Abstract
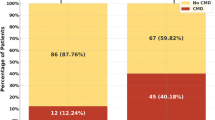
Coronary collateral flow (CCF) is crucial for myocardial viability in patients with obstructive coronary artery disease, specifically ST-elevation myocardial infarction (STEMI). However, hypertension can contribute to vascular dysfunction and hinder the formation of CCF. Wide pulse pressure (WPP), defined as ≥65 mmHg, may better reflect impaired cardiovascular health compared to classic blood pressure indices. The effect of WPP on CCF remains unclear. Therefore, we aimed to evaluate the impact of WPP on CCF. This retrospective study included 1180 STEMI patients that underwent primary percutaneous coronary intervention (PCI) between 2021 and 2023 at a tertiary healthcare center. Patients were classified into good and poor CCF groups based on the Rentrop classification. Out of these patients, 272 (23.1%) had good CCF, while 908 (76.9%) had poor CCF. Two distinct models were constructed using multivariable logistic regression analysis to identify independent predictors of good CCF, including pulse pressure (Model 1) and WPP (Model 2). Covariates such as age, gender, diabetes mellitus, smoking, pre-infarction angina, Killip Class 3/4, multivessel disease, peak troponin, pre-thrombolysis in myocardial infarction (TIMI) flow 0, and previous PCI were added to both models. WPP was identified as an independent predictor that negatively influences good CCF (OR: 0.511, 95% CI: 0.334–0.783, p = 0.002). Moreover, diabetes, pre-infarction angina, Killip class III/IV, multivessel disease, and pre-TIMI flow 0 were also found to be independent predictors of CCF. WPP, derived from blood pressure measurements, has been associated with poor CCF in STEMI patients undergoing primary PCI and may serve as a predictor of poor CCF.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The data of the research is available in our University Hospital archive. A de-identified dataset will be shared with other researchers upon reasonable request from the corresponding author.
References
Yoon SJ, Ko YG, Kim JS, Moon JY, Kim YJ, Park S, et al. Impact of coronary artery collaterals on infarct size assessed by serial cardiac magnetic resonance imaging after primary percutaneous coronary intervention in patients with acute myocardial infarction. Coron Artery Dis. 2009;20:440–5. https://doi.org/10.1097/MCA.0B013E328330C930.
Alsanjari O, Chouari T, Williams T, Myat A, Sambu N, Blows L. et al. Angiographically visible coronary artery collateral circulation improves prognosis in patients presenting with acute ST segment-elevation myocardial infarction. Catheter Cardiovasc Interv. 2020;96:528–33. https://doi.org/10.1002/CCD.28532.
Cui K, Lyu S, Song X, Yuan F, Xu F, Zhang M, et al. Effect of coronary collaterals on prognosis in patients undergoing primary percutaneous coronary intervention for acute ST-segment elevation myocardial infarction: a meta-analysis. Angiology. 2018;69:803–11. https://doi.org/10.1177/0003319718768399.
Tang KS, Medeiros ED, Shah AD. Wide pulse pressure: a clinical review. J Clin Hypertens. 2020;22:1960–7. https://doi.org/10.1111/JCH.14051.
Yang D, Chen J, Zhang T, Lin Y, Yao X, Meng L, et al. Influencing factors of wide pulse pressure in an elderly Chinese population: a cross-sectional study. J Clin Hypertens. 2022;24:1482–90. https://doi.org/10.1111/JCH.14582.
Wang P, Li Y, Liu X, Wang Q, Guo Y, Zhao Y, et al. Independent and cumulative effects of resting heart rate and pulse pressure with type 2 diabetes mellitus in Chinese rural population. Sci Rep. 2017;7. https://doi.org/10.1038/S41598-017-02758-1.
Okada K, Iso H, Cui R, Inoue M, Tsugane S. Pulse pressure is an independent risk factor for stroke among middle-aged Japanese with normal systolic blood pressure: the JPHC study. J Hypertens. 2011;29:319–24. https://doi.org/10.1097/HJH.0B013E32834143D9.
Geng TT, Talaei M, Jafar TH, Yuan JM, Koh WP. pulse pressure and the risk of end-stage renal disease among Chinese adults in Singapore: the Singapore Chinese health study. J Am Heart Assoc. 2019;8. https://doi.org/10.1161/JAHA.119.013282.
Franklin SS, Khan SA, Wong ND, Larson MG, Levy D. Is pulse pressure useful in predicting risk for coronary heart Disease? The Framingham heart study. Circulation. 1999;100:354–60. https://doi.org/10.1161/01.CIR.100.4.354.
Mancusi C, Losi MA, Izzo R, Canciello G, Carlino MV, Albano G, et al. Higher pulse pressure and risk for cardiovascular events in patients with essential hypertension: the Campania salute network. Eur J Prev Cardiol. 2018;25:235–43. https://doi.org/10.1177/2047487317747498.
Lorenzo C, Aung K, Stern MP, Haffner SM. Pulse pressure, prehypertension, and mortality: the San Antonio heart study. Am J Hypertens. 2009;22:1219–26. https://doi.org/10.1038/AJH.2009.151.
Peter Rentrop K, Cohen M, Blanke H, Phillips RA. Changes in collateral channel filling immediately after controlled coronary artery occlusion by an angioplasty balloon in human subjects. J Am Coll Cardiol. 1985;5:587–92. https://doi.org/10.1016/S0735-1097(85)80380-6.
Williams B, Mancia G, Spiering W, Rosei EA, Azizi M, Burnier M, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–104. https://doi.org/10.1093/EURHEARTJ/EHY339.
Homan TD, Bordes SJ, Cichowski E. Physiology, Pulse Pressure. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. 2024 Jan [updated 2023 Jul 10]. https://www.ncbi.nlm.nih.gov/books/NBK482408/.
DeMers D, Wachs D. Physiology, Mean Arterial Pressure. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. 2024 Jan [Updated 2023 Apr 10]. https://www.ncbi.nlm.nih.gov/books/NBK538226/
Mancia Chairperson G, Kreutz Co-Chair R, Brunström M, Burnier M, Grassi G, Januszewicz A, et al. 2023 ESH guidelines for the management of arterial hypertension the task force for the management of arterial hypertension of the European Society of Hypertension endorsed by the European Renal Association (ERA) and the International Society of Hypertension (ISH). J Hypertens. 2023. https://doi.org/10.1097/HJH.0000000000003480.
Benetos A, Rudnichi A, Safar M, Guize L. Pulse pressure and cardiovascular mortality in normotensive and hypertensive subjects. Hypertension. 1998;32:560–4. https://doi.org/10.1161/01.HYP.32.3.560.
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2014;37:S81–S90. https://doi.org/10.2337/DC14-S081.
François Mach, Colin Baigent, Alberico L Catapano, Konstantinos C Koskinas, Manuela Casula, Lina Badimon, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk: The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS). Eur Heart J. 2020;41:111–188. https://doi.org/10.1093/eurheartj/ehr158.
Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39:119–77. https://doi.org/10.1093/EURHEARTJ/EHX393.
Sotomi Y, Ueda Y, Hikoso S, Okada K, Dohi T, Kida H, et al. Pre-infarction angina: time interval to onset of myocardial infarction and comorbidity predictors. Front Cardiovasc Med. 2022;9. https://doi.org/10.3389/FCVM.2022.867723/FULL.
Carmeliet P. Mechanisms of angiogenesis and arteriogenesis. Nat Med. 2000;6:389–95. https://doi.org/10.1038/74651.
Schaper W, Ito WD. Molecular mechanisms of coronary collateral vessel growth. Circ Res. 1996;79:911–9. https://doi.org/10.1161/01.RES.79.5.911.
Bigler MR, Seiler C. The human coronary collateral circulation, its extracardiac anastomoses and their therapeutic promotion. Int J Mol Sci. 2019;20. https://doi.org/10.3390/ijms20153726.
Vural A, Kurt D, Karagöz A, Emecen Ö, Aydin E. The relationship between coronary collateral circulation and serum adropin levels. Cureus. 2023;15. https://doi.org/10.7759/CUREUS.35166.
Koerselman J, de Jaegere PPT, Verhaar MC, van der Graaf Y, Grobee DE, Algra A, et al. High blood pressure is inversely related with the presence and extent of coronary collaterals. J Hum Hypertens. 2005;19:809–17. https://doi.org/10.1038/SJ.JHH.1001917.
Bakris GL, Laffin LJ. Assessing wide pulse pressure hypertension: data beyond the guidelines. J Am Coll Cardiol. 2019;73:2856–8. https://doi.org/10.1016/J.JACC.2019.03.494.
Vicaut E. Microcirculation and arterial hypertension. Drugs. 1999;58:1–10. https://doi.org/10.2165/00003495-199958991-00001.
Boudier HA. Arteriolar and capillary remodelling in hypertension. Drugs. 1999;58:37–40.
Boudier HA. Hypertension et microcirculation [Hypertension and microcirculation]. Arch Mal Coeur Vaiss. 2002;95:17–22.
Nicolau JC, Pinto MAFV, Nogueira PR, Lorga AM, Jacob JLB, Garzon SAC. The role of antegrade and collateral flow in relation to left ventricular function post-thrombolysis. Int J Cardiol. 1997;61:47–54. https://doi.org/10.1016/S0167-5273(97)00134-4.
Kim EK, Choi JH, Song YBin, Hahn JY, Chang SA, Park SJ, et al. A protective role of early collateral blood flow in patients with ST-segment elevation myocardial infarction. Am Heart J. 2016;171:56–63. https://doi.org/10.1016/J.AHJ.2015.10.016.
Author information
Authors and Affiliations
Contributions
Conceptualization and design: CY, BGŞ, AK. Data collection: AK, CY, BK, MMT. Data curation and analysis: BK, MMT, CY. Writing original draft: CY. Writing reviewing and editing; TU, RZ, CY, MMT, AK, BGŞ.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study adhered to the principles of the Declaration of Helsinki and received ethical approval from the Kartal Kosuyolu Training and Research Hospital (Approval no: 2024/09/816).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yılmaz, C., Güvendi Şengör, B., Karaduman, A. et al. Association of wide pulse pressure with coronary collateral flow in patients with ST-elevation myocardial infarction undergoing percutaneous coronary intervention. J Hum Hypertens 39, 210–216 (2025). https://doi.org/10.1038/s41371-024-00986-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41371-024-00986-3