Abstract
Objective
To determine if multidisciplinary team-based care of severe BPD/CLD infants improve survival to discharge.
Design/methods
Retrospective review of severe BPD/CLD infants cared for by dedicated multidisciplinary CLD team using consensus-driven protocols and guidelines.
Results
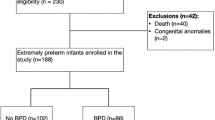
Total of 267 patients. Median gestational age was 26 weeks (IQR 24, 32); median birth-weight was 0.85 (IQR 0.64, 1.5). Twenty-four percent were preterm with severe BPD, 46% had other primary respiratory diseases (none BPD diseases). Total number of patients, proportion of patients with tracheostomy, prematurity, and genetic diagnoses increased over time. 88.8% survived to discharge. Unadjusted logistic regression showed that tracheostomy was not associated with odds of death; secondary pulmonary hypertension was associated with odds of tracheostomy (OR = 1.795 p value = 0.0264), or death (OR = 8.587 p value = <0.0001), or tracheostomy + death (OR = 13.58 p value = 0.0007).
Conclusions
Over time, mortality improved for infants with tracheostomy cared for by a multidisciplinary severe BPD/CLD team. Secondary pulmonary hypertension was associated with tracheostomy, or death, or tracheostomy + death.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Northway WH Jr., Rosan RC, Porter DY. Pulmonary disease following respiratory therapy of hyaline-membrane disease, Bronchopulmonary dysplasia. N Engl J Med. 1967;276:357–68.
Doyle LW, Anderson PJ. Long-term outcomes of bronchopulmonary dysplasia. Semin Fetal Neonatal Med. 2009;14:391–5.
Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001;163:1723–9.
Ehrenkranz RA, Walsh MC, Vohr BR, Jobe AH, Wright LL, Fanaroff AA, et al. Validation of the National Institutes of Health consensus definition of bronchopulmonary dysplasia. Pediatrics. 2005;116:1353–60.
Allen J, Zwerdling R, Ehrenkranz R, Gaultier C, Geggel R, Greenough A, et al. Statement on the care of the child with chronic lung disease of infancy and childhood. Am J Respir Crit Care Med. 2003;168:356–96.
Bapat R, Nelin L, Shepherd E, Ryshen G, Elgin A, Bartman T. A multidisciplinary quality improvement effort to reduce bronchopulmonary dysplasia incidence. J Perinatol. 2020;40:681–7.
Abman SH, Collaco JM, Shepherd EG, Keszler M, Cuecvas-Guaman M, Welty SE, et al. Interdisciplinary care of children with severe bronchopulmonary dysplasia. J Pediatr. 2018;197:300–8.
Gibbs K, Jensen E, Alexiou S, Munson D, Zhang H. Ventilation strategies in severe bronchopulmonary dysplasia. NeoReviews. 2020;21:e226–37.
Rosterman JL, Pallotto EK, Truog WE, Escobar H, Meinert KA, Holmes A, et al. The impact of neutrally adjusted ventilatory assist mode on respiratory severity score and energy expenditure in infants: a randomized crossover trial. J Perinatol. 2018;38:59–63.
McKinney RL, Keszler M, Truog WE, Norberg M, Sindelar R, Wallstrom L, et al. Multicenter experience with neutrally adjusted ventilator assist in infants with severe bronchopulmonary dysplasia. Am J Perinatol. 2020. https://doi.org/10.1055/s-0040-1708559.
Bamat NA, Kirpalani H, Feudtner C, Jensen EA, Laughon MM, Zhang H, et al. Medication use in infants with severe bronchopulmonary dysplasia admitted to United States children’s hospitals. J Perinatol. 2019;39:1291–9.
Greenberg JM, Poindexter BB, Shaw PA, Bellamy SL, Keller RL, Moore PE, et al. Respiratory medication use in extremely premature (<29 weeks) infants during initial NICU hospitalization: results from prematurity and respiratory outcomes program. Pediatr Pulmonol. 2020;55:360–8.
Overman AE, Liu M, Kurachek SC, Shreve MR, Maynard RC, Mammel MC, Moore BM. Tracheostomy for infants requiring prolonged mechanical ventilation: 10 years’ experience. Pediatrics. 2013;131:e1491–6.
Lewis CW, Carron JD, Perkins JA, Sie KCY, Feudner C. Tracheostomy in pediatric patients: a national perspective. Arch Otolaryngol Head Neck Surg. 2003;129:523–9.
Han SM, Watters KF, Hong CR, Edwards EM, Knell J, Morrow KA, et al. Tracheostomy in very low birth weight infants: a prospective multicenter study. Pediatrics. 2020;145:1–9.
Murthy K, Porta NFM, Lagatta JM, Zaniletti I, Truog W, Grover T, et al. Inter-center variation in death or tracheostomy placement in infants with severe bronchopulmonary dysplasia. J Perinatol. 2017;37:723–7.
Mandy G, Malkar M, Welty SE, Brown R, Shephard E, Gardner W, et al. Tracheostomy placement in infants with bronchopulmonary dysplasia: safety and outcomes. Pediatr Pulmonol. 2013;48:245–9.
Demauro SB, D’Agostino JA, Bann C, Bernbaum J, Gerdes M, Bell E, et al. Developmental outcomes of very preterm infants with tracheostomies. J Pediatr. 2014;164:1303–10.
Khemani E, McElhinney DB, Rhein L, Andrade O, Lacro R, Thomas K, et al. Pulmonary artery hypertension in formerly premature infants with bronchopulmonary dysplasia: clinical features and outcomes in the surfactant era. Pediatrics. 2007;120:1260–9.
Mathew R. Signaling pathways in the development of bronchopulmonary dysplasia and pulmonary hypertension. Children. 2020;7:100. https://doi.org/10.3390/children7080100.
Dh Kim, Kim HS, Choi CW, Kim EK, Kim B, Choi JH. Risk factors for pulmonary artery hypertension in preterm infants with moderate to severe bronchopulmonary dysplasia. Neonatology. 2012;101:40.
Farquhar M, Fitzgerald DA. Pulmonary hypertension in chronic neonatal lung disease. Pediatr Respir Rev. 2010;11:149.
Nyp MF, Taylor JB, Petralia A, Oschman A, Norberg M, Weatherly R, et al. Acute post-tracheostomy clinical decompensation in infants-are there predictive markers? Am J Perinatol. 2018;35:1206–12.
Gien J, Kinsella J, Thrasher J, Grenolds A, Abman S, Baker C. Retrospective analysis of an interdisciplinary ventilator care program intervention on survival of infants with ventilator-dependent bronchopulmonary dysplasia. Am J Perinatol. 2017;34:155–63.
Acknowledgements
The authors acknowledge all the members of the Chronic Lung Disease multidisciplinary team for their dedication to our BPD/CLD patients. The authors also thank the Children’s Mercy Medical Writing Center for reviewing and editing this manuscript.
Author information
Authors and Affiliations
Contributions
TPH and SK collected data with supervision from WM, MN provided the history of CLD team and the patient repository. JN-M performed statistics, figures, and tables. TPH, JN-M, and WM wrote the manuscript in consultation with MN, WT and SK.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Hansen, T.P., Noel-MacDonnell, J., Kuckelman, S. et al. A multidisciplinary chronic lung disease team in a neonatal intensive care unit is associated with increased survival to discharge of infants with tracheostomy. J Perinatol 41, 1963–1971 (2021). https://doi.org/10.1038/s41372-021-00974-2
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-021-00974-2
This article is cited by
-
Outcomes of infants and children with bronchopulmonary dysplasia-associated pulmonary hypertension who required home ventilation
Pediatric Research (2025)
-
Interdisciplinary clinical bronchopulmonary dysplasia programs: development, evolution, and maturation
Journal of Perinatology (2024)
-
The impact of early tracheostomy on neurodevelopmental outcomes of infants with severe bronchopulmonary dysplasia exposed to postnatal corticosteroids
Journal of Perinatology (2024)
-
Management pathway for infants requiring chronic care in neonatal units—a scoping review of practices
European Journal of Pediatrics (2022)