Abstract
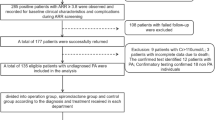
Apparent treatment-resistant hypertension (aTRH) is linked to significantly elevated cardiovascular risk and unfavorable long-term outcomes. Despite guideline recommendations to screen for primary aldosteronism (PA) in patients with aTRH, the prevalence of screening in Asian ambulatory care settings remains unknown. This cross-sectional study evaluated hypertensive adults who were managed in the ambulatory clinics of a tertiary hospital in Thailand between January 2020 and May 2023. aTRH was defined by: (1)uncontrolled office blood pressure (BP ≥ 140/90 mmHg) despite maximally tolerated doses of three antihypertensive drug classes, including a diuretic, or (2)use of four or more antihypertensive classes regardless of BP control. PA screening was performed using plasma aldosterone concentration and plasma renin activity measurements. Among 3207 hypertensive patients identified via ICD-10 (I10) coding, 2047 met inclusion criteria after excluding 1160 based on the exclusion criteria; the prevalence of aTRH was 9.4%. The mean age of the aTRH group was 74 ± 10 years, 59% were female, and the average number of antihypertensive agents was 3.8 ± 0.7. PA screening was conducted in only 3.1% of patients with aTRH and 17.9% of hypokalemia, with a median delay of 9.5 (21.25) months from the detection of hypokalemia to PA testing. Among 20 screened patients, five were diagnosed with PA, leading to improved BP control with targeted therapy. This study represents the first real-world analysis of PA screening practices in an Asian ambulatory care population. Strategies to enhance PA screening and address barriers to its implementation are warranted to improve clinical outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets used and/or analyzed during this study are available from the corresponding author upon reasonable request.
References
Carey RM, Calhoun DA, Bakris GL, Brook RD, Daugherty SL, Dennison-Himmelfarb CR, et al. Resistant hypertension: detection, evaluation, and management: a scientific statement from the American heart association. Hypertension. 2018;72:e53–e90.
Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 International Society of Hypertension global hypertension practice guidelines. Hypertension. 2020;75:1334–57.
Kunanon S, Chattranukulchai P, Chotruangnapa C, Kositanurit W, Methavigul K, Boonyasirinant T, et al. 2019 Thai guidelines on the treatment of hypertension: executive summary. J Med Assoc Thai. 2021;104:1729–38.
Mancia G, Kreutz R, Brunström M, Burnier M, Grassi G, Januszewicz A, et al. 2023 ESH Guidelines for the management of arterial hypertension the task force for the management of arterial hypertension of the European society of hypertension: endorsed by the international society of hypertension (ISH) and the European renal association (ERA). J Hypertens. 2023;41:1874–2071.
Achelrod D, Wenzel U, Frey S. Systematic review and meta-analysis of the prevalence of resistant hypertension in treated hypertensive populations. Am J Hypertens. 2015;28:355–61.
Chia R, Pandey A, Vongpatanasin W. Resistant hypertension-defining the scope of the problem. Prog Cardiovasc Dis. 2020;63:46–50.
Montrivade S, Chattranukulchai P, Siwamogsatham S, Vorasettakarnkij Y, Naeowong W, Boonchayaanant P, et al. Hypertension subtypes among Thai hypertensives: an analysis of telehealth-assisted instrument in home blood pressure monitoring nationwide pilot project. Int J Hypertens. 2020;2020:3261408.
Brown JM, Siddiqui M, Calhoun DA, Carey RM, Hopkins PN, Williams GH, et al. The unrecognized prevalence of primary aldosteronism: a cross-sectional study. Ann Intern Med. 2020;173:10–20.
Turcu AF, Yang J, Vaidya A. Primary aldosteronism - a multidimensional syndrome. Nat Rev Endocrinol. 2022;18:665–82.
Vaidya A, Carey RM. Evolution of the primary aldosteronism syndrome: updating the approach. J Clin Endocrinol Metab. 2020;105:3771–83.
Burrello J, Monticone S, Losano I, Cavaglia G, Buffolo F, Tetti M, et al. Prevalence of hypokalemia and primary aldosteronism in 5100 patients referred to a tertiary hypertension unit. Hypertension. 2020;75:1025–33.
Loh KC, Koay ES, Khaw MC, Emmanuel SC, Young WF Jr. Prevalence of primary aldosteronism among Asian hypertensive patients in Singapore. J Clin Endocrinol Metab. 2000;85:2854–9.
Xu Z, Yang J, Hu J, Song Y, He W, Luo T, et al. Primary aldosteronism in patients in china with recently detected hypertension. J Am Coll Cardiol. 2020;75:1913–22.
Jones DW, Ferdinand KC, Taler SJ, Johnson HM, Shimbo D, Abdalla M, et al. 2025 AHA/ACC/AANP/AAPA/ABC/ACCP/ACPM/AGS/AMA/ASPC/NMA/PCNA/SGIM Guideline for the prevention, detection, evaluation and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Hypertension. 2025;82:e212–e316.
Adler GK, Stowasser M, Correa RR, Khan N, Kline G, McGowan MJ, et al. Primary aldosteronism: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2025;110:2453–95.
Cohen JB, Cohen DL, Herman DS, Leppert JT, Byrd JB, Bhalla V. Testing for primary aldosteronism and mineralocorticoid receptor antagonist use among U.S. Veterans : a retrospective cohort study. Ann Intern Med. 2021;174:289–97.
Hundemer GL, Imsirovic H, Vaidya A, Yozamp N, Goupil R, Madore F, et al. Screening rates for primary aldosteronism among individuals with hypertension plus hypokalemia: a population-based retrospective cohort study. Hypertension. 2022;79:178–86.
Chattranukulchai P, Roubsanthisuk W, Kunanon S, Kotruchin P, Satirapoj B, Wongpraparut N, et al. Resistant hypertension: diagnosis, evaluation, and treatment a clinical consensus statement from the Thai hypertension society. Hypertens Res. 2024;47:2447–55.
Chia YC, Ching SM. Prevalence and predictors of resistant hypertension in a primary care setting: a cross-sectional study. BMC Fam Pract. 2014;15:131.
Naseem R, Adam AM, Khan F, Dossal A, Khan I, Khan A, et al. Prevalence and characteristics of resistant hypertensive patients in an Asian population. Indian Heart J. 2017;69:442–6.
Sakulsupsiri A, Chattranukulchai P, Siwamogsatham S, Boonchayaanant P, Naeowong W, Ariyachaipanich A, et al. Home blood pressure control and drug prescription patterns among Thai hypertensives: a 1-year analysis of telehealth assisted instrument in home blood pressure monitoring nationwide pilot project. Int J Hypertens. 2021;2021:8844727.
Zekarias K, Tessier KM. Screening rate for primary aldosteronism among patients with apparent treatment-resistant hypertension: retrospective analysis of current practice. Endocr Pract. 2022;28:271–5.
Jaffe G, Gray Z, Krishnan G, Stedman M, Zheng Y, Han J, et al. Screening rates for primary aldosteronism in resistant hypertension: a cohort study. Hypertension. 2020;75:650–9.
Turcu AF, Nhan W, Grigoryan S, Zhang L, Urban C, Liu H, et al. Primary aldosteronism screening rates differ with sex, race, and comorbidities. J Am Heart Assoc. 2022;11:e025952.
Funes Hernandez M, Bhalla V. Underdiagnosis of primary aldosteronism: a review of screening and detection. Am J Kidney Dis. 2023;82:333–46.
Kositanurit W, Giacona JM, Xie D, Wang J, Feuer D, O’Malley KJ, et al. Trends in primary aldosteronism screening among high-risk hypertensive adults. J Am Heart Assoc. 2024;13:e036373.
Tsan K, Yang J, Nainani A, Libianto R, Russell G. Screening for primary aldosteronism in primary care: a scoping review. Fam Pract. 2024;41:851–6.
Suntornlohanakul O, Sakarin S, Kietsiriroje N, Sriplung H. Geographical inequality in service utilization for primary aldosteronism screening: spatial epidemiological study in Southern Thailand. BMC Health Serv Res. 2022;22:458.
Buffolo F, Burrello J, Burrello A, Heinrich D, Adolf C, Müller LM, et al. Clinical score and machine learning-based model to predict diagnosis of primary aldosteronism in arterial hypertension. Hypertension. 2021;78:1595–604.
Charoensri S, Bashaw L, Dehmlow C, Ellies T, Wyckoff J, Turcu AF. Evaluation of a best-practice advisory for primary aldosteronism screening. JAMA Intern Med. 2024;184:174–82.
Gupta G, Teo AED, Swee DS, Loh LM, Chuah M, Loh WJ, et al. Prolonged hypokalemia and delayed diagnosis of primary aldosteronism: clinical course and risk factors. J Clin Endocrinol Metab. 2024;109:e1574–e81.
Acknowledgements
The authors acknowledge the support for article processing from the Cardiac Center, King Chulalongkorn Memorial Hospital and the use of ChatGPT for checking and editing the grammar of the sentences in this manuscript.
Author information
Authors and Affiliations
Contributions
TS, AY and WK wrote the manuscript. WK and PC created the figures. TS, YV, SS, AS, and PC were involved in the study design. TS and AY participated in data collection. TS, AY and YV performed the data analysis. YV is an essentially intellectual contributor, involved in the research design, data analysis, conclusions and recommendations. All authors have reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Suksiriworaboot, T., Yacharad, A., Kositanurit, W. et al. Prevalence of apparent treatment-resistant hypertension and screening rates for primary aldosteronism in an asian ambulatory care setting. J Hum Hypertens (2025). https://doi.org/10.1038/s41371-025-01105-6
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41371-025-01105-6