Abstract
Objective
To understand the nutritional intake and growth outcomes of very low birth weight infants with surgical necrotizing enterocolitis (NEC).
Study design
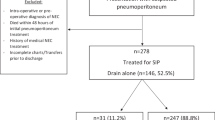
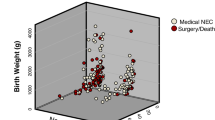
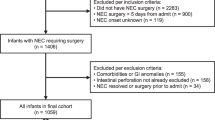
In a retrospective cohort study, linear mixed models were used to compare growth outcomes from birth to 24 months corrected age for very low birth weight (VLBW) infants with surgical NEC to those with spontaneous intestinal perforation (SIP). Kaplan-Meier curves were developed to demonstrate the duration of parenteral nutrition (PN) use.
Result
Height differed by surgical NEC and SIP over time (interaction p = 0.03). Surviving infants with surgical NEC had lower head circumference z-scores at 24 months. Of infants surviving surgical NEC, 71% received PN for >60 days after diagnosis.
Conclusion
The majority of infants with surgical NEC have a delay in achieving enteral autonomy. There was a difference in linear catch-up growth over time between infants with SIP and surgical NEC at 24 months.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Engelstad HJ, Danko ME. Short Bowel syndrome in an infant. NeoReviews. 2020;21:e370–e382.
Ehrenkranz RA, Dusick AM, Vohr BR, Wright LL, Wrage LA, Poole WK. Growth in the neonatal intensive care unit influences neurodevelopmental and growth outcomes of extremely low birth weight infants. Pediatrics. 2006;117:1253–61.
Lin GC, Robinson DT, Olsen S, Reber KM, Moallem M, DiGeronimo R, et al. Nutritional practices and growth in premature infants after surgical necrotizing enterocolitis. J Pediatr Gastroenterol Nutr. 2017;65:111–6.
Duggan CP, Jaksic T. Pediatric intestinal failure. N Engl J Med. 2017;377:666–75.
Goddard GR, McNelis K, Poindexter A, Jenkins T, Wessel J, Nathan AT, et al. Quality improvement efforts reduce incidence of surgical necrotizing enterocolitis and related deaths. Am J Perinatol. 2020 Jun 8. https://doi.org/10.1055/s-0040-1712967. Online ahead of print.
Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L, et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg. 1978;187:1–7.
Neu J. Necrotizing enterocolitis: the search for a unifying pathogenic theory leading to prevention. Pediatr Clin North Am. 1996;43:409–32.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81.
Fenton TR, Kim JH. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 2013;13:59.
WHO. Child growth standards based on length/height, weight and age. Acta Paediatr Suppl. 2006, 450:76–85.
Struijs MC, Diamond IR, de Silva N, Wales PW. Establishing norms for intestinal length in children. J Pediatr Surg. 2009;44:933–8.
Fenton TR, Cormack B, Goldberg D, Nasser R, Alshaikh B, Eliasziw M, et al. “Extrauterine growth restriction” and “postnatal growth failure” are misnomers for preterm infants. J Perinatol. 2020;40:704–14.
Guellec I, Lapillonne A, Marret S, Picaud JC, Mitanchez D, Charkaluk ML, et al. Effect of intra- and extrauterine growth on long-term neurologic outcomes of very preterm infants. J Pediatr. 2016;175:93–99.e91.
Meyers JM, Bann CM, Stoll BJ, D’Angio CT, Bell EF, Duncan AF, et al. Neurodevelopmental outcomes in postnatal growth-restricted preterm infants with postnatal head-sparing. J Perinatol. 2016;36:1116–21.
Neubauer V, Griesmaier E, Pehböck-Walser N, Pupp-Peglow U, Kiechl-Kohlendorfer U. Poor postnatal head growth in very preterm infants is associated with impaired neurodevelopment outcome. Acta Paediatr. 2013;102:883–8.
Matei A, Montalva L, Goodbaum A, Lauriti G, Zani A. Neurodevelopmental impairment in necrotising enterocolitis survivors: systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2020;105:432–9.
Cole CR, Hansen NI, Higgins RD, Ziegler TR, Stoll BJ. Very low birth weight preterm infants with surgical short bowel syndrome: incidence, morbidity and mortality, and growth outcomes at 18 to 22 months. Pediatrics. 2008;122:e573–e582.
Hong CR, Fullerton BS, Mercier CE, Morrow KA, Edwards EM, Ferrelli KR, et al. Growth morbidity in extremely low birth weight survivors of necrotizing enterocolitis at discharge and two-year follow-up. J Pediatr Surg. 2018;53:1197–202.
Zozaya C, Shah J, Pierro A, Zani A, Synnes A, Lee S, et al. Neurodevelopmental and growth outcomes of extremely preterm infants with necrotizing enterocolitis or spontaneous intestinal perforation. J Pediatr Surg. 2020. May 15;S0022-3468(20)30326-2. https://doi.org/10.1016/j.jpedsurg.2020.05.013. Online ahead of print.
Sondheimer JM, Cadnapaphornchai M, Sontag M, Zerbe GO. Predicting the duration of dependence on parenteral nutrition after neonatal intestinal resection. J Pediatr. 1998;132:80–4.
Khan FA, Squires RH, Litman HJ, Balint J, Carter BA, Fisher JG, et al. Predictors of enteral autonomy in children with intestinal failure: a multicenter cohort study. J Pediatr. 2015;167:29–34.e21.
Enman MA, Wilkinson LT, Meloni KB, Shroyer MC, Jackson TF, Aban I, et al. Key determinants for achieving enteral autonomy and reduced parenteral nutrition exposure in pediatric intestinal failure. J Parenter Enteral Nutr. 2019 Dec 16. https://doi.org/10.1002/jpen.1754. Online ahead of print.
Nathan AT, Ward L, Schibler K, Moyer L, South A, Kaplan HC. A quality improvement initiative to reduce necrotizing enterocolitis across hospital systems. J Perinatol. 2018;38:742–50.
Jones KD, Howarth LJ. Intestinal failure following necrotizing enterocolitis: A clinical approach. Early Hum Dev. 2016;97:29–32.
Cole CR, Kocoshis SA. Nutrition management of infants with surgical short bowel syndrome and intestinal failure. Nutr Clin Pract. 2013;28:421–8.
Kuik SJ, Kalteren WS, Mebius MJ, Bos AF, Hulscher JBF, Kooi EMW. Predicting intestinal recovery after necrotizing enterocolitis in preterm infants. Pediatr Res. 2020;87:903–9.
Carter BA, Cohran VC, Cole CR, Corkins MR, Dimmitt RA, Duggan C, et al. Outcomes from a 12-week, open-label, multicenter clinical trial of teduglutide in pediatric short bowel syndrome. J Pediatr. 2017;181:102–111.e105.
Acknowledgements
This project was supported in part by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number 5UL1TR001425-03. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Contributions
KM designed the study, acquired, analyzed and interpreted the data, and drafted the manuscript; GG acquired and analyzed the data, and helped to write the manuscript; TJ analyzed and interpreted the data and critically revised the manuscript; AP acquired the data and critically revised the manuscript; JW, MH, and BP interpreted the data and critically revised the manuscript. All authors approve the final version to be published and agree to be accountable to all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
McNelis, K., Goddard, G., Jenkins, T. et al. Delay in achieving enteral autonomy and growth outcomes in very low birth weight infants with surgical necrotizing enterocolitis. J Perinatol 41, 150–156 (2021). https://doi.org/10.1038/s41372-020-00880-z
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-020-00880-z
This article is cited by
-
Optimal enteral feeding after surgery for necrotising enterocolitis: a systematic review
Pediatric Surgery International (2026)
-
A time series algorithm to predict surgery in neonatal necrotizing enterocolitis
BMC Medical Informatics and Decision Making (2024)
-
Body composition and bone mass among 5-year-old survivors of necrotizing enterocolitis
Pediatric Research (2023)