Abstract
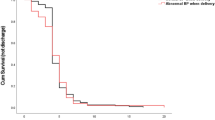
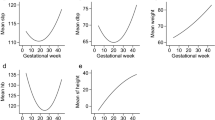
To date, data on postpartum management of preeclampsia including the optimal time for discharge are limited. The aims of this study were to investigate the appropriate time for discharge after delivery, and factors that could affect the time for discharge. Data on 210 preeclamptic women including the severity or time of onset and days in the ward after delivery were collected and analysed. In total, 167 (73%) patients were followed up for at least 16 months and none of them developed any complications after delivery. The mean days in the ward after delivery in preeclamptic women with vaginal delivery or with caesarean section was 3.4 or 5.8 days, respectively. After adjusting for delivery modes and parity, women with severe or early onset preeclampsia or preeclamptic women complicated with IUGR were in the ward longer than women with mild or late onset of preeclampsia or preeclamptic women without IUGR. In addition, women with severe preeclampsia or with IUGR delayed the time for blood pressure to return to normal range. Our descriptive data reported that preeclamptic women stayed in the ward for 4–6 days after delivery, dependent on the delivery modes. Preeclamptic women with severe or early onset form or complicated with IUGR delayed the improvement of clinical symptoms after delivery. We further found that women with severe preeclampsia, and preeclampsia complicated with IUGR delayed blood pressure returning to normal range. These pre-discharge checklists may help obstetricians and midwives decide when to discharge.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Ananth CV, Keyes KM, Wapner RJ Pre-eclampsia rates in the United States, 1980–2010: age-period-cohort analysis. BMJ. 2013; 347. https://doi.org/10.1136/bmj.f6564.
Hogan MC, Foreman KJ, Naghavi M, Ahn SY, Wang M, Makela SM, et al. Maternal mortality for 181 countries, 1980-2008: a systematic analysis of progress towards Millennium Development Goal 5. Lancet. 2010;375:1609–23.
Hernández-Díaz S, Toh S, Cnattingius S. Risk of pre-eclampsia in first and subsequent pregnancies: prospective cohort study. BMJ. 2009;339:34.
Staff AC. Long-term cardiovascular health after stopping pre-eclampsia. Lancet. 2019;394:1120–1.
Vikse BE, Hallan S, Bostad L, Leivestad T, Iversen BM. Previous preeclampsia and risk for progression of biopsy-verified kidney disease to end-stage renal disease. Nephrol Dial Transpl. 2010;25:3289–96.
Grand’Maison S, Pilote L, Schlosser K, Stewart DJ, Okano M, Dayan N. Clinical features and outcomes of acute coronary syndrome in women with previous pregnancy complications. Can J Cardiol. 2017;33:1683–92.
Varnier N, Brown MA, Reynolds M, Pettit F, Davis G, Mangos G, et al. Indications for delivery in pre-eclampsia. Pregnancy Hypertens. 2018;11:12–17.
Sibai BM, Stella CL. Diagnosis and management of atypical preeclampsia-eclampsia. Am J Obstet Gynecol. 2009;200:481.e1–481.e7.
Leeman L, Dresang LT, Fontaine P. Hypertensive disorders of pregnancy. Am Fam Physician. 2016;93:121–7.
Magee L, von Dadelszen P. Prevention and treatment of postpartum hypertension. Cochrane Database Syst Rev. 2013; https://doi.org/10.1002/14651858.
Smith M, Waugh J, Nelson-Piercy C. Management of postpartum hypertension. Obstet Gynaecol. 2013;15:45–50.
Sibai B, Dekker, Kupferminc M. Pre-eclampsia, The Lancet 2005;365:785–99.
Benahmed N, San Miguel L, Devos C, Fairon N, Christiaens W. Vaginal delivery: how does early hospital discharge affect mother and child outcomes? A systematic literature review. BMC Pregnancy Childbirth. 2017;17:1–14.
Brown MA, Magee LA, Kenny LC, Karumanchi SA, McCarthy FP, Saito S, et al. Hypertensive disorders of pregnancy: ISSHP classification, diagnosis, and management recommendations for international practice. Hypertension. 2018;72:24–43.
Dai L, Deng C, Li Y, Zhu J, Mu Y, Deng Y et al. Birth weight reference percentiles for Chinese. PLoS One. 2014; 9. https://doi.org/10.1371/journal.pone.0104779.
Matthys LA, Coppage KH, Lambers DS, Barton JR, Sibai BM. Delayed postpartum preeclampsia: an experience of 151 cases. Am J Obstet Gynecol. 2004;190:1464–6.
Atterbury JL, Groome LJ, Hoff C. Blood pressure changes in normotensive women readmitted in the postpartum period with severe preeclampsia/eclampsia. J Matern Neonatal Med. 1996;5:201–5.
Mongraw-Chaffin ML, Cirillo PM, Cohn BA. Preeclampsia and cardiovascular disease death: prospective evidence from the child health and development studies cohort. Hypertension. 2010;56:166–71.
Acknowledgements
We would like to thank Greg Gamble, from The University of Auckland for helping statistical analysis.
Funding
This study was received the support from Shaanxi Province International collaborative program (Grant number 2016KW-006), Shaanxi province Science and Technology Development project (Grant number 2020SF-040).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, C., Gou, W., Liu, J. et al. Length of stay in the ward following a preeclamptic pregnancy. J Hum Hypertens 36, 201–206 (2022). https://doi.org/10.1038/s41371-021-00484-w
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41371-021-00484-w
This article is cited by
-
Factors related to postpartum length of stay in women with pre-eclampsia: a systematic review
BMC Pregnancy and Childbirth (2025)
-
Analysis of postpartum hypertension in women with preeclampsia
Journal of Human Hypertension (2023)