Abstract
Objective
To evaluate an implementation of lower oxygen saturation targets with retinopathy of prematurity (ROP) as primary outcome, in infants at the lowest extreme of prematurity.
Study design
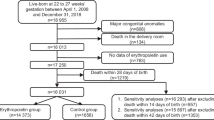
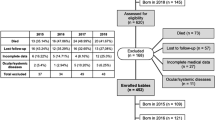
Retrospective cohort including infants born at 22–25 weeks of gestation in 2005–2015 (n = 325), comparing high (87–93%) and low (85–90%) targets; infants transferred early were excluded from the main analysis to avoid bias.
Results
Overall survival was 76% in high saturation era, and 69% in low saturation era (p = .17). Treatment-requiring ROP was less common in low saturation group (14% vs 28%, p < .05) with the most prominent difference in the most immature infants. Including deceased infants in the analysis, necrotizing enterocolitis was more frequent in low saturation era (21% vs 10%, p < .05).
Conclusions
Implementing lower saturation targets resulted in a halved incidence of treatment-requiring ROP; the most immature infants seem to benefit the most. An association between lower oxygenation and necrotizing enterocolitis cannot be excluded.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Hellström A, Smith LE, Dammann O. Retinopathy of prematurity. Lancet. 2013;382:1445–57.
Hartnett ME, Penn JS. Mechanisms and management of retinopathy of prematurity. N Engl J Med. 2012;367:2515–26.
Blencowe H, Lawn JE, Vazquez T, Fielder A, Gilbert C. Preterm-associated visual impairment and estimates of retinopathy of prematurity at regional and global levels for 2010. Pediatr Res. 2013;74:35–49.
Holmström GE, Källen K, Hellström A, Jakobsson PG, Serenius F, Stjernqvist K, et al. Ophthalmologic outcome at 30 months’ corrected age of a prospective Swedish cohort of children born before 27 weeks of gestation: the extremely preterm infants in Sweden study. JAMA Ophthalmol. 2014;132:182–9.
Cummings JJ, Polin RA, COMMITTEE ON FETUS AND NEWBORN. Oxygen targeting in extremely low birth weight infants. Pediatrics. 2016;138:e20161576.
Cayabyab R, Ramanathan R. Retinopathy of prematurity: therapeutic strategies based on pathophysiology. Neonatology. 2016;109:369–76.
Askie LM, Henderson-Smart DJ, Irwig L, Simpson JM. Oxygen-saturation targets and outcomes in extremely preterm infants. N Engl J Med. 2003;349:959–67.
Chow LC, Wright KW, Sola A, CSMC Oxygen Administration Study Group. Can changes in clinical practice decrease the incidence of severe retinopathy of prematurity in very low birth weight infants? Pediatrics. 2003;111:339–45.
Chen M, Çitil A, McCabe F, Leicht KM, Fiascone J, Dammann CEL, et al. Infection, oxygen, and immaturity: interacting risk factors for retinopathy of prematurity. Neonatology. 2011;99:125–32.
Wu C, Löfqvist C, Smith LEH, VanderVeen DK, Hellström A. WINROP consortium. importance of early postnatal weight gain for normal retinal angiogenesis in very preterm infants: a multicenter study analyzing weight velocity deviations for the prediction of retinopathy of prematurity. Arch Ophthalmol. 2012;130:992–9.
SUPPORT Study Group of the Eunice Kennedy Shriver NICHD Neonatal Research Network, Carlo WA, Finer NN, Walsh MC, Rich W, Gantz MG, et al. Target ranges of oxygen saturation in extremely preterm infants. N Engl J Med. 2010;362:1959–69.
Stenson B, Brocklehurst P, Tarnow-Mordi W. U.K. BOOST II trial, Australian BOOST II trial, New Zealand BOOST II trial. Increased 36-week survival with high oxygen saturation target in extremely preterm infants. N Engl J Med. 2011;364:1680–2.
BOOST II United Kingdom Collaborative Group, BOOST II Australia Collaborative Group, BOOST II New Zealand Collaborative Group, Stenson BJ, Tarnow-Mordi WO, Darlow BA, et al. Oxygen saturation and outcomes in preterm infants. N Engl J Med. 2013;368:2094–104.
BOOST-II Australia and United Kingdom Collaborative Groups, Tarnow-Mordi W, Stenson B, Kirby A, Juszczak E, Donoghoe M, et al. Outcomes of two trials of oxygen-saturation targets in preterm infants. N Engl J Med. 2016;374:749–60.
Stenson BJ. Oxygen saturation targets for extremely preterm infants after the NeOProM trials. Neonatology. 2016;109:352–8.
Holmström GE, Hellström A, Jakobsson PG, Lundgren P, Tornqvist K, Wallin A. Swedish national register for retinopathy of prematurity (SWEDROP) and the evaluation of screening in Sweden. Arch Ophthalmol. 2012;130:1418–24.
International Committee for the Classification of Retinopathy of Prematurity. The international classification of retinopathy of prematurity revisited. Arch Ophthalmol. 2005;123:991–9.
Early Treatment For Retinopathy Of Prematurity Cooperative Group. Revised indications for the treatment of retinopathy of prematurity: results of the early treatment for retinopathy of prematurity randomized trial. Arch Ophthalmol. 2003;121:1684–94.
Niklasson A, Albertsson-Wikland K. Continuous growth reference from 24th week of gestation to 24 months by gender. BMC Pediatr. 2008;8:8.
Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001;163:1723–9.
Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1500 g. J Pediatr. 1978;92:529–34.
Kapadia VS, Lal CV, Kakkilaya V, Heyne R, Savani RC, Wyckoff MH. Impact of the neonatal resuscitation program-recommended low oxygen strategy on outcomes of infants born preterm. J Pediatr. 2017;191:35–41.
Askie LM, Brocklehurst P, Darlow BA, Finer N, Schmidt B, Tarnow-Mordi W, et al. NeOProM: neonatal oxygenation prospective meta-analysis collaboration study protocol. BMC Pediatr. 2011;11:6.
Darlow BA, Marschner SL, Donoghoe M, Battin MR, Broadbent RS, Elder MJ, et al. Randomized controlled trial of oxygen saturation targets in very preterm infants: 2 year outcomes. J Pediatr. 2014;165:30–35.e2.
Schmidt B, Whyte RK, Asztalos EV, Moddemann D, Poets C, Rabi Y, et al. Effects of targeting higher vs lower arterial oxygen saturations on death or disability in extremely preterm infants: a randomized clinical trial. JAMA. 2013;309:2111–20.
Schmidt B, Whyte RK, Shah PS, Abbasi S, Bairam A, Harrold J, et al. Effects of targeting higher or lower oxygen saturations in centers with more versus less separation between median saturations. J Pediatr. 2016;178:288–.e2.
Whyte RK, Nelson H, Roberts RS, Schmidt B. Benefits of oxygen saturation targeting trials: oximeter calibration software revision and infant saturations. J Pediatr. 2017;182:382–4.
Sweet DG, Carnielli V, Greisen G, Hallman M, Ozek E, Plavka R, et al. European consensus guidelines on the management of respiratory distress syndrome—2016 update. Neonatology. 2017;111:107–25.
Tin W, Milligan DWA, Pennefather P, Hey E. Pulse oximetry, severe retinopathy, and outcome at one year in babies of less than 28 weeks gestation. Arch Dis Child Fetal Neonatal Ed. 2001;84:F106–F110.
Deulofeut R, Critz A, Adams-Chapman I, Sola A. Avoiding hyperoxia in infants ≤ 1250 g is associated with improved short and long-term outcomes. J Perinatol. 2006;26:700–5.
Castillo A, Deulofeut R, Critz A, Sola A. Prevention of retinopathy of prematurity in preterm infants through changes in clinical practice and SpO2 technology. Acta Paediatr. 2010;100:188–92.
Cayabyab R, Arora V, Wertheimer F, Durand M, Ramanathan R. Graded oxygen saturation targets and retinopathy of prematurity in extremely preterm infants. Pediatr Res. 2016;80:401–6.
Urrets-Zavalia JA, Crim N, Knoll EG, Esposito FA, Collino E, Urrets-Zavalia ME, et al. Impact of changing oxygenation policies on retinopathy of prematurity in a neonatal unit in Argentina. Br J Ophthalmol. 2012;96:1456–61.
Wright KW, Sami D, Thompson L, Ramanathan R, Joseph R, Farzavandi S. A physiologic reduced oxygen protocol decreases the incidence of threshold retinopathy of prematurity. Trans Am Ophthalmol Soc. 2006;104:78–84.
Manley BJ, Kuschel CA, Elder JE, Doyle LW, Davis PG. Higher rates of retinopathy of prematurity after increasing oxygen saturation targets for very preterm infants: experience in a single center. J Pediatr. 2016;168:242–4.
Sears JE, Sonnie C, Hoppe G. Incidence of ROP after suppoRT. Invest Ophthalmol Vis Sci. 2016;57:6287–6287.
Serenius F, Blennow M, Maršál K, Sjörs G, Källen K, Group for the ES. Intensity of perinatal care for extremely preterm infants: outcomes at 2.5 years. Pediatrics. 2015;135:e1163–e1172.
Backes CH, Rivera BK, Haque U, Srouji L, Beck S, Yin H, et al. A proactive approach to neonates born at 23 weeks of gestation. Obstet Gynecol. 2015;126:939–46.
Backes CH, Söderström F, Ågren J, Sindelar R, Bartlett CW, Rivera BK et al. Outcomes following a comprehensive versus a selective approach for infants born at 22 weeks of gestation. J Perinatol. 2018. https://doi.org/10.1038/s41372-018-0248-y.
Mehler K, Oberthuer A, Keller T, Becker I, Valter M, Roth B, et al. Survival among infants born at 22 or 23 weeks’ gestation following active prenatal and postnatal care. JAMA Pediatr. 2016;170:671–7.
Ishii N, Kono Y, Yonemoto N, Kusuda S, Fujimura M. Neonatal research network, Japan. outcomes of infants born at 22 and 23 weeks’ gestation. Pediatrics. 2013;132:62–71.
Santhakumaran S, Statnikov Y, Gray D, Battersby C, Ashby D, Modi N. Survival of very preterm infants admitted to neonatal care in England 2008–2014: time trends and regional variation. Arch Dis Child Fetal Neonatal Ed. 2018;103:F208–F215.
Baron IS, Weiss BA, Baker R, Ahronovich MD, Litman FR, Baveja R. Neuropsychological outcomes in extremely preterm preschoolers exposed to tiered low oxygen targets: an observational study. J Int Neuropsychol Soc. 2016;22:322–31.
Hergenhan A, Steurer M, Berger TM. Gestational age-adapted oxygen saturation targeting and outcome of extremely low gestational age neonates (ELGANs). Swiss Med Wkly. 2015;145:w14197.
Walsh MC, Fiore JMD, Martin RJ, Gantz M, Carlo WA, Finer N. Association of oxygen target and growth status with increased mortality in small for gestational age infants: further analysis of the surfactant, positive pressure and pulse oximetry randomized trial. JAMA Pediatr. 2016;170:292–4.
Lakshminrusimha S, Manja V, Mathew B, Suresh GK. Oxygen targeting in preterm infants: a physiologic interpretation. J Perinatol J Calif Perinat Assoc. 2015;35:8–15.
Acknowledgements
Funding
This study was supported by Födelsefonden and Gillbergska stiftelsen.
Author contributions
FS contributed to study design and conceptualization, is responsible for data collection, contributed to data analysis and interpretation, and drafted, reviewed, and revised the manuscript. EN assisted in data collection, contributed to data analysis and interpretation, and reviewed and revised the manuscript. GH, EL, and FA assisted in data collection and interpretation, and reviewed and revised the manuscript. RS contributed to data interpretation, and critically reviewed the manuscript for important intellectual content. JA contributed to study design and conceptualization, data analysis and interpretation, and drafted, reviewed, and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Söderström, F., Normann, E., Holmström, G. et al. Reduced rate of treated retinopathy of prematurity after implementing lower oxygen saturation targets. J Perinatol 39, 409–414 (2019). https://doi.org/10.1038/s41372-018-0300-y
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-018-0300-y