Abstract
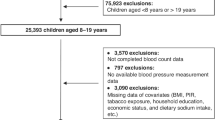
This study investigated the relationship between white blood cell counts and pediatric hypertension, addressing the limited evidence on white blood cell counts/subtypes and pediatric hypertension. A prospective cohort study was conducted involving 5971 children aged 6–12 years in Chongqing, China, with baseline data collected in 2014–2015 and 1282 children completed a 5-year follow-up in 2019. White blood cell indicators, including total white blood cell counts (WBC), lymphocyte counts and percentage (LC, LP), monocyte counts and percentage (MC, MP), neutrophil counts and percentage (ANC, NR), and lymphocyte-monocyte ratio (LMR) were measured using Complete Blood Count (CBC) tests. Blood pressure (BP), and anthropometric indices were also measured. Multilevel linear mixed models and logistic regression models, adjusted for confounders were applied to illustrate the relevance of cell counts indicators and blood pressure. Results showed that compared to normal BP (NBP) group, the elevated BP (EBP) group had significant lower MC(OR(95%CIs) = 0.79(0.68,0.90)) and MP(OR(95%CIs) = 0.78(0.68,0.88)) but higher LMR(OR(95%CIs) = 1.31(1.15,1.50)). Multivariate analyses adjusted for confounding factors revealed that MP was negatively correlated with SBP, DBP and MAP, while LMR positively correlated with these blood pressure(P < 0.05). MC and MP were associated with a reduced risk of hypertension, whereas LMR was associated with an increased risk, particularly in boys. No significant mediation effect of WBC indices between BMI and BP was observed. In conclusion, Peripheral MC, MP, and LMR were significantly associated with pediatric hypertension; MC and MP act as protective factors and LMR acts as a risk factor, suggesting that these indices may serve as potential biomarkers for childhood hypertension.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Datasets are available from the corresponding author (xiaohualiang@hospital.cqmu.edu.cn) upon reasonable request with appropriate ethical approvals and data use agreements that ensure participant privacy protection.
References
Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1345-422.
Hansen ML, Gunn PW, Kaelber DC. Underdiagnosis of hypertension in children and adolescents. Jama. 2007;298:874–9.
Song P, Zhang Y, Yu J, Zha M, Zhu Y, Rahimi K, et al. Global prevalence of hypertension in children: a systematic review and meta-analysis. JAMA pediatrics. 2019;173:1154–63.
Robinson CH, Chanchlani R. High blood pressure in children and adolescents: current perspectives and strategies to improve future kidney and cardiovascular health. Kidney Int Rep. 2022;7:954–70.
Siedlinski M, Jozefczuk E, Xu X, Teumer A, Evangelou E, Schnabel RB, et al. White blood cells and blood pressure: a mendelian randomization study. Circulation. 2020;141:1307–17.
Friedman GD, Selby JV, Quesenberry CP Jr. The leukocyte count: a predictor of hypertension. J Clin Epidemiol. 1990;43:907–11.
Gillum RF, Mussolino ME. White blood cell count and hypertension incidence. the NHANES I epidemiologic follow-up study. J Clin Epidemiol. 1994;47:911–9.
Shankar AKB. Klein R. Relationship between white blood cell count and incident hypertension. Am J hypertension. 2004;17:233–9.
Sun YTGY, Zhu R, Liu X, Zhu Y, Wang Y, Qiu Q, et al. Relationship between white blood cells and hypertension in Chinese adults: the cardiometabolic risk in Chinese (CRC) study. Clin Exp Hypertens. 2015;37:594–8.
Nakanishi NSM, Shirai K, Suzuki K, Tatara K. White blood cell count as a risk factor for hypertension; a study of Japanese male office workers. J Hypertension. 2002;20:851–7.
Musial K, Bargenda-Lange A, Mazurkiewicz P, Gaik M, Gralec S, Zwolinska D. Lymphocyte to monocyte ratio and blood pressure variability in childhood hypertension-a pilot study. Pediatric Res. 2023;93:137–42.
Huang Lan, Qin Liu CS, Liang Xiaoyue, Ren Yanling, Huang Daochao, Guan Xianmin, et al. The associations between hematological parameters and the incidence of prehypertension and hypertension in children and adolescents: a prospective cohort study. Hypertension Res. 2023;46:2085–99.
Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387:957–67.
Tong J, An X, Zhao L, Qu P, Tang X, Chen M, et al. Combining multiaspect factors to predict the risk of childhood hypertension incidence. J Clin hypertension. 2022;24:1015–25.
Liang X, He Y, Chen M, Ping Q, Chen J. The association of lecithin retinol acyltransferase and the 25(OH)D receptor with pediatric overweight and obesity. Eur J Clin Nutr. 2019;73:1626–9.
Liang X, Su S, Hao G, Snieder H, Treiber F, Kapuku G, et al. Determinants of pulse wave velocity trajectories from youth to young adulthood: the Georgia stress and heart study. J hypertension. 2019;37:563–71.
Liang X, Chen J, An X, Liu F, Liang F, Tang X, et al. The impact of PM2.5 on children’s blood pressure growth curves: a prospective cohort study. Env Int. 2022;158:107012.
Wu, Dong Z, Tong J, Jiang X, LiqiangQin X. Evaluation of balanced diet pagodas in Chinese residents (2007). Mod Preventive Med. 2011;38:4835–9.
Fan H, Yan Y, Mi J. Updating blood pressure references for Chinese children aged 3-17 years. Chin J Hypertension. 2017;25:428–35.
Yang L, Magnussen CG, Bovet P, Xi B. Elevated blood pressure in childhood or adolescence and cardiovascular outcomes in adulthood: a systematic review. Hypertension. 2020;75:948–55.
Chen X, Wang Y. Tracking of blood pressure from childhood to adulthood: a systematic review and meta-regression analysis. Circulation. 2008;117:3171–80.
Thompson M, Dana T, Bougatsos C, Blazina I, Norris SL. Screening for hypertension in children and adolescents to prevent cardiovascular disease. Pediatrics. 2013;131:490–525.
Liang X, Xiao L, Luo Y, Xu J. Prevalence and risk factors of childhood hypertension in urban-rural areas of China: a cross-sectional study. Int J hypertension. 2020;2020:2374231.
Liang X, Xiao L, Luo Y, Xu J. Prevalence and risk factors of childhood hypertension from birth through childhood: a retrospective cohort study. J Hum Hypertens. 2020;34:151–64.
Mouton AJ, Li X, Hall ME, Hall JE. Obesity, hypertension, and cardiac dysfunction: novel roles of immunometabolism in macrophage activation and inflammation. Circ Res. 2020;126:789–806.
Mohammadi M, Ghazizadeh H, Mohammadi-Bajgiran M, Kathryn Bohn M, Yaghooti-Khorasani M, Kamel Khodabandeh A, et al. Pediatric reference intervals for hematology parameters in healthy infants and young children in Iran. Int J laboratory Hematol. 2023;45:845–52.
Zhang W, Wang Q, Liu H, Hong F, Tang Q, Hu C, et al. Systemic inflammation markers and the prevalence of hypertension in 8- to 17-year-old children and adolescents: a NHANES cross-sectional study. Nutrition, metabolism, cardiovascular Dis. 2025;35:103727.
Emamian M, Hasanian SM, Tayefi M, Bijari M, Movahedian Far F, Shafiee M, et al. Association of hematocrit with blood pressure and hypertension. J Clin laboratory Anal. 2017;31:e22124.
Khalid M, Miller C, Gebregziabher N, Guckien Z, Goswami S, Perkins A, et al. Factors affecting dialysis duration in children with Shiga toxin-producing Escherichia coli-associated hemolytic uremic syndrome. Pediatric nephrology. 2023;38:2753–61.
Wanner C, Iliev H, Duarte N, Schueler E, Soares AR, Thanam V, et al. Safety of empagliflozin: an individual participant-level data meta-analysis from four large trials. Adv Ther. 2024;41:2826–44.
Wyse CA, Celis Morales CA, Ward J, Lyall D, Smith DJ, Mackay D, et al. Population-level seasonality in cardiovascular mortality, blood pressure, BMI and inflammatory cells in UK biobank. Ann Med. 2018;50:410–9.
Tsuda K. A link between white blood cell count and blood pressure levels. Hypertension Res. 2024;47:537–9.
Guzik TJ, Nosalski R, Maffia P, Drummond GR. Immune and inflammatory mechanisms in hypertension. Nat Rev Cardiology. 2024;21:396–416.
Abais-Battad JM, Rudemiller NP, Mattson DL. Hypertension and immunity: mechanisms of T cell activation and pathways of hypertension. Curr Opin nephrology hypertension. 2015;24:470–4.
Li J, Imano H, Yamagishi K, Tanaka M, Cui R, Muraki I, et al. Leukocyte count and risks of stroke and coronary heart disease: the circulatory risk in communities study (CIRCS). J atherosclerosis thrombosis. 2022;29:527–35.
Kresovich JK, Xu Z, O’Brien KM, Parks CG, Weinberg CR, Sandler DP, et al. Peripheral immune cell composition is altered in women before and after a hypertension diagnosis. Hypertension. 2023;80:43–53.
de Simone G, Mancusi C, Hanssen H, Genovesi S, Lurbe E, Parati G, et al. Hypertension in children and adolescents. Eur heart J. 2022;43:3290–301.
Zhang Z, Zhao L, Zhou X, Meng X, Zhou X. Role of inflammation, immunity, and oxidative stress in hypertension: new insights and potential therapeutic targets. Front immunology. 2022;13:1098725.
Sha W, Zhao B, Wei H, Yang Y, Yin H, Gao J, et al. Astragalus polysaccharide ameliorates vascular endothelial dysfunction by stimulating macrophage M2 polarization via potentiating Nrf2/HO-1 signaling pathway. Phytomedicine. 2023;112:154667.
Pan W, Zhou G, Hu M, Li G, Zhang M, Yang H, et al. Coenzyme Q10 mitigates macrophage mediated inflammation in heart following myocardial infarction via the NLRP3/IL1β pathway. BMC cardiovascular Disord. 2024;24:76.
Gupta RM, Lee-Kim VS, Libby P. The march of monocytes in atherosclerosis: one cell at a time. Circulation Res. 2020;126:1324–6.
Wenzel P. Monocytes as immune targets in arterial hypertension. Br J pharmacology. 2019;176:1966–77.
Shapouri-Moghaddam A, Mohammadian S, Vazini H, Taghadosi M, Esmaeili SA, Mardani F, et al. Macrophage plasticity, polarization, and function in health and disease. J Cell Physiol. 2018;233:6425–40.
Medrano-Bosch M, Simon-Codina B, Jimenez W, Edelman ER, Melgar-Lesmes P. Monocyte-endothelial cell interactions in vascular and tissue remodeling. Front immunology. 2023;14:1196033.
Parihar A, Eubank TD, Doseff AI. Monocytes and macrophages regulate immunity through dynamic networks of survival and cell death. J innate Immun. 2010;2:204–15.
Kapellos TS, Bonaguro L, Gemund I, Reusch N, Saglam A, Hinkley ER, et al. Human monocyte subsets and phenotypes in major chronic inflammatory diseases. Front immunology. 2019;10:2035.
Thomas G, Tacke R, Hedrick CC, Hanna RN. Nonclassical patrolling monocyte function in the vasculature. Arteriosclerosis, thrombosis, Vasc Biol. 2015;35:1306–16.
Harwani SC. Macrophages under pressure: the role of macrophage polarization in hypertension. Transl Res. 2018;191:45–63.
Barhoumi T, Todryk S. Role of monocytes/macrophages in renin-angiotensin system-induced hypertension and end organ damage. Front Physiol. 2023;14:1199934.
Kang M, Jia H, Feng M, Ren H, Gao J, Liu Y, et al. Cardiac macrophages in maintaining heart homeostasis and regulating ventricular remodeling of heart diseases. Front immunology. 2024;15:1467089.
Harrison DG, Patrick DM. Immune mechanisms in hypertension. Hypertension. 2024;81:1659–74.
Azizi Z, Alipour P, Raparelli V, Norris CM, Pilote L. The role of sex and gender in hypertension. J Hum hypertension. 2023;37:589–95.
Klein SL, Flanagan KL. Sex differences in immune responses. Nat Rev Immunology. 2016;16:626–38.
Martin TG, Leinwand LA. Hearts apart: sex differences in cardiac remodeling in health and disease. J Clin investigation. 2024;134:e180074.
Becerra-Diaz M, Song M, Heller N. Androgen and androgen receptors as regulators of monocyte and macrophage biology in the healthy and diseased lung. Front immunology. 2020;11:1698.
Alvarez A, Hermenegildo C, Issekutz AC, Esplugues JV, Sanz MJ. Estrogens inhibit angiotensin II-induced leukocyte-endothelial cell interactions in vivo via rapid endothelial nitric oxide synthase and cyclooxygenase activation. Circ Res. 2002;91:1142–50.
Bowling MR, Xing D, Kapadia A, Chen YF, Szalai AJ, Oparil S, et al. Estrogen effects on vascular inflammation are age dependent: role of estrogen receptors. Arteriosclerosis, thrombosis, Vasc Biol. 2014;34:1477–85.
Gubbels Bupp MR, Jorgensen TN. Androgen-Induced immunosuppression. Front immunology. 2018;9:794.
Libert C, Dejager L, Pinheiro I. The X chromosome in immune functions: when a chromosome makes the difference. Nat Rev Immunology. 2010;10:594–604.
McPhee PG, Singh S, Morrison KM. Childhood obesity and cardiovascular disease risk: working toward solutions. Can J cardiology. 2020;36:1352–61.
Bridges AB, Fisher TC, Scott N, McLaren M, Belch JJ. Circadian rhythm of white blood cell aggregation and free radical status in healthy volunteers. Free Radic Res Commun. 1992;16:89–97.
Poursafa P, Kelishadi R, Amini A, Amini A, Amin MM, Lahijanzadeh M, et al. Association of air pollution and hematologic parameters in children and adolescents. J de Pediatr. 2011;87:350–6.
Varra FN, Varras M, Varra VK, Theodosis-Nobelos P. Molecular and pathophysiological relationship between obesity and chronic inflammation in the manifestation of metabolic dysfunctions and their inflammation‑mediating treatment options (Review). Mol Med Rep. 2024;29:95.
Acknowledgements
The authors would like to acknowledge all the children and the staffs of the surveyed schools in Chongqing.
Funding
This work was supported by the Natural Science Foundation Project (82373590), Chongqing Science and Technology Bureau and Health Commission joint project (2025ZDXM008, 2023MSXM036), General Project of Clinical Medical Research from National Clinical Research Center for Child Health and Disorders (No. NCRCCHD-2022-GP-01,NCRC-2020-GP-13), Major Health Project of Chongqing Science and Technology Bureau (No. CSTC2021jscx-gksb-N0001, CSTB2024NSCQ-MSX0180), Intelligent Medicine Project (No.ZHYX202109). The funders had no role in the whole study research process, including study design, data collection and analysis, the decision to publish, or the preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
DH, LC: Methodology; DH, XA, LC: Writing – Original Draft; XA, LC, XL: Writing - Review & Editing; XL: Study Design; SL, LX: Validation; XG, LX, XL:Resources; DH, LC, XA, XL: Investigation; XG, XA, XL: Supervision; XL: Conceptualization.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests
Ethical approval and consent to participate
Ethics Committee of the Children’s Hospital of Chongqing Medical University approved the study (No. 2019-86), and all procedures were conducted following the Declaration of Helsinki. All participants and their legal guardians provided written informed consents before inclusion in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41371_2026_1115_MOESM1_ESM.docx
Supplementary table 1. The difference of hemodynamic indexes for children under different levels of the variables for a cohort study
41371_2026_1115_MOESM2_ESM.docx
Supplementary table 2. The increased risk of the variables in men on elevated blood pressure compared with Q1 for a cohort study
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hu, D., Chen, L., Luo, S. et al. The relationship between white blood cell counts and pediatric hypertension: a prospective cohort study. J Hum Hypertens (2026). https://doi.org/10.1038/s41371-026-01115-y
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41371-026-01115-y