Abstract
Objective
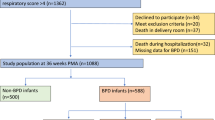
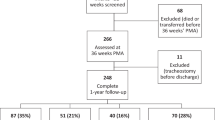
To compare pulmonary function in extremely low birth weight (ELBW) infants with bronchopulmonary dysplasia (BPD) studied at 34–36 weeks postmenstrual age (PMA) with a reference group of “healthy” infants born at 34–36 weeks. We hypothesized that ELBW infants have decreased functional residual capacity (FRC) and respiratory compliance (Crs).
Study design
Pulmonary function testing was performed at 34–36 weeks PMA in infants with BPD and within 96 h of age in infants delivered at 34–36 weeks.
Results
Twenty BPD patients and 20 healthy infants were studied. FRC (18.9 versus 26.2 mL/kg; adjusted 95% CI 5.0, 10.9; P < 0.001) and Crs (0.80 versus 1.29-mL/cm H2O/kg; 95% CI 0.31, 0.71; P < 0.001) were decreased in BPD patients. Respiratory resistance was increased in BPD patients.
Conclusions
ELBW infants with BPD have decreased pulmonary function compared to healthy infants delivered at 34–36 weeks. This suggests that infants with BPD have smaller lung volumes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001;163:1723–9.
Northway WH Jr, Rosan RC, Porter DY. Pulmonary disease following respirator therapy of hyaline-membrane disease. Bronchopulmonary dysplasia. N Engl J Med. 1967;276:357–68.
Baraldi E, Filippone M. Chronic lung disease after premature birth. N Engl J Med. 2007;357:1946–55.
Coalson JJ. Pathology of bronchopulmonary dysplasia. Semin Perinatol. 2006;30:179–84.
McEvoy CT, Jain L, Schmidt B, Abman S, Bancalari E, Aschner JL. Bronchopulmonary dysplasia: NHLBI Workshop on the Primary Prevention of Chronic Lung Diseases. Ann Am Thorac Soc. 2014;11:S146–53.
Shepherd EG, Clouse BJ, Hasenstab KA, Sitaram S, Malleske DT, Nelin LD, et al. Infant pulmonary function testing and phenotypes in severe bronchopulmonary dysplasia. Pediatrics. 2018;141:e20173350.
Doyle LW, Faber B, Callanan C, Freezer N, Ford GW, Davis NM. Bronchopulmonary dysplasia in very low birth weight subjects and lung function in late adolescence. Pediatrics. 2006;118:108–13.
McEvoy C, Venigalla S, Schilling D, Clay N, Spitale P, Nguyen T. Respiratory function in healthy late preterm infants delivered at 33-36 weeks of gestation. J Pediatr. 2013;162:464–9.
Yuksel B, Greenough A, Chan V, Russell RR. Comparison of helium dilution and nitrogen washout measurements of functional residual capacity in premature infants. Pediatr Pulmonol. 1993;16:197–200.
Gerhardt T, Hehre D, Bancalari E, Watson H. A simple method for measuring functional residual capacity by N2 washout in small animals and newborn infants. Pediatr Res. 1985;19:1165–9.
Gappa M, Colin AA, Goetz I, Stocks J. Passive respiratory mechanics: the occlusion techniques. Eur Respir J. 2001;17:141–8.
Go M, Schilling D, Nguyen T, Durand M, McEvoy CT. Respiratory compliance in late preterm infants (340/7–346/7 weeks) after antenatal steroid therapy. J Pediatr. 2018;201:21–26.
Morris MG, Gustafsson P, Tepper R, Gappa M, Stocks J. The bias flow nitrogen washout technique for measuring the functional residual capacity in infants. ERS/ATS Task Force on Standards for Infant Respiratory Function Testing. Eur Respir J. 2001;17:529–36.
McEvoy C, Schilling D, Spitale P, Peters D, O’Malley J, Durand M. Decreased respiratory compliance in infants less than or equal to 32 weeks’ gestation, delivered more than 7 days after antenatal steroid therapy. Pediatrics. 2008;121:e1032–8.
McEvoy CT, Schilling D, Clay N, Jackson K, Go MD, Spitale P, et al. Vitamin C supplementation for pregnant smoking women and pulmonary function in their newborn infants: a randomized clinical trial. JAMA. 2014;311:2074–82.
Brown H, Prescott R. Applied mixed models in medicine. Chichester, United Kingdom: John Wiley and Sons; 2003.
Friedrich L, Pitrez PM, Stein RT, Goldani M, Tepper R, Jones MH. Growth rate of lung function in healthy preterm infants. Am J Respir Crit Care Med. 2007;176:1269–73.
Martinez FJ, Han MK, Allinson JP, Barr RG, Boucher RC, Calverley PMA, et al. At the root: defining and halting progression of early chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2018;197:1540–51.
Stern DA, Morgan WJ, Wright AL, Guerra S, Martinez FD. Poor airway function in early infancy and lung function by age 22 years: a non-selective longitudinal cohort study. Lancet. 2007;370:758–64.
McEvoy CT, Shorey-Kendrick LE, Milner K, Schilling D, Tiller C, Vuylsteke B, et al. Oral vitamin C (500 mg/day) to pregnant smokers improves infant airway function at 3 months (VCSIP): a randomized trial. Am J Respir Crit Care Med. 2019;199:1139–47.
Morrow LA, Wagner BD, Ingram DA, Poindexter BB, Schibler K, Cotton CM, et al. Antenatal determinants of bronchopulmonary dysplasia and late respiratory disease in preterm infants. Am J Respir Crit Care Med. 2017;196:364–74.
Stocks J, Hislop A, Sonnappa S. Early lung development: lifelong effect on respiratory health and disease. Lancet Respir Med. 2013;1:728–42.
Kotecha SJ, Edwards MO, Watkins WJ, Henderson AJ, Paranjothy S, Dunstan FD, et al. Effect of preterm birth on later FEV1: a systematic review and meta-analysis. Thorax. 2013;68:760–6.
McEvoy C, Schilling D, Peters D, Tillotson C, Spitale P, Wallen L, et al. Respiratory compliance in preterm infants after a single rescue course of antenatal steroids: a randomized controlled trial. Am J Obstet Gynecol. 2010;202:544.e1–544.e9.
Dinger J, Topfer A, Schaller P, Schwarze R. Functional residual capacity and compliance of the respiratory system after surfactant treatment in premature infants with severe respiratory distress syndrome. Eur J Pediatr. 2002;161:485–90.
Baraldi E, Filippone M, Trevisanuto D, Zanardo V, Zacchello F. Pulmonary function until two years of life in infants with bronchopulmonary dysplasia. Am J Respir Crit Care Med. 1997;155:149–55.
Hjalmarson O, Sandberg KL. Lung function at term reflects severity of bronchopulmonary dysplasia. J Pediatr. 2005;146:86–90.
Plopper CG, Nishio SJ, Schelegle ES. Tethering tracheobronchial airways within the lungs. Am J Respir Crit Care Med. 2003;167:2–3.
Colin AA, McEvoy C, Castile RG. Respiratory morbidity and lung function in preterm infants of 32 to 36 weeks’ gestational age. Pediatrics. 2010;126:115–28.
Hjalmarson O, Sandberg K. Abnormal lung function in healthy preterm infants. Am J Respir Crit Care Med. 2002;165:83–7.
Goyal NK, Fiks AG, Lorch SA. Association of late-preterm birth with asthma in young children: practice based study. Pediatrics. 2011;128:e830–8.
Doyle LW, Ford GW, Olinsky A, Knoches AM, Callanan C. Bronchopulmonary dysplasia and very low birthweight: lung function at 11 years of age. J Paediatr Child Health. 1996;32:339–43.
Doyle LW. Respiratory function at age 8-9 years in extremely low birthweight/very preterm children born in Victoria in 1991-1992. Pediatr Pulmonol. 2006;41:570–6.
Korhonen P, Laitinen J, Hyodynmaa E, Tammela O. Respiratory outcome in school-aged, very-low-birth-weight children in the surfactant era. Acta Paediatr. 2004;93:316–21.
Jones MH, Davis SD, Grant D, Christoph K, Kisling J, Tepper RS. Forced expiratory maneuvers in very young children. Assessment of flow limitation. Am J Respir Crit Care Med. 1999;159:791–5.
Morrow DK, Schilling D, McEvoy CT. Response to bronchodilators in very preterm infants with evolving bronchopulmonary dysplasia. Res Rep Neonatol. 2015;5:113–7.
Lam R, Schilling D, Scottoline B, Platteau A, Niederhausen M, Lund KC, et al. The effect of extended continuous positive airway pressure on changes in lung volumes in stable premature infants: a randomized controlled trial. J Pediatr. 2020;217:66–72.e1.
Thebaud B. Mesenchymal stromal cell therapy for respiratory complications of extreme prematurity. Am J Perinatol. 2018;35:566–9.
Acknowledgements
The authors would like to thank the neonatologists, obstetricians, neonatal fellows, and the staff of our Neonatal Intensive Care Unit for their help with the study.
Funding
Supported by NIH/NHLBI (K23 HL080231 and R01 HL105447), Office of Dietary Supplements to CTM.
Author information
Authors and Affiliations
Contributions
Drafting the manuscript: all authors; data analysis: SM.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
McEvoy, C.T., Schilling, D., Go, M.D. et al. Pulmonary function in extremely low birth weight infants with bronchopulmonary dysplasia before hospital discharge. J Perinatol 41, 77–83 (2021). https://doi.org/10.1038/s41372-020-00856-z
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-020-00856-z
This article is cited by
-
Is small for gestational age associated with reduced oxygen saturation to FiO2 ratio at 36 weeks postmenstrual age in preterm infants, independent of bronchopulmonary dysplasia? A retrospective Italian two-center cohort study
European Journal of Pediatrics (2026)
-
How to personalise ventilation of infants with congenital diaphragmatic hernia? A simulation study
BMC Pediatrics (2025)
-
Pulmonary function tests in the neonatal intensive care unit and beyond: a clinical review
Journal of Perinatology (2025)
-
Prematurity-associated wheeze: current knowledge and opportunities for further investigation
Pediatric Research (2023)
-
Dose-dependent impact of human milk feeding on tidal breathing flow-volume loop parameters across the first 2 years of life in extremely low-birth-weight infants: a cohort study
European Journal of Pediatrics (2023)