Abstract
Objective
To characterize the neural breathing pattern in preterm infants supported with non-invasive neurally adjusted ventilatory assist (NIV-NAVA).
Study Design
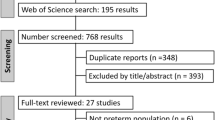
Single-center prospective observational study. The electrical activity of the diaphragm (EAdi) was periodically recorded in 30-second series with the Edi catheter and the Servo-n software (Maquet, Solna, Sweden) in preterm infants supported with NIV-NAVA. The EAdiPeak, EAdiMin, EAdiTonic, EAdiPhasic, neural inspiratory, and expiratory times (nTi and nTe) and the neural respiratory rate (nRR) were calculated. EAdi curves were generated by Excel for visual examination and classified according to the predominant pattern.
Results
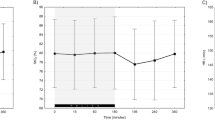
291 observations were analyzed in 19 patients with a mean GA of 27.3 weeks (range 24–36 weeks), birth weight 1028 g (510–2945 g), and a median (IQR) postnatal age of 18 days (4–27 days). The distribution of respiratory patterns was phasic without tonic activity 61.9%, phasic with basal tonic activity 18.6, tonic burst 3.8%, central apnea 7.9%, and mixed pattern 7.9%. In addition, 12% of the records showed apneas of >10 seconds, and 50.2% one or more “sighs”, defined as breaths with an EAdiPeak and/or nTi greater than twice the average EAdiPeak and/or nTi of the recording. Neural times were measurable in 252 observations. The nTi was, median (IQR): 279 ms (253–285 ms), the nTe 764 ms (642–925 ms), and the nRR 63 bpm (51–70), with a great intra and inter-subjects variability.
Conclusions
The neural breathing patterns in preterm infants supported with NIV-NAVA are quite variable and are characterized by the presence of significant tonic activity. Central apneas and sighs are common in this group of patients. The nTi seems to be shorter than the mechanical Ti commonly used in assisted ventilation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Beck J, Reilly M, Grasselli G, Qui H, Slutsky AS, Dunn MS, et al. Characterization of neural breathing pattern in spontaneously breathing preterm infants. Pediatr Res. 2011;70:607–13.
Aldrich TK, Sinderby C, McKenzie DK, Estenne M, Gandevia SC. Electrophysiologic techniques for the assessment of respiratory muscle function. American Thoracic Society/European Respiratory Society 2002 ATS/ERS Statement on Respiratory Muscle Testing. Am J Respir Crit Care Med. 2002;166:518–624.
Lopes J, Muller NL, Bryan MH, Bryan AC. Importance of inspiratory muscle tone in maintenance of FRC in the newborn. J Appl Physiol. 1981;51:830–4.
Emeriaud G, Beck J, Tucci M, Lacroix J, Sinderby C. Diaphragm electrical activity during expiration in mechanically ventilated infants. Pediatr Res. 2006;59:705–10.
Allo JC, Beck JC, Brander L, Brunet F, Slutsky AS, Sinderby CA. Influence of neurally adjusted ventilatory assist and positive end-expiratory pressure on breathing pattern in rabbits with acute lung injury. Crit Care Med. 2006;34:2997–3004.
Barwing J, Ambold M, Linden N, Quintel M, Moerer O. Evaluation of the catheter positioning for neurally adjusted ventilatory assist. Intensive Care Med. 2009;35:1809–14.
Meesen NE, van der Grinten CP, Folgering HT, Luijendijk SC. Tonic activity in inspiratory muscles during continuous negative airway pressure. Respir Physiol. 1993;92:151–66.
D’Angelo E, Pecchiari M, Acocella F, Monaco A, Bellemare F. Effects of abdominal distension on breathing pattern and respiratory mechanics in rabbits. Respir Physio Neurobiol. 2002;130:293–304.
Gunawardena S, Ravi K, Longhurst JC, Kaufman MP, Ma A, Bravo M, et al. Responses of C fiber afferents of the rabbit airway and lungs to changes in extra-vascular fluid volumen. Respir Physiol Neurobiol. 2002;132:239–51.
Ma A, Bravo M, Kappagoda CT. Responses of bronchial C-fiber afferents of the rabbit to changes in lung compliance. Respir Physiol Neurobiol. 2003;138:155–63.
Bonora M, Boule M, Gautier H. Diaphragmatic and ventilatory responses to alveolar hypoxia and hypercapnia in conscious kittens. J Appl Physiol (1985). 1992;72:203–10.
Stein HM, Wilmoth J, Burton J. Electrical activity of the diaphragm in a small cohort of term neonates. Respir Care. 2012;57:1483–7.
Mally PV, Beck J, Sinderby C, Caprio M, Bailey SM. Neural breathing pattern and patient-ventilator interaction during neurally adjusted ventilatory assist and conventional ventilation in newborns. Pediatr Crit Care Med. 2018;19:48–55.
Kosch PC, Stark AR. Dynamic maintenance of end-expiratory lung volume in full-term infants. J Appl Physiol. 1984;57:1126–33.
Kosch PC, Hutchinson AA, Wozniack JA, Carlo WA, Stark AR. Posterior cricoarytenoid and diaphragm activities during tidal breathing in neonates. J Appl Physiol (1985). 1988;64:1968–78.
Alvarez JE, Bodani J, Fajardo CA, Kwiatkowski K, Cates DB, Rigatto H. Sighs and their relationship to apnea in the newborn infant. Biol Neonate. 1993;63:139–46.
Parthasarathy S, Jubran A, Tobin MJ. Assessment of neural inspiratory time in ventilator-supported patients. Am J Respir Crit Care Med. 2000;162:546–52.
Lawson EE, Richter DW, Bischoff A. Intracellular recordings of respiratory neurons in the lateral medulla of piglets. J Appl Physiol. 1989;66:983–8.
Stark AR, Cohlan BA, Waggener TB, Frantz ID 3rd, Kosch PC. Regulation of end-expiratory lung volume during sleep in premature infants. J Appl Physiol. 1987;62:1117–23.
Arold SP, Bartolák-Suki E, Suki B. Variable stretch pattern enhances surfactant secretion in alveolar type II cells in culture. Am J Physiol Lung Cell Mol Physiol. 2009;296:L574–81.
Spieth PM, Carvalho AR, Pelosi P, Hoehn C, Meissner C, Kasper M, et al. Variable tidal volumes improve lung protective ventilation strategies in experimental lung injury. Am J Respir Crit Care Med. 2009;179:684–93.
García-Muñoz Rodrigo F, Urquía Marti L, Galán Henríquez G, Rivero Rodríguez S, Siles Quesada C. Neurally adjusted ventilatory assist increases respiratory variability and improves patient-ventilator synchronisation. Pediatr (Barc). 2016;84:231–2.
Acknowledgements
The authors thank all the nurses of the Neonatal Intensive Care Unit for their contribution to the collection of data and for their loving care of the patients and their families.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
García-Muñoz Rodrigo, F., Urquía Martí, L., Galán Henríquez, G. et al. Neural breathing patterns in preterm newborns supported with non-invasive neurally adjusted ventilatory assist. J Perinatol 38, 1235–1241 (2018). https://doi.org/10.1038/s41372-018-0152-5
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-018-0152-5
This article is cited by
-
Evaluating peak inspiratory pressures and tidal volume in premature neonates on NAVA ventilation
European Journal of Pediatrics (2021)