Abstract
Background
It’s pivotal to control the presence of legionella in sanitary structures. So, it’s important to determine the risk factors associated with Legionella colonization in health care centres. In recent years that is why new diagnostic techniques have been developed.
Objective
To evaluate risks factors for Legionella colonization using a novel and more sensitive Legionella positivity index.
Methods
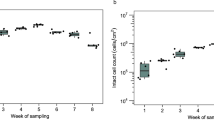
A total of 204 one-litre water samples (102 cold water samples and 102 hot water samples), were collected from 68 different sampling sites of the hospital water system and tested for Legionella spp. by two laboratories using culture, polymerase chain reaction and a method based on immunomagnetic separation (IMS). A Legionella positivity index was defined to evaluate Legionella colonization and associated risk factors in the 68 water samples sites. We performed bivariate analyses and then logistic regression analysis with adjustment of potentially confounding variables. We compared the performance of culture and IMS methods using this index as a new gold standard to determine if rapid IMS method is an acceptable alternative to the use of slower culture method.
Results
Based on the new Legionella positivity index, no statistically significant differences were found neither between laboratories nor between methods (culture, IMS). Positivity was significantly correlated with ambulatory health assistance (p = 0.05) and frequency of use of the terminal points. The logistic regression model revealed that chlorine (p = 0.009) and the frequency of use of the terminal points (p = 0.001) are predictors of Legionella colonization. Regarding this index, the IMS method proved more sensitive (69%) than culture method (65.4%) in hot water samples.
Significance
We showed that the frequency of use of terminal points should be considered when examining environmental Legionella colonization, which can be better evaluated using the provided Legionella positivity index. This study has implications for the prevention of Legionnaires’ disease in hospital settings.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
Data are available from the authors upon reasonable request and with permission from the Hospital Clínico Universitario de Valencia.
References
Kuiper MW, Wullings BA, Akkermans ADL, Beumer RR, Van Der Kooij D. Intracellular proliferation of legionella pneumophila in hartmannella vermiformis in aquatic biofilms grown on plasticized polyvinyl chloride. Appl Environ Microbiol. 2004;70:6826–33.
Buse HY, Schoen ME, Ashbolt NJ. Legionellae in engineered systems and use of quantitative microbial risk assessment to predict exposure. Water Res. 2012;46:921–33.
Hellinga JR, Gardu~ No RA, Kormish JD, Tanner JR, Khan D, Buchko K. et al. Identification of vacuoles containing extraintestinal differentiated forms of Legionella pneumophila in colonized Caenorhabditis elegans soil nematodes. Microbiologyopen. 2015;4:660–81.
Alleron L, Khemiri A, Koubar M, Lacombe C, Coquet L, Cosette P, et al. VBNC Legionella pneumophila cells are still able to produce virulence proteins. Water Res. 2013;47:6606–17.
Burillo A, Pedro-Botet ML, Bouza E. Microbiology and epidemiology of Legionnaire’s disease. Infect Dis Clin North Am. 2017;31:7–27.
Cunha BA, Burillo A, Bouza E. Legionnaires’ disease. In: The Lancet. Elsevier; 2016. p. 376–85.
Beauté J. The European Legionnaires’ Disease Surveillance Network on behalf of the ELDS. Legionnaires’ disease in Europe, 2011 to 2015. Euro Surveill. 2017;22:171116–1.
Neil K, Berkelman R. Increasing incidence of legionellosis in the United States, 1990–2005: changing epidemiologic trends. Clin Infect Dis. 2008;47:591–9.
Dooling KL, Toews K-A, Hicks LA, Garrison LE, Bachaus B, Zansky S, et al. Active bacterial core surveillance for Legionellosis - United States, 2011–2013. MMWR Morb Mortal Wkly Rep. 2015;64:1190–3.
Mercante JW, Winchell JM. Current and emerging Legionella diagnostics for laboratory and outbreak investigations. Clin Microbiol Rev. 2015;28:95–133.
Phin N, Parry-Ford F, Harrison T, Stagg HR, Zhang N, Kumar K, et al. Epidemiology and clinical management of Legionnaires’ disease. Lancet Infect Dis. 2014;14:1011–21.
St-Martin G, Uldum S, Mølbak K. Incidence and prognostic factors for Legionnaires’ Disease in Denmark 1993–2006. ISRN Epidemiol. 2013;2013:1–8.
von Baum H, Ewig S, Marre R, Suttorp N, Gonschior S, Welte T, et al. Community-acquired Legionella pneumonia: new insights from the German competence network for community acquired pneumonia. Clin Infect Dis. 2008;46:1356–64.
Beauté JulienBeaute J, Zucs P, de Jong B Legionnaires disease in Europe, 2009–2010. 18, Euro Surveill. 2013.
Cross KE, Mercante JW, Benitez AJ, Brown EW, Diaz MH, Winchell JM. Simultaneous detection of Legionella species and L. anisa, L. bozemanii, L. longbeachae and L. micdadei using conserved primers and multiple probes in a multiplex real-time PCR assay. Diagn Microbiol Infect Dis. 2016;85:295–301.
Yu VL, Plouffe JF, Pastoris MC, Stout JE, Schousboe M, Widmer A, et al. Distribution of Legionella species and serogroups isolated by culture in patients with sporadic community-acquired legionellosis: an international collaborative survey. J Infect Dis. 2002;186:127–8.
Rucinski SL, Murphy MP, Kies KD, Cunningham SA, Schuetz AN, Patel R. Eight years of clinical Legionella PCR testing illustrates a seasonal pattern. J Infect Dis. 2018;218:669–70.
Ecdc. Legionnaires’ disease Annual Epidemiological Report for 2018. Available from: https://www.ecdc.europa.eu/en/publications-data/legionnaires-disease-annual-epidemiological-report-2018
IIII de SC Weekly epidemiological bulletin (No. 4). 2020. Available from: https://www.isciii.es/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/Boletines/Documents/Boletin_Epidemiologico_en_red/boletines%20en%20red%202020/IS_N%c2%ba%204-200123-WEB.pdf
National Academies of Sciences E and M. Management of Legionella in Water Systems. Washington, D.C.: National Academies Press; 2019.
Montagna MT, De Giglio O, Cristina ML, Napoli C, Pacifico C, Agodi A, et al. Evaluation of Legionella air contamination in healthcare facilities by different sampling methods: An Italian multicenter study. Int J Environ Res Public Health. 2017.
Straus WL, Plouffe JF, File TM, Lipman HB, Hackman BH, Salstrom S-J, et al. Risk factors for domestic acquisition of Legionnaires disease. Arch Intern Med. 1996;156(Aug):1685.
Alary M, Joly JR. Risk factors for contamination of domestic hot water systems by legionellae. Appl Environ Microbiol. 1991;57:2360–7.
Borella P, Montagna MT, Romano-Spica V, Stampi S, Stancanelli G, Triassi M, et al. Legionella infection risk from domestic hot water. Emerg Infect Dis. 2004;10:457–64.
Rhoads WJ, Ji P, Pruden A, Edwards MA. Water heater temperature set point and water use patterns influence Legionella pneumophila and associated microorganisms at the tap. Microbiome 2015;3:67.
Soda EA, Barskey AE, Shah PP, Schrag S, Whitney CG, Arduino MJ, et al. Vital signs: health care-associated legionnaires’ disease surveillance data from 20 states and a large metropolitan area-United States, 2015. Am J Transpl. 2017;17:2215–20.
Lee TC, Vickers RM, Yu VL, Wagener MM. Growth of 28 Legionella species on selective culture media: a comparative study. J Clin Microbiol. 1993;31:2764–8.
Allegra S, Berger F, Berthelot P, Grattard F, Pozzetto B, Riffard S. Use of flow cytometry to monitor Legionella viability. Appl Environ Microbiol. 2008;74:7813–6.
Allegra S, Grattard F, Girardot F, Riffard S, Pozzetto B, Berthelot P. Longitudinal evaluation of the efficacy of heat treatment procedures against Legionella spp. in hospital water systems by using a flow cytometric assay. Appl Environ Microbiol. 2011;77:1268–75.
Bentham R, Whiley H, Bentham R, Whiley H. Quantitative microbial risk assessment and opportunist waterborne infections–are there too many gaps to fill? Int J Environ Res Public Health. 2018;15:1150.
Van Kenhove E, Dinne K, Janssens A, Laverge J. Overview and comparison of Legionella regulations worldwide. Am J Infect Control. 2019;47:968–78.
Codony F, Dinh-Thanh M, Agustí G. Key factors for removing bias in viability PCR-based methods: a review. Curr Microbiol. 2020;77:682–7.
Shevchuk O, Jäger J, Steinert M. Virulence properties of the legionella pneumophila cell envelope. Front Microbiol. 2011;2:74.
Díaz-Flores Á, Montero JC, Castro FJ, Alejandres EM, Bayón C, Solís I, et al. Comparing methods of determining Legionella spp. in complex water matrices. BMC Microbiol. 2015;15:91.
Quero S, Párraga-Niño N, Garcia-Núñez M, Pedro-Botet ML, Gavaldà L, Mateu L, et al. The impact of pipeline changes and temperature increase in a hospital historically colonised with Legionella. Sci Rep. 2021;11:1916.
Proctor CR, Dai D, Edwards MA, Pruden A. Interactive effects of temperature, organic carbon, and pipe material on microbiota composition and Legionella pneumophila in hot water plumbing systems. Microbiome. 2017;5:130.
Gavaldà L, Garcia-Nuñez M, Quero S, Gutierrez-Milla C, Sabrià M. Role of hot water temperature and water system use on Legionella control in a tertiary hospital: An 8-year longitudinal study. Water Res. 2019;149:460–6.
ISO 11731:2017 - Water quality - Enumeration of Legionella [Internet]. 2017 [cited 2019 Jun 26]. Available from: https://www.iso.org/standard/61782.html
Albalat GR, Broch BB, Bono MJ. Method Modification of the Legipid ® Legionella Fast Detection Test Kit. J AOAC Int. 2014;97:1403–9.
Totaro M, Mariotti T, Bisordi C, De Vita E, Valentini P, Costa AL, et al. Evaluation of legionella pneumophila decrease in hot water network of four hospital buildings after installation of electron time flow taps. Water. 2020;12:210.
Nakamura I, Amemura-Maekawa J, Kura F, Kobayashi T, Sato A, Watanabe H, et al. Persistent Legionella contamination of water faucets in a tertiary hospital in Japan. Int J Infect Dis. 2020;93:300–4.
Stout JE, Yu VL. Environmental culturing for Legionella: Can we build a better mouse trap? Am J Infect Control. 2010;38:341–3.
Stout JE, Muder RR, Mietzner S, Wagener MM, Perri MB, DeRoos K, et al. Role of environmental surveillance in determining the risk of hospital-acquired legionellosis: a national surveillance study with clinical correlations. Infect Control Hosp Epidemiol. 2007;28:818–24.
Allen JG, Myatt TA, MacIntosh DL, Ludwig JF, Minegishi T, Stewart JH, et al. Assessing risk of health care-acquired Legionnaires’ disease from environmental sampling: The limits of using a strict percent positivity approach. Am J Infect Control. 2012;40:917–21.
Hamilton KA, Haas CN Critical review of mathematical approaches for quantitative microbial risk assessment (QMRA) of: Legionella in engineered water systems: Research gaps and a new framework. 2, Environmental Science: Water Research and Technology. Royal Society of Chemistry; 2016. p. 599–613.
Whiley H, Taylor M. Critical reviews in microbiology Legionella detection by culture and qPCR: Comparing apples and oranges. Crit Rev Microbiol. 2016;42:65–74.
Dietersdorfer E, Kirschner A, Schrammel B, Ohradanova-Repic A, Stockinger H, Sommer R, et al. Starved viable but non-culturable (VBNC) Legionella strains can infect and replicate in amoebae and human macrophages. Water Res. 2018;141:428–38.
Shamsizadeh Z, Ehrampoush MH, Nikaeen M, Ebrahimi AA, Asghari FB. Investigation of hospital water systems contamination to bacterial agents of nosocomial infections. Int J Environ Health Eng. 2020;9:10.
Lai C-C, Wang C-Y, Hsueh P-R. Co-infections among patients with COVID-19: The need for combination therapy with non-anti-SARS-CoV-2 agents? J Microbiol Immunol Infect. 2020;53:505–12.
Cebrián F, Montero JC, Fernández PJ. New approach to environmental investigation of an explosive legionnaireś disease outbreak in Spain: Early identification of potential risk sources by rapid Legionella spp immunosensing technique. BMC Infect Dis. 2018;18:696.
Acknowledgements
The authors would like to thank the staff of the following laboratories for their help in offering us the resources in running the water assays: Ambientalys (Laboratory 1), Iproma (Laboratory 2) and Anticimex. No sources of funding required.
Author information
Authors and Affiliations
Contributions
RO is the principal investigator of the Public Health and Patient Safety Research Group at the Catholic University of Valencia. He directed the meetings and the preparation of this document. EL is the Co-I of this working group. Both authors contributed to the writing of the text. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare that they have no conflict of interest.
Ethics approval and consent to participate
This manuscript was approved by the Hospital Clínico Universitario de Valencia (Spain).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ortí-Lucas, R.M., Luciano, E. New immunomagnetic separation method to analyze risk factors for Legionella colonization in health care centres. J Expo Sci Environ Epidemiol 32, 744–750 (2022). https://doi.org/10.1038/s41370-022-00421-0
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41370-022-00421-0