, and episodic future thinking); (2) Sham group (received placebo cognitive interventions); and (3) Control group (no cognitive intervention). All three groups received BWLI. Cognitive trainings were delivered through four consecutive 90-min online group sessions. BMI, weight, percentage of weight loss (%WL), and waist-to-height ratio (WHtR) were assessed at baseline, post-treatment, and 3- and 6-month follow-ups. Mixed 3 (group) × 3 (time point) analysis were conducted to examine changes over time and between groups. Chi-squared test was used to explore group differences in reaching a clinically meaningful %WL.
Results
Significant group-by-time effects interactions were found for BMI (p = 0.009), weight (p = 0.003), %WL (p = 0.004) and WHtR (p = 0.041). Post hoc analyses showed greater reductions in all anthropometric measures in the Cognitive group compared to the Control group at post-intervention and at both follow-ups. Further, only the Cognitive group showed significant improvements over time. At 6-month follow-up, effect sizes were moderate in the Cognitive group, small in the Sham group, and negligible to small in the Control group. A higher proportion of participants in the Cognitive group achieved a clinically meaningful %WL.
Conclusions
A comprehensive cognitive training delivered as an add-on to BWLI improved anthropometric outcomes in individuals with excess weight, with sustained effects over 6 months.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets generated and analyzed during the current study are available on the Open Science Framework (OSF) at https://osf.io/wj38y.
References
Kluge, H. H. P. & Weltgesundheitsorganisation (Eds.). WHO European regional obesity report 2022. World Health Organization..
Delpino FM, dos Santos Rodrigues AP, Petarli GB, Machado KP, Flores TR, Batista SR, et al. Overweight, obesity and risk of multimorbidity: a systematic review and meta-analysis of longitudinal studies. Obes Rev. 2023;24:e13562.
Chong B, Jayabaskaran J, Kong G, Chan YH, Chin YH, Goh R, et al. Trends and predictions of malnutrition and obesity in 204 countries and territories: an analysis of the Global Burden of Disease Study 2019. eClinicalMedicine. 2023;57:101850.
Chu DT, Minh Nguyet NT, Nga VT, Thai Lien NV, Vo DD, Lien N, et al. An update on obesity: mental consequences and psychological interventions. Diabetes Metab Syndr Clin Res Rev. 2019;13:155–60.
Pearl RL. Weight bias and stigma: public health implications and structural solutions. Soc Issues Policy Rev. 2018;12:146–82.
Okunogbe A, Nugent R, Spencer G, Powis J, Ralston J, Wilding J. Economic impacts of overweight and obesity: current and future estimates for 161 countries. BMJ Glob Health. 2022;7:e009773.
Amiri S, Behnezhad S. Body mass index and risk of sick leave: a systematic review and meta-analysis. Clin Obes. 2019;9:e12334.
Wadden TA, Butryn ML. Behavioral treatment of obesity. Endocrinol Metab Clin North Am. 2003;32:981–1003.
Wadden TA, Volger S, Sarwer DB, Vetter ML, Tsai AG, Berkowitz RI, et al. A two-year randomized trial of obesity treatment in primary care practice. N Engl J Med. 2011;365:1969.
Sharma AM, Birney S, Crotty M, Finer N, Segal-Lieberman G, Vázquez-Velázquez V, et al. Determinants of adherence to obesity medication: a narrative review. Obes Rev. 2025;26:e13885.
Noria SF, Shelby RD, Atkins KD, Nguyen NT, Gadde KM. Weight regain after bariatric surgery: scope of the problem, causes, prevention, and treatment. Curr Diab Rep. 2023;23:31–42.
Appelhans BM. Neurobehavioral inhibition of reward-driven feeding: implications for dieting and obesity. Obesity. 2009;17:640–7.
Dakin C, Finlayson G, Stubbs RJ. Exploring the underlying psychological constructs of self-report eating behavior measurements: toward a comprehensive framework. Psychol Rev. 2024;132:1241–1265.
Yang Y, Shields GS, Wu Q, Liu Y, Chen H, Guo C. Cognitive training on eating behaviour and weight loss: a meta-analysis and systematic review. Obes Rev. 2019;20:1628–41.
Satyal MK, Basso JC, Tegge AN, Metpally AR, Bickel WK. Novel model of obesity prediction: neurobehaviors as targets for treatment. Behav Neurosci. 2021;135:426.
Kakoschke N, Hawker C, Castine B, de Courten B, Verdejo-Garcia A. Smartphone-based cognitive bias modification training improves healthy food choice in obesity: a pilot study. Eur Eat Disord Rev. 2018;26:526–32.
Adams RC, Button KS, Hickey L, Morrison S, Smith A, Bolus W, et al. Food-related inhibitory control training reduces food liking but not snacking frequency or weight in a large healthy adult sample. Appetite. 2021;167:105601.
Benyamini Y, Geron R, Steinberg DM, Medini N, Valinsky L, Endevelt R. A structured intentions and action-planning intervention improves weight loss outcomes in a group weight loss program. Am J Health Promot. 2013;28:119–27.
O’Neill J, Daniel TO, Epstein LH. Episodic future thinking reduces eating in a food court. Eat Behav. 2016;20:9–13.
Yang Y, Morys F, Wu Q, Li J, Chen H. Pilot study of food-specific go/no-go training for overweight individuals: brain imaging data suggest inhibition shapes food evaluation. Soc Cogn Affect Neurosci. 2023;18:nsab137.
Stapleton P, Bannatyne AJ, Urzi KC, Porter B, Sheldon T. Food for thought: a randomised controlled trial of emotional freedom techniques and cognitive behavioural therapy in the treatment of food cravings. Appl Psychol Health Well Being. 2016;8:232–57.
Mehl N, Mueller-Wieland L, Mathar D, Horstmann A. Retraining automatic action tendencies in obesity. Physiol Behav. 2018;192:50–8.
Turton R, Bruidegom K, Cardi V, Hirsch CR, Treasure J. Novel methods to help develop healthier eating habits for eating and weight disorders: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2016;61:132–55.
Bélanger-Gravel A, Godin G, Bilodeau A, Poirier P. The effect of implementation intentions on physical activity among obese older adults: a randomised control study. Psychol Health. 2013;28:217–33.
Armitage CJ, Norman P, Noor M, Alganem S, Arden MA. Evidence that a very brief psychological intervention boosts weight loss in a weight loss program. Behav Ther. 2014;45:700–7.
Forman EM, Manasse SM, Dallal DH, Crochiere RJ, Loyka CM, Butryn ML, et al. Computerized neurocognitive training for improving dietary health and facilitating weight loss. J Behav Med. 2019;42:1029–40.
Lawrence NS, O’Sullivan J, Parslow D, Javaid M, Adams RC, Chambers CD, et al. Training response inhibition to food is associated with weight loss and reduced energy intake. Appetite. 2015;95:17–28.
Veling H, van Koningsbruggen GM, Aarts H, Stroebe W. Targeting impulsive processes of eating behavior via the internet. Effects on body weight. Appetite. 2014;78:102–9.
Sze YY, Daniel TO, Kilanowski CK, Collins RL, Epstein LH. Web-based and mobile delivery of an episodic future thinking intervention for overweight and obese families: a feasibility study. JMIR MHealth UHealth. 2015;3:e4603.
Armitage CJ, Alganem S, Norman P. Randomized controlled trial of a volitional help sheet to encourage weight loss in the Middle East. Prev Sci. 2017;18:976–83.
Forcano L, Mata F, de la Torre R, Verdejo-Garcia A. Cognitive and neuromodulation strategies for unhealthy eating and obesity: systematic review and discussion of neurocognitive mechanisms. Neurosci Biobehav Rev. 2018;87:161–91.
Kaur T, Ranjan P, Kaloiya GS, Bhatia H, Prakash B, Singh A, et al. Effectiveness of cognitive retraining intervention on weight loss and lifestyle-related behaviours among adults: a systematic review and meta-analysis. Diabetes Metab Syndr Clin Res Rev. 2024;18:102969.
Semlitsch T, Stigler FL, Jeitler K, Horvath K, Siebenhofer A. Management of overweight and obesity in primary care—a systematic overview of international evidence-based guidelines. Obes Rev. 2019;20:1218–30.
Kakoschke N, Kemps E, Tiggemann M. The effect of combined avoidance and control training on implicit food evaluation and choice. J Behav Ther Exp Psychiatry. 2017;55:99–105.
Sweatt K, Garvey WT, Martins C. Strengths and limitations of BMI in the diagnosis of obesity: what is the path forward? Curr Obes Rep. 2024;13:584–95.
Rubino F, Cummings DE, Eckel RH, Cohen RV, Wilding JPH, Brown WA, et al. Definition and diagnostic criteria of clinical obesity. Lancet Diabetes Endocrinol. 2025. https://www.sciencedirect.com/science/article/pii/S2213858724003164.
Williamson DA, Bray GA, Ryan DH. Is 5% weight loss a satisfactory criterion to define clinically significant weight loss? Obesity. 2015;23:2319–20.
Stout RL, Wirtz PW, Carbonari JP, Del Boca FK. Ensuring balanced distribution of prognostic factors in treatment outcome research. J Stud Alcohol Suppl. 1994;12:70–5.
Bazzaz MM, Fadardi JS, Parkinson J. Efficacy of the attention control training program on reducing attentional bias in obese and overweight dieters. Appetite. 2017;108:1–11.
Aulbach MB, Knittle K, van Beurden SB, Haukkala A, Lawrence NS. App-based food Go/No-Go training: user engagement and dietary intake in an opportunistic observational study. Appetite. 2021;165:105315.
Miller WR, Rollnick S. Motivational interviewing: helping people change. 3rd ed. New York, NY, US: Guilford Press; 2013. xii, p 482.
Solier-López L, González-González R, Caracuel A, Kakoschke N, Lawrence N, Vilar-López R. A program for the comprehensive cognitive training of excess weight (TRAINEP): the study protocol for a randomized, controlled trial. Int J Environ Res Public Health. 2022;19:8447.
Hoaglin DC, Iglewicz B, Tukey JW. Performance of some resistant rules for outlier labeling. J Am Stat Assoc. 1986;81:991–9.
Cumming G. Understanding the new statistics: effect sizes, confidence intervals, and meta-analysis. New York: Routledge; 2013. p 536.
Lakens D. Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Front Psychol. 2013;4. https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2013.00863/full.
Navas JF, Verdejo-García A, Vadillo MA. The evidential value of research on cognitive training to change food-related biases and unhealthy eating behavior: a systematic review and p-curve analysis. Obes Rev. 2021;22:e13338.
VanWormer JJ, Martinez AM, Martinson BC, Crain AL, Benson GA, Cosentino DL, et al. Self-weighing promotes weight loss for obese adults. Am J Prev Med. 2009;36:70–3.
Stice E, Yokum S, Veling H, Kemps E, Lawrence NS. Pilot test of a novel food response and attention training treatment for obesity: brain imaging data suggest actions shape valuation. Behav Res Ther. 2017;94:60–70.
Rubino F, Batterham RL, Koch M, Mingrone G, le Roux CW, Farooqi IS, et al. Commission on the definition and diagnosis of clinical obesity. Lancet Diabetes Endocrinol. 2023;11:226–8.
Eguaras S, Toledo E, Buil-Cosiales P, Salas-Salvadó J, Corella D, Gutierrez-Bedmar M, et al. Does the Mediterranean diet counteract the adverse effects of abdominal adiposity? Nutr Metab Cardiovasc Dis. 2015;25:569–74.
Geng S, Chen X, Shi Z, Bai K, Shi S. Association of anthropometric indices with the development of multimorbidity in middle-aged and older adults: a retrospective cohort study. PLoS ONE. 2022;17:e0276216.
Lee CMY, Huxley RR, Wildman RP, Woodward M. Indices of abdominal obesity are better discriminators of cardiovascular risk factors than BMI: a meta-analysis. J Clin Epidemiol. 2008;61:646–53.
Nevill AM, Duncan MJ, Lahart IM, Sandercock GR. Scaling waist girth for differences in body size reveals a new improved index associated with cardiometabolic risk. Scand J Med Sci Sports. 2017;27:1470–6.
Wu Y, Li D, Vermund SH. Advantages and limitations of the body mass index (BMI) to assess adult obesity. Int J Environ Res Public Health. 2024;21:757.
Heymsfield SB, Wadden TA. Mechanisms, pathophysiology, and management of obesity. N Engl J Med. 2017. https://www.nejm.org/doi/full/10.1056/NEJMra1514009.
Nevill AM, Duncan MJ, Myers T. BMI is dead; long live waist-circumference indices: but which index should we choose to predict cardio-metabolic risk? Nutr Metab Cardiovasc Dis. 2022;32:1642–50.
US Preventive Services Task Force. Behavioral weight loss interventions to prevent obesity-related morbidity and mortality in adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2018;320:1163–71.
Eichen DM, Pasquale EK, Twamley EW, Boutelle KN. Targeting executive function for weight loss in adults with overweight or obesity. Physiol Behav. 2021;240:113540.
Collins LM. Optimization of behavioral, biobehavioral, and biomedical interventions: the Multiphase Optimization Strategy (MOST) [Internet]. Cham: Springer International Publishing; 2018. http://link.springer.com/10.1007/978-3-319-72206-1.
Acknowledgements
This study was supported by the organizations listed in the Funding section.
Funding
This work was carried out with support from the following grants and institutions: the TRAINEP project [grant RTI2018–098771-B-I00] funded by the Spanish Ministry of Science, Innovation, and Universities [MCIN/AEI/ 10.13039/501100011033] and the European Regional Development Fund “FEDER A way of making Europe”; the INHIBE project [grant PDI2022-137524OB-I00] funded by the Spanish Ministry of Science, Innovation, and Universities [MCIN/AEI/10.13039/501100011033] and the European Social Fund Plus (FSE+); the BE-NEMOIC project [grant P21_00776] funded by the Consejería de Universidad, Investigación e Innovación (Junta de Andalucía); the Mind, Brain and Behavior Research Center [Grant CEX2023-001312-M/ funded by MCIN/AEI /10.13039/501100011033 and Grant UCEPP2023-11 funded by University of Granada]; Formación de Profesorado Universitario [Contract FPU2020-04540 (RGG)] funded by the Spanish Ministry of Science, Innovation and Universities; Research stays in foreign centres funded by Ministry of Science, Innovation and Universities [grant EST25/00046 (RGG) and PRX22/00698 (AC)] and the University of Granada [Plan Propio de Investigación y Transferencia 2024-Programa 10 (RGG and LSL)].
Author information
Authors and Affiliations
Contributions
Lucía Solier-López: writing—original draft, data curation, formal analysis, investigation, and visualization. Raquel González-González: data curation, formal analysis, investigation, and writing—review and editing. Alfonso Caracuel: conceptualization, funding acquisition, methodology, project administration, supervision, validation, visualization, and writing—review and editing. Antonio Verdejo-García: conceptualization, methodology, resources, software, validation, visualization, and writing—review and editing. José A. Puertas-González: writing—review and editing. Raquel Vilar-López: conceptualization, funding acquisition, methodology, project administration, supervision, validation, visualization, and writing—review and editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Solier-López, L., González-González, R., Caracuel, A. et al. Comprehensive cognitive training improves anthropometric measures in people with excess weight: the TRAINEP randomized controlled trial. Int J Obes (2026). https://doi.org/10.1038/s41366-025-02012-z
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41366-025-02012-z