Abstract
Introduction
Red blood cell transfusions in infants born at ≤30 weeks gestation are frequent. Erythropoietin therapy reduces transfusions. An increase in hematocrit is an adaptive response at high altitudes but a guaranteed source of iron is necessary for adequate erythropoiesis.
Methods
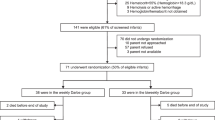
A retrospective cohort study was done to compare red blood cell transfusion practices of the 2019 EpicLatino (EPIC) Latin America network database with a single unit at 2650 m above sea level (LOCAL). The data from LOCAL for three time periods were compared over 10 years based on changes in erythropoietin dose and fewer phlebotomies. The number of cases that received transfusions and the total number of transfusions required were compared. Adjustments were made for known risk factors using a multivariate regression analysis.
Results
Two hundred and twenty-one cases in LOCAL and 382 cases from EPIC were included. Overall basic demographic characteristics were similar. In EPIC a significantly higher rate of infection (28% vs. 15%) and outborn (10% vs. 1%) was found, but less necrotizing enterocolitis (9% vs. 15%) and use of prenatal steroids (62% vs. 93%) than LOCAL (p < 0.05). EPIC patients received more transfusions (2.6 ± 3 vs. 0.6 ± 1 times) than LOCAL (p < 0.001) and received them significantly more frequently (61% vs. 25%). Within the LOCAL time periods, no statistically significant differences were found other than the need for transfusions (1st 32%, 2nd 28%, 3rd 9%, p = 0.005) and the average number of transfusions (1st 0.8 ± 1.6, 2nd 0.7 ± 1.3, 3rd 0.1 ± 0.3, p = 0.004). These differences remained significant after multivariate regression analysis and adjusting for risk variables.
Conclusion
The combination of erythropoietin, parenteral sucrose iron, fewer phlebotomies during the first 72 h, and delayed umbilical cord clamping seem to reduce red blood cell transfusion needs. This can be extremely important in high altitude units where higher hematocrit is desirable but may also be valuable at sea level.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Howarth C, Banerjee J, Aladangady N. Red blood cell transfusion in preterm infants: current evidence and controversies. Neonatology. 2018;114:7–16.
Shanmugha Priya RA, Krishnamoorthy R, Panicker VK, Ninan B. Transfusion support in preterm neonates <1500 g and/or <32 weeks in a tertiary care center: a descriptive study. Asian J Transfus Sci. 2018;12:34–41.
Ohlsson A, Aher SM. Early erythropoiesis-stimulating agents in preterm or low birth weight infants. Cochrane Database Syst Rev. 2017;11:CD004863.
Ohlsson A, Aher SM. Early erythropoiesis-stimulating agents in preterm or low birth weight infants. Cochrane Database Syst Rev. 2020;2:CD004863.
Aher SM, Ohlsson A. Late erythropoiesis-stimulating agents to prevent red blood cell transfusion in preterm or low birth weight infants. Cochrane Database Syst Rev. 2019;2:CD004868.
Juul SE, Vu PT, Comstock BA, Wadhawan R, Mayock DE, Courtney SE, et al. Effect of high-dose erythropoietin on blood transfusions in extremely low gestational age neonates: post hoc analysis of a randomized clinical trial. JAMA Pediatr. 2020;174:933–43.
Jain D, D’Ugard C, Bancalari E, Claure N. Cerebral oxygenation in preterm infants receiving transfusion. Pediatr Res. 2019;85:786–9.
Andersen CC, Karayil SM, Hodyl NA, Stark MJ. Early red cell transfusion favourably alters cerebral oxygen extraction in very preterm newborns. Arch Dis Child Fetal Neonatal Ed. 2015;100:F433–5.
Ree IMC, Lopriore E. Updates in neonatal hematology: causes, risk factors, and management of anemia and thrombocytopenia. Hematol Oncol Clin North Am. 2019;33:521–32.
Windsor JS, Rodway GW. Heights and haematology: the story of haemoglobin at altitude. Postgrad Med J. 2007;83:148–51.
Zubieta-Calleja GR, Paulev PE, Zubieta-Calleja L, Zubieta-Castillo G. Altitude adaptation through hematocrit changes. J Physiol Pharmacol. 2007;58:811–8.
Dirren H, Logman MH, Barclay DV, Freire WB. Altitude correction for hemoglobin. Eur J Clin Nutr. 1994;48:625–32.
Muckenthaler MU, Rivella S, Hentze MW, Galy B. A red carpet for iron metabolism. Cell. 2017;168:344–61.
Pollak A, Hayde M, Hayn M, Herkner K, Lombard KA, Lubec G, et al. Effect of intravenous iron supplementation on erythropoiesis in erythropoietin-treated premature infants. Pediatrics. 2001;107:78–85.
Lopriore E. Updates in red blood cell and platelet transfusions in preterm neonates. Am J Perinatol. 2019;36:S37–40.
Kaltwasser JP, Gottschalk R. Erythropoietin and iron. Kidney Int Suppl. 1999;69:S49–56.
Naude S, Clijsen S, Naulaers G, Daniels H, Vanhole C, Devlieger H. Iron supplementation in preterm infants: a study comparing the effect and tolerance of a Fe2+ and a nonionic FeIII compound. J Clin Pharmacol. 2000;40:1447–51.
Franz AR, Mihatsch WA, Sander S, Kron M, Pohlandt F. Prospective randomized trial of early versus late enteral iron supplementation in infants with a birth weight of less than 1301 grams. Pediatrics. 2000;106:700–6.
Papadopoulos M, Patel D, Korologou-Linden R, Goto E, Soondrum K, Fell JME, et al. Safety and efficacy of parenteral iron in children with inflammatory bowel disease. Br J Clin Pharmacol. 2018;84:694–9.
Auerbach M, Macdougall I. The available intravenous iron formulations: history, efficacy, and toxicology. Hemodial Int. 2017;21 Suppl 1:S83–92.
Lemyre B, Sample M, Lacaze-Masmonteil T. Canadian paediatric society FtaNC Minimizing blood loss and the need for transfusions in very premature infants. Paediatr Child Health. 2015;20:451–62.
Counsilman CE, Heeger LE, Tan R, Bekker V, Zwaginga JJ, Te Pas AB, et al. Iatrogenic blood loss in extreme preterm infants due to frequent laboratory tests and procedures. J Matern Fetal Neonatal Med. 2019:1–6.
Fogarty M, Osborn DA, Askie L, Seidler AL, Hunter K, Lui K, et al. Delayed vs early umbilical cord clamping for preterm infants: a systematic review and meta-analysis. Am J Obstet Gynecol. 2018;218:1–18.
Patel RM, Knezevic A, Shenvi N, Hinkes M, Keene S, Roback JD, et al. Association of red blood cell transfusion, anemia, and necrotizing enterocolitis in very low-birth-weight infants. JAMA. 2016;315:889–97.
Rocha G, Pereira S, Antunes-Sarmento J, Flôr-de-Lima F, Soares H, Guimarães H. Early anemia and neonatal morbidity in extremely low birth-weight preterm infants. J Matern Fetal Neonatal Med. 2019:1–7.
Aher S, Malwatkar K, Kadam S. Neonatal anemia. Semin Fetal Neonatal Med. 2008;13:239–47.
Bierer R, Peceny MC, Hartenberger CH, Ohls RK. Erythropoietin concentrations and neurodevelopmental outcome in preterm infants. Pediatrics. 2006;118:e635–40.
EpicLatino. Epiclatino repport 2019. EpicLatino; 2019. https://www.epiclatino.co/report-2019.
Pinsk V, Levy J, Moser A, Yerushalmi B, Kapelushnik J. Efficacy and safety of intravenous iron sucrose therapy in a group of children with iron deficiency anemia. Isr Med Assoc J. 2008;10:335–8.
Schröder O, Mickisch O, Seidler U, de Weerth A, Dignass AU, Herfarth H, et al. Intravenous iron sucrose versus oral iron supplementation for the treatment of iron deficiency anemia in patients with inflammatory bowel disease-a randomized, controlled, open-label, multicenter study. Am J Gastroenterol. 2005;100:2503–9.
Gredilla E, Gimeno M, Canser E, Martínez B, Pérez Ferrer A, Gilsanz F. [Postpartum and early postoperative anemia after gynecological surgery: treatment with intravenous iron]. Rev Esp Anestesiol Reanim. 2006;53:208–13.
Friel JK, Andrews WL, Hall MS, Rodway MS, Keith M, McCloy UC, et al. Intravenous iron administration to very-low-birth-weight newborns receiving total and partial parenteral nutrition. JPEN J Parenter Enter Nutr. 1995;19:114–8.
Qiao L, Tang Q, Zhu W, Zhang H, Zhu Y, Wang H. Effects of early parenteral iron combined erythropoietin in preterm infants: a randomized controlled trial. Medicine. 2017;96:e5795.
Kaneva K, Chow E, Rosenfield CG, Kelly MJ. Intravenous iron sucrose for children with iron deficiency anemia. J Pediatr Hematol Oncol. 2017;39:e259–62.
Mantadakis E. Advances in pediatric intravenous iron therapy. Pediatr Blood Cancer. 2016;63:11–6.
Cançado RD, Muñoz M. Intravenous iron therapy: how far have we come? Rev Bras Hematol Hemoter. 2011;33:461–9.
Jeon GW, Sin JB. Risk factors of transfusion in anemia of very low birth weight infants. Yonsei Med J. 2013;54:366–73.
dos Santos AM, Guinsburg R, de Almeida MF, Procianoy RS, Marba ST, Ferri WA, et al. Factors associated with red blood cell transfusions in very-low-birth-weight preterm infants in Brazilian neonatal units. BMC Pediatr. 2015;15:113.
Omar S, Salhadar A, Lorenz JM. Prenatal steroids (pns) reduce erythrocyte transfusion in very low birth weight neonates ≤1500 GM. 1396. Pediatr Res. 1996;39:235.
Madan A, Kumar R, Adams MM, Benitz WE, Geaghan SM, Widness JA. Reduction in red blood cell transfusions using a bedside analyzer in extremely low birth weight infants. J Perinatol. 2005;25:21–5.
Collard KJ. Is there a causal relationship between the receipt of blood transfusions and the development of chronic lung disease of prematurity? Med Hypotheses. 2006;66:355–64.
Auerbach M, Macdougall IC. Safety of intravenous iron formulations: facts and folklore. Blood Transfus. 2014;12:296–300.
Juul SE, Comstock BA, Wadhawan R, Mayock DE, Courtney SE, Robinson T, et al. A randomized trial of erythropoietin for neuroprotection in preterm infants. N Engl J Med. 2020;382:233–43.
Wallin DJ, Zamora TG, Alexander M, Ennis KM, Tran PV, Georgieff MK. Neonatal mouse hippocampus: phlebotomy-induced anemia diminishes and treatment with erythropoietin partially rescues mammalian target of rapamycin signaling. Pediatr Res. 2017;82:501–8.
Barks A, Fretham SJB, Georgieff MK, Tran PV. Early-life neuronal-specific iron deficiency alters the adult mouse hippocampal transcriptome. J Nutr. 2018;148:1521–8.
Sola-Visner M. Anemia in neonates EpicLatino. Proceedings of the 1st EpicLatino Virtual Meeting. 2020. https://youtu.be/wT2xJY6D6D0. www.epiclatino.com
Kling PJ. Iron nutrition, erythrocytes, and erythropoietin in the NICU: erythropoietic and neuroprotective effects. Neoreviews .2020;21:e80–e8.
Ertl R, Waldhoer T, Yang L. Moderate altitude impacts birth weight: 30 years retrospective sibling analyses using record linkage data. Pediatr Res. 2019;86:403–7.
West JB. A strategy for reducing neonatal mortality at high altitude using oxygen conditioning. J Perinatol. 2015;35:900–2.
Soria R, Julian CG, Vargas E, Moore LG, Giussani DA. Graduated effects of high-altitude hypoxia and highland ancestry on birth size. Pediatr Res. 2013;74:633–8.
Gonzales G, Salirrosas A. Arterial oxygen saturation in healthy newborns delivered at term in Cerro de Pasco (4340 m) and Lima (150 m). Reprod Biol Endocrinol. 2005;3:46.
Acknowledgements
We would like to thank EpicLatino, its board of directors, and the participating units for letting us use their data and for systematically entering the information to make it a reliable one and thus enabling this type of work. We also want to thank the people who work in the Clínica del Country unit for their dedication and fine work that made these results possible and Felipe Fajardo for his valuable input on this English paper.
Author information
Authors and Affiliations
Contributions
ABH and PVH contributed equally to this research as authors. They were involved in planning and designing the study and participated in all stages of the project. ABH was involved in data extraction. ABH and PVH analyzed the data and described the results. Together, they wrote and approved the final paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hoyos, A.B., Vasquez-Hoyos, P. Transfusion prevention using erythropoietin, parenteral sucrose iron, and fewer phlebotomies in infants born at ≤30 weeks gestation at a high altitude center: a 10-year experience. J Perinatol 41, 1403–1411 (2021). https://doi.org/10.1038/s41372-021-00945-7
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-021-00945-7