Abstract
Objective
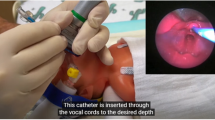
To compare surfactant administration via supraglottic airway device (SAD) vs. nasal CPAP alone or INSURE.
Study design
A systematic search of PubMed, EMBASE, SCOPUS, Cochrane Central Register of Controlled Trials and Clinicaltrials.gov was performed. Articles meeting inclusion criteria (RCT, surfactant administration via SAD, laryngeal mask, I-gel) were assessed
Results
Five RCTs were eligible. Surfactant administration via SAD reduced the need for intubation/mechanical ventilation (RR 0.57, 95%CI 0.38–0.85) and short-term oxygen requirements (MD −8.00, 95%CI −11.09 to −4.91) compared to nCPAP alone. Surfactant administration via SAD reduced the need for intubation/mechanical ventilation (RR 0.43, 95%CI 0.31–0.61), but increased short-term oxygen requirements (MD 3.10, 95%CI 0.51–5.69) compared to INSURE approach.
Conclusions
In preterm infants with RDS, surfactant administration via SAD reduces the need for intubation/mechanical ventilation. Overall, available literature includes few, small, poor-quality studies. Surfactant administration via SAD should be limited to clinical trials.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
References
Owen LS, Manley BJ, Davis PG, Doyle LW. The evolution of modern respiratory care for preterm infants. Lancet. 2017;389:1649–59.
Warren JB, Anderson JM. Core concepts: respiratory distress syndrome. NeoReviews. 2009;10:351–61.
Seger N, Soll R. Animal derived surfactant extract for treatment of respiratory distress syndrome. Cochrane Database Syst Rev. 2009;2:CD007836.
Soll RF. Synthetic surfactant for respiratory distress syndrome in preterm infants. Cochrane Database Syst Rev. 2000;CD001149.
Bahadue FL, Soll R. Early versus delayed selective surfactant treatment for neonatal respiratory distress syndrome. Cochrane Database Syst Rev. 2012;11:CD001456.
Sardesai S, Biniwale M, Wertheimer F, Garingo A, Ramanathan R. Evolution of surfactant therapy for respiratory distress syndrome: past, present, and future. Pediatr Res. 2017;81:240–8.
Verder H, Robertson B, Greisen G, Ebbesen F, Albertsen P, Lundstrøm K, et al. Surfactant therapy and nasal continuous positive airway pressure for newborns with respiratory distress syndrome. Danish-Swedish Multicenter Study Group. N Engl J Med. 1994;331:1051–5.
Carbajal R, Eble B, Anand KJ. Premedication for tracheal intubation in neonates: confusion or controversy? Semin Perinatol. 2007;31:309–17.
Marshall TA, Deeder R, Pai S, Berkowitz GP, Austin TL. Physiologic changes associated with endotracheal intubation in preterm infants. Crit Care Med. 1984;12:501–3.
Ghanta S, Abdel-Latif ME, Lui K, Ravindranathan H, Awad J, Oei J. Propofol compared with the morphine, atropine, and suxamethonium regimen as induction agents for neonatal endotracheal intubation: a randomized, controlled trial. Pediatrics. 2007;119:e1248–1255.
Kribs A, Roll C, Göpel W, Wieg C, Groneck P, Laux R, et al. NINSAPP trial investigators. nonintubated surfactant application vs conventional therapy in extremely preterm infants: a randomized clinical trial. JAMA Pediatr. 2015;169:723–30.
Dargaville PA, Aiyappan A, De Paoli AG, Kuschel CA, Kamlin CO, Carlin JB, et al. Minimally-invasive surfactant therapy in preterm infants on continuous positive airway pressure. Arch Dis Child Fetal Neonatal Ed. 2013;98:F122–6.
More K, Sakhuja P, Shah PS. Minimally invasive surfactant administration in preterm infants: a meta-narrative review. JAMA Pediatr. 2014;168:901–8.
Oncel MY, Arayici S, Uras N, Alyamac-Dizdar E, Sari FN, Karahan S, et al. Nasal continuous positive airway pressure versus nasal intermittent positive-pressure ventilation within the minimally invasive surfactant therapy approach in preterm infants: a randomised controlled trial. Arch Dis Child Fetal Neonatal Ed. 2016;101:F323–8.
Brimacombe J, Gandini D, Keller C. The laryngeal mask airway for administration of surfactant in two neonates with respiratory distress syndrome. Paediatr Anaesth. 2004;14:188–90.
Trevisanuto D, Grazzina N, Ferrarese P, Micaglio M, Verghese C, Zanardo V. Laryngeal mask airway used as a delivery conduit for the administration of surfactant to preterm infants with respiratory distress syndrome. Biol Neonate. 2005;87:217–20.
Hohlrieder M, Brimacombe J, von Goedecke A, Keller C. Postoperative nausea, vomiting, airway morbidity, and analgesic requirements are lower for the ProSeal laryngeal mask airway than the tracheal tube in females undergoing breast and gynaecological surgery. Br J Anaesth. 2007;99:576–80.
van Esch BF, Stegeman I, Smit AL. Comparison of laryngeal mask airway vs tracheal intubation: a systematic review on airway complications. J Clin Anesth. 2017;36:142–50.
Trevisanuto D, Micaglio M, Ferrarese P, Zanardo V. The laryngeal mask airway: potential applications in neonates. Arch Dis Child Fetal Neonatal Ed. 2004;89:F485–9.
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. Cochrane Bias Methods G, Cochrane Statistical Methods G. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Schünemann H, Brozek J, Guyatt G, Oxman A (eds). GRADE Working Group. GRADE handbook for grading quality of evidence and strength of recommendations. https://gdt.gradepro.org/app/handbook/handbook.html. Accessed October 2013.
GRADE Working Group, McMaster University. GRADEpro GDT Version. Hamilton, ON: GRADE Working Group, McMaster University; 2014.
GRADEpro. GDT. https://gradepro.org. Accessed 8 April 2018.
Roberts KD, Brown R, Lampland AL, Leone TA, Rudser KD, Finer NN, et al. Laryngeal mask airway for surfactant administration in neonates: a randomized, controlled trial. J Pediatr. 2018;193:40–46.e1.
Pinheiro JM, Santana-Rivas Q, Pezzano C. Randomized trial of laryngeal mask airway versus endotracheal intubation for surfactant delivery. J Perinatol. 2016;36:196–201.
Attridge JT, Stewart C, Stukenborg GJ, Kattwinkel J. Administration of rescue surfactant by laryngeal mask airway: lessons from a pilot trial. Am J Perinatol. 2013;30:201–6.
Barbosa RF, ESAC Simoes, Silva. YP. A randomized controlled trial of the laryngeal mask airway for surfactant administration in neonates. J Pediatr. 2017;93:343–50.
Sadeghnia A, Tanhaei M, Mohammadizadeh M, Nemati M. A comparison of surfactant administration through i-gel and ET-tube in the treatment of respiratory distress syndrome in newborns weighing more than 2000 g. Adv Biomed Res. 2014;3:1–6.
Review Manager (RevMan) Version 5.3 [Computer program]. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration; 2014. P.
Doglioni N, Cavallin F, Zanardo V, Trevisanuto D. Intubation training in neonatal patients: a review of one trainee’s first 150 procedures. J Matern Fetal Neonatal Med. 2012;25:1302–4.
Abdel-Latif ME, Osborn DA. Laryngeal mask airway surfactant administration for prevention of morbidity and mortality in preterm infants with or at risk of respiratory distress syndrome. Cochrane Database Syst Rev. 2011;CD008309.
Barbosa RF, Marcatto Jde O, Silva AC, Silva YP. ProSealTM laryngeal mask airway for surfactant administration in the treatment of respiratory distress syndrome in a premature infant. Rev Bras Ter Intensiv. 2012;24:207–10.
Trevisanuto D, Doglioni N, Mario F, Micaglio M, Parotto M, Zanardo V. Drug administration via the laryngeal mask airway. Resuscitation. 2006;71:263–4.
Micaglio M, Zanardo V, Ori C, Parotto M, Doglioni N, Trevisanuto D, et al. for surfactant administration. Paediatr Anaesth. 2008;18:91–92.
Vannozzi CiantelliM, Moscuzza F, Scaramuzzo RT, Panizza D, Sigali E, et al. Catheter and Laryngeal mask endotracheal surfactant therapy: the CALMEST approach as a novel MIST technique. J Matern Fetal Neonatal Med. 2017;30:2375–7.
Acknowledgements
We thank Dr. Stubbs Brendon, Institute of Psychiatry, Psychology and Neuroscience, Kings College London, UK for helping in literature search. We are grateful to the authors of 5 included trials for providing additional study information for this systematic review.
Author contributions
MGC analyzed the data, contributed to interpret the results and draft the manuscript, and approved the final manuscript as submitted. NV conceived and designed the study, contributed to the data analysis, and approved the final manuscript as submitted. FC contributed to interpret the results and draft the manuscript, and approved the final manuscript as submitted. PC and MM conducted the literature search, extracted key data from the included articles, critically revised the manuscript, and approved the final manuscript as submitted. DT conceived and designed the study, drafted the manuscript, and approved the final manuscript as submitted. All the Authors are responsible for the accuracy and the integrity of the data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Calevo, M.G., Veronese, N., Cavallin, F. et al. Supraglottic airway devices for surfactant treatment: systematic review and meta-analysis. J Perinatol 39, 173–183 (2019). https://doi.org/10.1038/s41372-018-0281-x
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-018-0281-x