Abstract
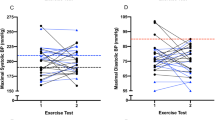
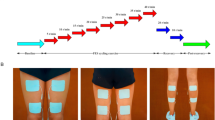
Exaggerated systolic blood pressure (SBP) during submaximal exercise is associated with increased cardiovascular (CV) risk. However, findings are mixed and new evidence indicates that cardiorespiratory fitness should be considered for proper clinical interpretation of exercise SBP responses. This study aimed to determine the relationship between exercise SBP during submaximal effort corrected and uncorrected for fitness, as well as at peak effort and abnormalities of cardiac structure and function. Each of 231 participants with controlled BP (with or without previously diagnosed hypertension), no evidence for ischemic or valvular heart disease, or heart failure underwent cardiopulmonary exercise testing and resting and exercise echocardiography. Submaximal exercise SBP (measured at the 2nd stage of Bruce protocol) and peak exercise SBP was corrected for peak VO2. Associations with TOD – target organ damage (left ventricular [LV] mass, relative wall thickness, diastolic function, LV exercise reserve) were stronger for fitness-corrected than uncorrected exercise SBP. There was a progressive deterioration of cardiac function and structure parameters across the submaximal exercise SBP/peak VO2 tertiles. Multivariable models demonstrated that fitness-corrected SBP was more closely associated with LV hypertrophy and diastolic dysfunction than uncorrected SBP, and ROC analysis revealed better performance of fitness-corrected SBP than uncorrected SBP (AUC 0.792 vs. 0.627, and 0.808 vs. 0.662, both p < 0.001, for LV hypertrophy and diastolic dysfunction, respectively). Fitness-corrected SBP responses to submaximal exercise can identify more profound target organ damage with respect to cardiac function and structure even among patients with controlled clinic BP. Exaggerated BP response to exercise must be considered relative to fitness for proper clinical interpretation of BP responses to exercise testing.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
Data are available from the corresponding author on reasonable request.
References
Bakris G, Hill M, Mancia G, Steyn K, Black HR, Pickering T, et al. Achieving blood pressure goals globally: five core actions for health-care professionals. a worldwide call to action. J Hum Hypertens. 2008;22:63–70.
Messerli FH, Williams B, Ritz E. Essential hypertension. Lancet. 2007;370:591–603.
Lawes CM, Vander Hoorn S, Law MR, Elliott P, MacMahon S, Rodgers A. Blood pressure and the global burden of disease 2000. Part II: estimates of attributable burden. J Hypertens. 2006;24:423–30.
Kokkinos P, Pittaras A, Narayan P, Faselis C, Singh S, Manolis A. Exercise capacity and blood pressure associations with left ventricular mass in prehypertensive individuals. Hypertension. 2007;49:55–61.
Mottram PM, Haluska B, Yuda S, Leano R, Marwick TH. Patients with a hypertensive response to exercise have impaired systolic function without diastolic dysfunction or left ventricular hypertrophy. J Am Coll Cardiol. 2004;43:848–53.
Takamura T, Onishi K, Sugimoto T, Kurita T, Fujimoto N, Dohi K, et al. Patients with a hypertensive response to exercise have impaired left ventricular diastolic function. Hypertens Res. 2008;31:257–63.
Yang WI, Kim JS, Kim SH, Moon JY, Sung JH, Kim IJ, et al. J Hypertens. 2014;32:1862–9.
Schultz MG, Currie KD, Hedman K, Climie RE, Maiorana A, Coombes JS, et al. The identification and management of high blood pressure using exercise blood pressure: current evidence and practical guidance. Int J Env Res Public Health. 2022;19:2819.
Schultz MG, Picone DS, Nikolic SB, Williams AD, Sharman JE. Exaggerated blood pressure response to early stages of exercise stress testing and presence of hypertension. J Sci Med Sport. 2016;19:1039–42.
Schultz MG, La Gerche A, Sharman JE. Cardiorespiratory fitness, workload, and the blood pressure response to exercise testing. Exerc Sport Sci Rev. 2022;50:25–30.
Huang Z, Park C, Chaturvedi N, Howe LD, Sharman JE, Hughes AD, et al. Cardiorespiratory fitness, fatness, and the acute blood pressure response to exercise in adolescence. Scand J Med Sci Sports. 2021;31:1693–8.
Huang Z, Fonseca R, Sharman JE, Park C, Chaturvedi N, Howe LD, et al. The influence of fitness on exercise blood pressure and its association with cardiac structure in adolescence. Scand J Med Sci Sports. 2020;30:1033–9.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European society of cardiology (ESC) and the european society of hypertension (ESH). Eur Heart J. 2018;39:3021–104.
Nikolic SB, Abhayaratna WP, Leano R, Stowasser M, Sharman JE. Waiting a few extra minutes before measuring blood pressure has potentially important clinical and research ramifications. J Hum Hypertens. 2014;28:56–61.
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American society of echocardiography and the European association of cardiovascular imaging. Eur Heart J Cardiovasc Imaging. 2015;16:233–71.
Nagueh SF, Smiseth OA, Appleton CP, Byrd BF, Dokainish H, Edvardsen T, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American society of echocardiography and the European association of cardiovascular imaging. Eur Heart J Cardiovasc Imaging. 2016;17:1321–60.
Smiseth OA, Morris DA, Cardim N, Cikes M, Delgado V, Donal E, et al. Multimodality imaging in patients with heart failure and preserved ejection fraction: an expert consensus document of the european association of cardiovascular imaging. Eur Heart J Cardiovasc Imaging. 2022;23:e34–61.
Myers J, Arena R, Franklin B, Pina I, Kraus WE, McInnis K, et al. Recommendations for clinical exercise laboratories: a scientific statement from the American Heart Association. Circulation. 2009;119:3144–61.
Stergiou GS, Giovas PP, Gkinos CP, Tzamouranis DG. Validation of the A&D UM-101 professional hybrid device for office blood pressure measurement according to the international protocol. Blood Press Monit. 2008;13:37–42.
Schultz MG, Sharman JE. Exercise hypertension. Pulse. 2014;1:161–76.
Wei W, Tölle M, Zidek W, van der Giet M. Validation of the mobil-O-Graph: 24 h-blood pressure measurement device. Blood Press Monit. 2010;15:225–8.
McEvoy JW, McCarthy CP, Bruno RM, Brouwers S, Canavan MD, Ceconi C, et al. 2024 ESC guidelines for the management of elevated blood pressure and hypertension: developed by the task force on the management of elevated blood pressure and hypertension of the European society of cardiology (ESC) and endorsed by the European society of endocrinology (ESE) and the European stroke organisation (ESO). Eur Heart J. 2024;45:3912–4018.
Bauer P, Kraushaar L, Dörr O, Nef H, Hamm CW, Most A. Workload-indexed blood pressure response to a maximum exercise test among professional indoor athletes. Eur J Prev Cardiol. 2021;28:1487–94.
Joyner MJ, Casey DP. Regulation of increased blood flow (hyperemia) to muscles during exercise: a hierarchy of competing physiological needs. Physiol Rev. 2015;95:549–601.
Schultz MG, Otahal P, Cleland VJ, Blizzard L, Marwick TH, Sharman JE. Exercise-induced hypertension, cardiovascular events, and mortality in patients undergoing exercise stress testing: a systematic review and meta-analysis. Am J Hypertens. 2013;26:357–66.
Zafrir B, Aker A, Asaf Y, Saliba W. Blood pressure response during treadmill exercise testing and the risk for future cardiovascular events and new-onset hypertension. J Hypertens. 2022;40:143–52.
Sarma S, Howden E, Carrick-Ranson G, Lawley J, Hearon C, Samels M, et al. Elevated exercise blood pressure in middle-aged women is associated with altered left ventricular and vascular stiffness. J Appl Physiol. 2020;128:1123–9.
Miyai N, Shiozaki M, Terada K, Takeshita T, Utsumi M, Miyashita K, et al. Exaggerated blood pressure response to exercise is associated with subclinical vascular impairment in healthy normotensive individuals. Clin Exp Hypertens. 2021;43:56–62.
Schultz MG, La Gerche A, Sharman JE. Blood pressure response to exercise and cardiovascular disease. Curr Hypertens Rep. 2017;19:89.
Stewart KJ, Sung J, Silber HA, Fleg JL, Kelemen MD, Turner KL, et al. Exaggerated exercise blood pressure is related to impaired endothelial vasodilator function. Am J Hypertens. 2004;17:314–20.
Tzemos N, Lim PO, Mackenzie IS, MacDonald TM. Exaggerated exercise blood pressure response and future cardiovascular disease. J Clin Hypertens. 2015;17:837–44.
Thanassoulis G, Lyass A, Benjamin EJ, Larson MG, Vita JA, Levy D, et al. Relations of exercise blood pressure response to cardiovascular risk factors and vascular function in the framingham heart study. Circulation. 2012;125:2836–43.
Funding
This work was funded by the grant from the National Science Centre Poland (UMO-201829/B/NZ5/01172.
Author information
Authors and Affiliations
Contributions
WK, JS, MPK contributed to study conception and design, ethical approval, data collection, and analysis as well as manuscript writing. WK, JZ, AKW, WK, TK, and GK recruited participants, performed study procedures and provided feedback on manuscript writing. JZ, JS, AKW, TK, WK, MPK, GK and WK critically revised the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
All methods were performed in accordance with the relevant guidelines and regulations. The study was conducted in accordance with the Declaration of Helsinki and approved by the ethics committee of Wroclaw Medical University. Informed consent was obtained from all participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41371_2025_1079_MOESM1_ESM.pdf
Exaggerated blood pressure response to submaximal exercise and cardiac target organ damage: importance of fitness. Supplementary materials
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zachwyc, J., Sharman, J.E., Kosowski, W. et al. Exaggerated blood pressure response to submaximal exercise and cardiac target organ damage: importance of fitness. J Hum Hypertens 39, 849–858 (2025). https://doi.org/10.1038/s41371-025-01079-5
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41371-025-01079-5